Femoral hernias are a common disease. However, an incarcerated femoral hernia sac containing the appendix is quite rare. We present 2 cases treated at our hospital.
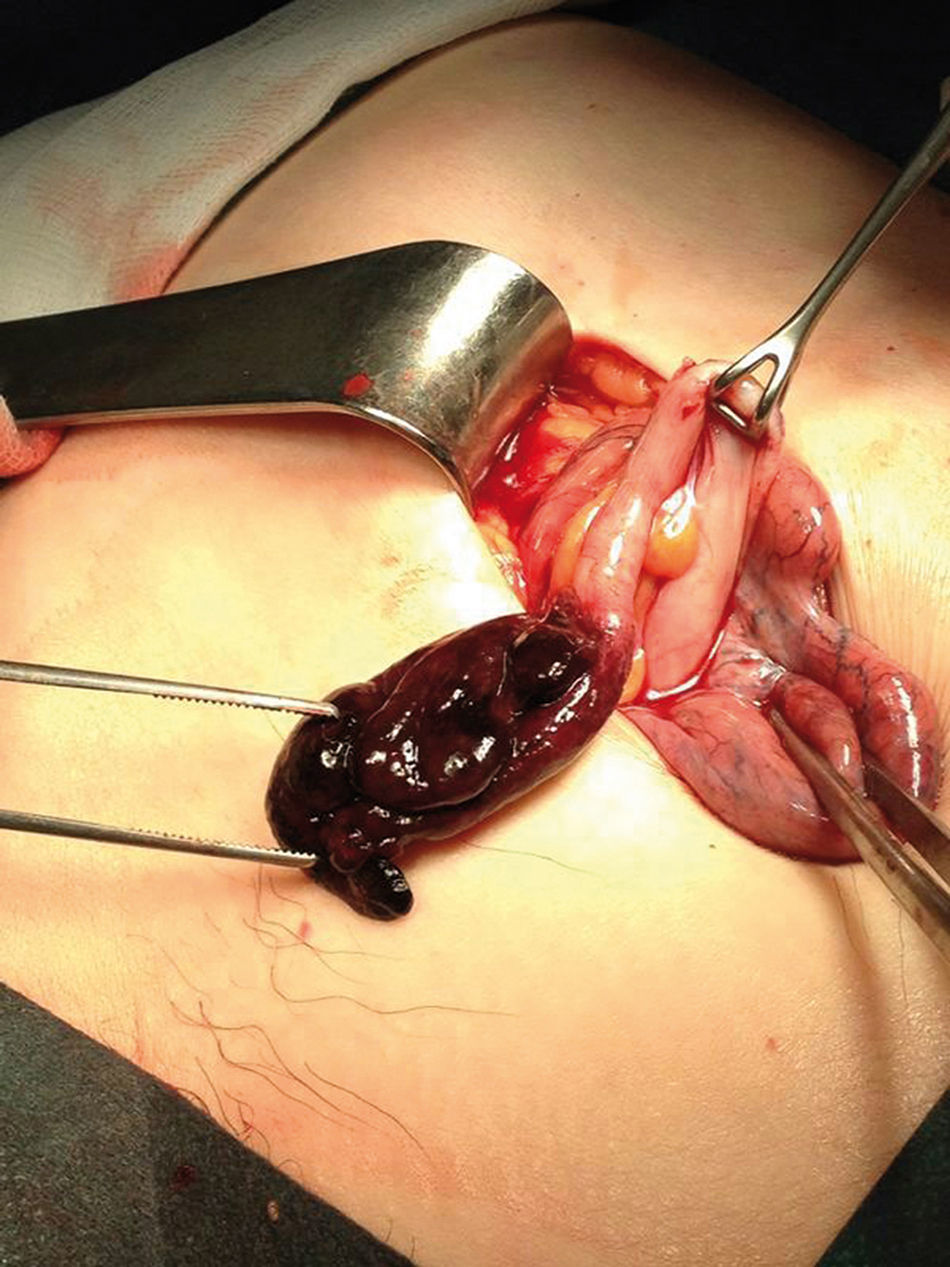
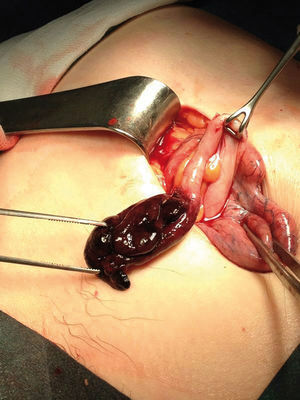
Case 1The patient is an 85-year-old woman with a history of right inguinal hernia repair, who came to the emergency room with abdominal pain. She reported diffuse abdominal discomfort and the sensation of a mass in the right groin region that had been progressing over the previous month. The patient had experienced increasing pain in the hours prior to coming to the ER, which had coincided with an increase in the size of the inguinal mass. The patient experienced nausea without vomiting or any changes in gastrointestinal transit. Upon examination, the diagnostic impression was of an incarcerated right femoral hernia, with no signs of bowel obstruction (non-distended abdomen without peritonism; abdominal radiography showing no dilatation of the small intestine). Lab work-up demonstrated elevated creatine-kinase levels (257U/L) with mild neutrophilia. We decided on urgent surgery and observed a femoral hernia that contained the vermiform appendix, which was necrotic, with a hematoma in the mesoappendix and no local signs of infection (Fig. 1). We conducted appendectomy, closure of the sac and repair of the hernia defect using a polypropylene plug. The pathology study confirmed the vermiform appendix with transmural hemorrhage.
Case 2The patient is a 38-year-old pregnant woman at 9 weeks gestation, who came to the emergency room due to abdominal pain that had been progressing over the previous 24h and a mass in the right femoral region. Upon examination, an incarcerated right femoral hernia was observed, and lab work demonstrated neutrophilia. During surgery, we observed the presence of an appendix with signs of inflammation in the herniary sac, without abscess or apparent contamination. We conducted appendectomy, closure of the sac and hernioplasty. The pathology report confirmed phlegmonous appendicitis.
In both cases, antibiotic prophylaxis was administered, and no antibiotic therapy was added post-op. The patients were discharged after 48h. During follow-up they have both been asymptomatic and have had no complications of the surgical wound.
Hernias are one of the most frequent diseases, approximately 75% appear in the inguinal region and 3% are femoral.1 The hernia sac can be empty or contain preperitoneal fat, omentum, small intestine; the colon or bladder may be found in a smaller percentage of cases. Much rarer is the presence of a portion of the circumference of the intestine (Richter), a Meckel diverticulum (Littré) or the appendix (Amyand in the inguinal regional and de Garengeot in the femoral). There is controversy in the use of these terms, as some texts consider all inguinal or femoral hernias “de Garengeot” if they contain the appendix without appendicitis. Historically, in 1735 Claudius Amyand reported the presence of a perforated appendix within an incarcerated inguinal hernia sac; and, in 1731 René-Jacques Croissant de Garengeot reported the first intervention of a femoral hernia containing the appendix without inflammation. The first appendicitis in a femoral hernia, which is even more uncommon, was treated surgically by Hevin in 1785. Thus, the appendix can be found in this type of hernias without alteration, or different grades of appendicitis or congestion due to the incarceration. The term “Amyand hernia” should be used to describe an appendix within an irreductible inguinal hernia, and “de Garengeot” should be used to describe incarceration of the appendix within a femoral sac.2
The incidence of de Garengeot hernia is estimated at 0.8%–1% of femoral hernias, mainly on the right side. Until 2009, less than 80 cases had been reported in the literature. The incidence is somewhat greater in women than in men (ratio 3:1), which is logical since femoral hernias are more frequent in this sex.3
The longest series was published in 2007, including 7 patients over a period of 16 years.4 The mean age at presentation was 55 years, with an age range from 35 to 89. The most frequent presentation was the presence of a painful femoral mass (100% of patients), with associated abdominal pain in only 14%. At diagnosis, the mean number of days since presentation was 5.2 (range: 2.5–21 days), and no patients presented signs of dilatation of the small intestine on abdominal radiograph or leukocytosis. Most studies showed forms of presentation that had evolved over a few hours or days, as in our second patient. Nonetheless, although the most common form is acute, patients may also report nonspecific chronic symptoms. This is more frequent in older patients, who report vague abdominal discomfort, as in our first case, or the masses may be confused with lymphadenopathies as they progress over several days, with no associated peritonism or signs of obstruction on simple abdominal radiography.5
Diagnosis is usually intraoperative, since the observation of an incarcerated femoral hernia during examination indicates the need for urgent surgery. The only cases of preoperative diagnosis occur in cases with uncertain diagnosis, requiring ultrasound or abdominal CT.6
Treatment is urgent surgery. Given the rarity of these cases, no guidelines have been established. Most articles recommend hernia repair after reducing the appendix when it shows no necrosis or inflammation, or rather herniorraphy in cases where appendectomy is required. Nonetheless, there have been numerous articles published about the use of prosthetic material in incarcerated inguinal hernias requiring bowel resection,7 and this could be extrapolated to de Garengeot hernias. Another alternative would be the laparoscopic approach,3 including laparoscopic appendectomy with hernia repair by means of the transabdominal preperitoneal (TAPP) technique,8 totally extraperitoneal (TEP) procedure9 or open surgery (these latter 2 options have the advantage of mesh placement without opening the peritoneum, thereby separating the prosthesis from any contamination). Last of all, there have been descriptions of appendectomy with hernia repair in a second procedure.10 Thus, treatment is adjusted to each specific case and experience of the surgeon.
FundingNo funding or grants were received for the completion of this article.
AuthorshipNatalia González Alcolea and José Luis Lucena de la Poza: data collection and composition of the article.
Félix Martínez Arrieta, Elena Jiménez Cubedo and Víctor Sánchez Turrión: data collection, critical review and approval of the final version.
Please cite this article as: González Alcolea N, Martínez Arrieta F, Lucena de la Poza JL, Jiménez Cubedo E, Sánchez Turrión V. Hernia de Garengeot: hernia crural incarcerada conteniendo el apéndice. Revisión de la literatura a propósito de 2 casos. Cir Esp. 2017;95:177–178.