Bariatric surgery is the best method to achieve relevant weight loss that is maintained over time.1 It is not free of risks and may not be indicated for mild–moderate obesity (BMI below 35kg/m2). However, several current clinical guidelines state that surgery may be indicated in patients with grade I obesity (BMI: 30–35kg/m2), poorly controlled type 2 diabetes and increased cardiovascular risk after an individualized assessment by a multidisciplinary committee.2,3
In the last decade, intraluminal bariatric endoscopic procedures have been developed, such as the Primary Obesity Surgery Endoluminal (POSE) method. The POSE method consists of reducing the volume of the stomach, mainly at the gastric fundus, along with antral dysmotility to prolong satiety. This is done with endoscopic transmural sutures, creating plications in the fundus and in the proximal part of the antrum.4 To date, no serious complications have been described related to these endoscopic procedures, although the published series are small and long-term follow-ups are not yet available, given that these are new techniques and the published results are based on one- or 2-year patient follow-up.5,6 Many patients in whom the POSE method has failed need to later undergo a surgical bariatric procedure, and this previous manipulation of the stomach increases the risk of complications during surgery, which, despite the absence of evidence in the literature, can be expected because of the techniques involved and the previous changes made during the POSE method.
The main objective of this study is to describe the appearance of anastomotic ulcer after surgery for conversion from POSE to Roux-en-Y gastric bypass.
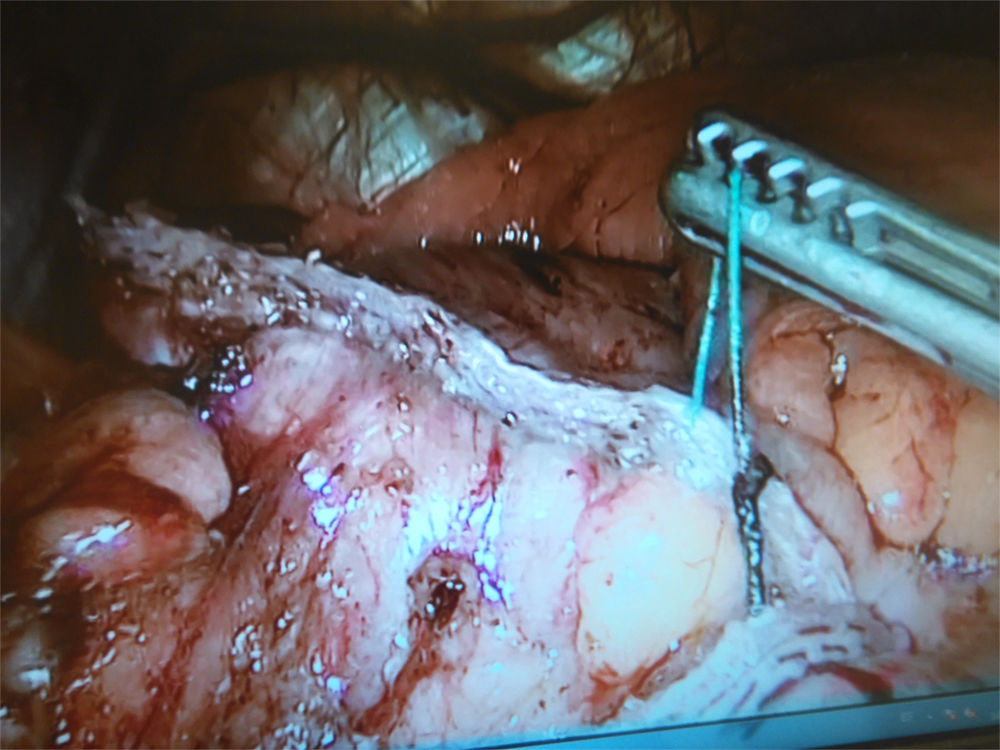
A 51-year-old woman, with a history of hypercholesterolemia and sleep apnea–hypopnea syndrome was referred to the obesity unit at our hospital, weighing 110kg with a BMI of 38kg/m2. Two years earlier, she had undergone a POSE method, after which she only managed to lose 4kg. The preoperative upper gastrointestinal endoscopy only detected changes in the gastric cavity secondary to POSE. The patient underwent laparoscopic Roux-en-Y gastric bypass, with a 60cm biliopancreatic loop and a 150cm intestinal loop. Intraoperatively, during the creation of the gastric pouch with an endostapler (Echelon Flex, Johnson & Johnson, USA), numerous suture strands from the previous POSE procedure passed through the staple line (Fig. 1), which were cut. The mechanical linear reservoir-jejunal anastomosis was completed with the endostapler (Echelon Flex, Johnson & Johnson, USA) and the opening was closed with 2/0 absorbable barbed suture (V-Loc, Medtronic, USA). The anastomosis was created without incident and the reservoir and anastomosis were checked for leaks with methylene. The patient was discharged on the 2nd day after surgery, with no postoperative events. Recommendations given at discharge included omeprazole at a dose of 20mg/day for at least 6 months.
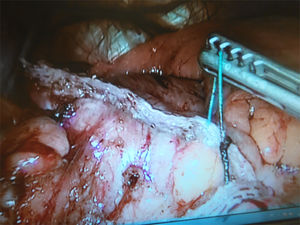
Three months after surgery, the patient came to the emergency room due to severe abdominal pain that had been progressing over the previous 48h, associated with vomiting. Abdominal CT scan showed nonspecific inflammatory changes adjacent to the reservoir-jejunal anastomosis. An upper gastrointestinal endoscopy revealed an anastomotic ulcer (Fig. 2). Treatment with omeprazole was initiated in a continuous infusion of 120mg/day/3 days, which drastically improved the pain, and the patient correctly tolerated oral intake. The patient was discharged with omeprazole 40mg/12h. A follow-up endoscopy was performed 2 months after discharge, which demonstrated complete healing of the ulcer.
Anastomotic ulcers after Roux-en-Y gastric bypass can reach an incidence of up to 7%. Most cases appear in patients with risk factors (use of tobacco, alcohol or non-steroidal anti-inflammatory drugs). Fringeli et al.7 reported its appearance in the first 6 postoperative months or one year after surgery. Following their management protocol, patients took proton pump inhibitors (PPI) only during the first postoperative month, so all of their cases occurred in patients without PPI. The main causal agent of ulcers in the gastrojejunal anastomosis is the acid secretion of the gastric reservoir and its action on the intestinal mucosa, which is not prepared for acidic secretions. Precisely for this reason, PPI are indicated in the postoperative period. However, PPI do not eliminate the risk of ulcers. Garrido et al.8 described an anastomotic ulcer rate of 7.6% in the first 2 postoperative months, despite treatment with esomeprazole and no non-steroidal anti-inflammatory drugs. These authors suggested that the ischemia at the anastomosis and the suture and stapling material used, which act as foreign bodies, are possibly causative agents as well.
The etiology of the ulcer in our patient is unclear. She had no risk factors and was taking omeprazole at the time of diagnosis of the ulcer. Given that the ulcer appeared on the anastomosis, where prior POSE suture material was cut intraoperatively, we believe that the remains of the endoluminal sutures and the ischemia associated with the stapling of the previous plication may have possibly contributed even more to the development of the ulcer. As more and more endoluminal procedures are being performed and their conversions to bariatric surgical procedures are increasing, in the future we will have data about the real incidence of this complication in these patients.
The limited evidence in the literature for weight loss results using the POSE method indicate that these are limited, providing no long-term data. Espinós et al. reported an average 6-month weight loss of 13kg, representing a percentage of excess weight lost (%EWL) of 49%.5 Lopez-Nava Breviere et al. published an average weight loss of 16.6kg per year, representing a %EWL of 44.9%.4 The American Society for Gastrointestinal Endoscopy (ASGE) recommends that bariatric endoscopic methods should achieve a %EWL of at least 25%.9 However, bariatric surgery societies require that, in order to consider a surgical procedure successful, a %EWL of at least 50% should be reached, and the final BMI should be lower than 35kg/m2. Therefore, endoscopic procedures are inferior to surgery and cannot be considered an alternative. In addition, we must bear in mind that these series also include patients with BMI below 35kg/m2, and by having less excess weight, a smaller weight loss could be considered an acceptable %EWL. Lastly, and given that these endoscopic procedures are similar to sleeve gastrectomy, there may be a similar weight gain after the 3rd year.10 However, this is uncertain as there are no results of these techniques in the mid-long term. Although the ultimate goal of both bariatric surgery and endoscopic methods is weight loss, it should possibly be considered that the population group to which the POSE method may be directed is different from candidates for bariatric surgery; thus, endoscopy would be included within the therapeutic options for patients with mild obesity, requiring less weight loss, or even for overweight patients.
Please cite this article as: Ruiz-Tovar J, González J, García A, Levano-Linares DC, Durán M. Conversión de cirugía endoscópica endoluminal primaria a bypass gástrico en Y de Roux laparoscópico. Aparición de úlcera de boca anastomótica a los 3 meses del postoperatorio. Cir Esp. 2018;96:519–521.