The aim of this study was to determine factors associated with a prolonged postoperative stay (PS) in patients operated on with bowel resection for Crohn's disease (CD) included in an enhanced recovery program (ERP).
MethodsWe included patients operated on for CD between January 2013 and December 2015. ERP was organized following an 8-point protocol. Variables studied were: age, sex, PS, ASA, location and type of CD, presence of perianal disease, Harvey–Bradshaw index, previous resection, type of surgery (minimally invasive vs laparotomy) and Clavien Dindo. An inferential study was performed to identify factors related with a PS>6 days and multivariate analysis.
ResultsA total of 52 patients were operated on. The median PS was 8 days (IR: 5–11). In the univariate analysis, location (L1 vs L2–3), type (B2 vs B3), presence of perianal disease, prior surgery, type of surgery performed, Harvey–Bradshaw index and Clavien-Dindo were associated with a PS > or < 6 days. The model that best adjusts to predict a PS>6days contained the variable Harvey–Bradshaw (OR: 6.49; 95% CI: 1.46–28.8) and the type of surgery (OR: 0.23; 95% CI: 0.05–0.95).
ConclusionA prolonged postoperative stay after bowel resection for CD is more related to the type or severity of the disease and the type of surgery performed, than with other patient factors. Patients with CD need good coordination between prehabilitation, ERP and postoperative management.
Los objetivos del trabajo fueron determinar los factores asociados a una estancia postoperatoria (EP) prolongada en pacientes con resección intestinal por enfermedad de Crohn (EC) con un protocolo de rehabilitación multimodal (RM).
MétodosSe incluyó a los pacientes intervenidos entre enero de 2013 y diciembre de 2015 por EC. Para la RM se siguió un protocolo de 8 puntos. Las variables estudiadas fueron: edad, sexo, EP, ASA, localización y patrón de la EC, presencia de enfermedad perianal, índice de Harvey-Bradshaw, resección previa, tipo de cirugía actual (mínimamente invasiva vs laparotomía) y Clavien-Dindo. Se realizó un estudio inferencial para identificar los factores asociados a una EP>de 6 días y un modelo logístico multivariante.
ResultadosSe intervino a 52 pacientes. La EP mediana fue de 8 días (RI: 5-11). En el análisis univariante, la localización (L1 vs L2-3), el patrón (B2 vs B3), la existencia de enfermedad perianal, la cirugía previa, el tipo de cirugía realizada, el Harvey-Bradshaw y el grado de Clavien-Dindo se asociaron todos ellos con una EP inferior o superior a 6 días. El modelo parsimonioso que mejor ajusta para predecir una EP > 6 días es el que contiene la variable Harvey-Bradshaw (OR: 6,49; IC 95%: 1,46-28,8) y el tipo de cirugía efectuado (OR: 0,23; IC 95%: 0,05-0,95).
ConclusionesLa estancia prolongada tras cirugía resectiva por EC se relaciona más con el tipo o gravedad de la enfermedad y de cirugía realizada que con otras características del paciente. Los pacientes con EC requieren una buena coordinación entre prehabilitación, RM y transferencia de cuidados postoperatorios.
The application of a series of perioperative measures, mainly in randomized studies, that are known as “fast-track surgery” (FTS), “enhanced recovery after surgery” (ERAS) or, in Spanish, programa de recuperación intensificada (PRI), which are used to reduce stress (and its response) caused by major surgery, has profoundly changed the practice of perioperative medicine in the last 10 years.1
After individual patient needs and risks have been recognized, FTS combines a series of elements that are initiated at the moment of surgical indication to optimize treatment before (prehabilitation), during and after surgery. The application and standardization of an FTS protocol requires close collaboration of all the specialists who participate in the process as well as the active participation of the patient and family members.
The FTS protocol has been applied to a good number of surgical processes, and the published results have shown a lower incidence of medical complications, shorter hospitalizations and the consequent reduction in costs, which improve the overall efficiency of the healthcare system, while hospital readmission rates remain acceptable. Initially proposed for a series of selected patients, the growing demand for major surgery in high-risk patients requires new improvements that should focus on the specific evidence per procedure.
Little is known about the results of an FTS program applied to patients with inflammatory bowel disease (IBD) requiring major surgery.2,3 Patients with Crohn's disease (CD) who are candidates for surgery are a special group as they are predominantly young, with long-term and weakening symptoms that are refractory to medical treatment. They may also have irreversible damage to intestinal structures, complex clinical presentations with abscesses, fistulae or inflammatory mass, and their condition may be aggravated by anemia, iron deficiency, pharmacological immunosuppression and malnutrition.4 In spite of this (or perhaps due to this), it is important to optimize the perioperative management of these patients, which are part of some of the measures included in FTS protocols.
The aim of this present study was to analyze the factors associated with prolonged postoperative stay (as a substitute datum for results of an FTS protocol) in patients who had been treated surgically for gastrointestinal CD (excluding isolated proctological surgery).
MethodsIncluded in the study were all patients with CD who required scheduled major abdominal surgery (for gastrointestinal stenosis or resection) between January 2013 and December 2015. Patient records were used, which had been collected prospectively and consecutively from an activity database of the Colorectal Surgery Unit at the hospital. The records contained a specific section for IBD, and we complemented the search with the database of hospitalization episodes. Excluded from the study were cases of urgent or semi-urgent surgery, isolated anal surgery or stoma-closure surgery.
The majority of the cases were assessed preoperatively by a multidisciplinary IBD team (surgeons, gastroenterologists and radiologists). The perioperative care protocol was, in general terms, the same as that used for other types of colorectal surgery; nonetheless, measures were applied to reduce preoperative sepsis (previous aspiration of intraabdominal, pelvic or retroperitoneal abscesses). Intensive treatment was also administered with enteral or parenteral nutrition for preoperative malnutrition (BMI less than 18kg/m2, weight loss greater than 10% in the last 6 months or serum albumin levels lower than 3g/dL) and iron deficiency was corrected if possible. As for preoperative medication, biopharmaceuticals or immunosuppressants were not suspended preoperatively (except in patients with prior sepsis, in whom treatment was withdrawn one week before surgery). However, steroid doses were suspended or reduced to the minimum dose possible once the surgical indication had been determined.
For perioperative care, an 8-point FTS protocol was followed: fast of 6h for solids and 2h for clear liquids with supplement of carbonated drink, prophylaxis of postoperative nausea and vomiting, balanced anesthesia, minimally invasive surgery (MIS), multimodal analgesia without morphine derivatives (preoperative gabapentin, local anesthesia and NSAIDS postoperatively), restrictive fluid therapy, early oral intake (the morning after the procedure intervention) and scheduled mobilization (with specific objectives).
The variables studied were: age at the time of surgery, sex, year of surgery, hospital stay in days, ASA grade, current location of CD, current pattern of CD, presence or history of perianal disease, Harvey–Bradshaw activity index5 (clinical data from anamnesis and physical exploration collected at the time of surgical indication), previous abdominal surgery, type of current surgery (MIS vs laparotomy) and degree of postoperative complications (Clavien-Dindo6).
MIS was classified as single-port or multi-port laparoscopic surgery, in which assistance laparotomy (transumbilical or Pfannenstiel, respectively) was done exclusively to resect the bowel mesentery or conduct extracorporeal anastomosis, after the intracorporeal mobilization of the segment to be resected (or segments for strictureplasty). A single-port approach was preferentially selected for ileocecal resection due to distal stenosis, while a multi-port laparoscopy was preferred in the cases associated with inflammatory mass or fistulae. In cases requiring laparotomy from the onset, this was done on the midline.
Statistical AnalysisThe results were analyzed by the Clinical Epidemiology department of the hospital, using STATA software (StataCorp. 2013 StataStatistical Software: Release 14.1. CollegeStation, TX: StataCorp LP).
The statistical data are reported as most appropriate, given the nature and scale of measurement for each variable: absolute and relative frequencies in percentage, and means and standard deviation for continuous variables, or median and interquartile range if required by the data distribution.
In the first stage, a univariate analysis was used of the possible risk factors associated with prolonged hospitalization (>6 days), both quantitatively and categorically, in order to identify the variables that have statistical significance, using the Student's t test (Mann–Whitney U) or Pearson's χ2 (Fisher test). Those that showed a level of significance under 0.20 were entered in a multivariate stepwise logistic model, retaining the variables that were independently and significantly associated with a hospital stay >6 days.
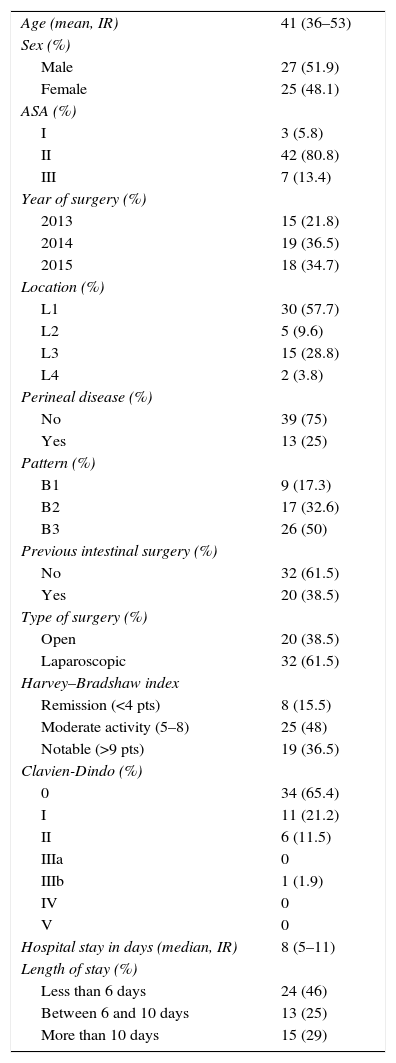
ResultsA total of 52 patients were treated, with a mean age of 41 (IR 36–53); 48% were women. Table 1 shows the data related to the variables studied. The median hospital stay was 8 days (IR: 5–11); 46% of the patients had a hospital stay equal to or less than 6 days, 25% from 6 to 10 days and 29% >10 days. The location of the current disease was ileal in 58%, and 50% of the patients had disease with a perforating pattern. Some 38% of the patients presented a history of prior bowel surgery for CD, although 62% of the series was treated with MIS techniques. One patient required reoperation due to anastomotic dehiscence, involving resection and re-anastomosis, without stoma or further postoperative incidences (2% Clavien-Dindo IIIb).
Data of the Study Cohort (No.=52).
| Age (mean, IR) | 41 (36–53) |
| Sex (%) | |
| Male | 27 (51.9) |
| Female | 25 (48.1) |
| ASA (%) | |
| I | 3 (5.8) |
| II | 42 (80.8) |
| III | 7 (13.4) |
| Year of surgery (%) | |
| 2013 | 15 (21.8) |
| 2014 | 19 (36.5) |
| 2015 | 18 (34.7) |
| Location (%) | |
| L1 | 30 (57.7) |
| L2 | 5 (9.6) |
| L3 | 15 (28.8) |
| L4 | 2 (3.8) |
| Perineal disease (%) | |
| No | 39 (75) |
| Yes | 13 (25) |
| Pattern (%) | |
| B1 | 9 (17.3) |
| B2 | 17 (32.6) |
| B3 | 26 (50) |
| Previous intestinal surgery (%) | |
| No | 32 (61.5) |
| Yes | 20 (38.5) |
| Type of surgery (%) | |
| Open | 20 (38.5) |
| Laparoscopic | 32 (61.5) |
| Harvey–Bradshaw index | |
| Remission (<4 pts) | 8 (15.5) |
| Moderate activity (5–8) | 25 (48) |
| Notable (>9 pts) | 19 (36.5) |
| Clavien-Dindo (%) | |
| 0 | 34 (65.4) |
| I | 11 (21.2) |
| II | 6 (11.5) |
| IIIa | 0 |
| IIIb | 1 (1.9) |
| IV | 0 |
| V | 0 |
| Hospital stay in days (median, IR) | 8 (5–11) |
| Length of stay (%) | |
| Less than 6 days | 24 (46) |
| Between 6 and 10 days | 13 (25) |
| More than 10 days | 15 (29) |
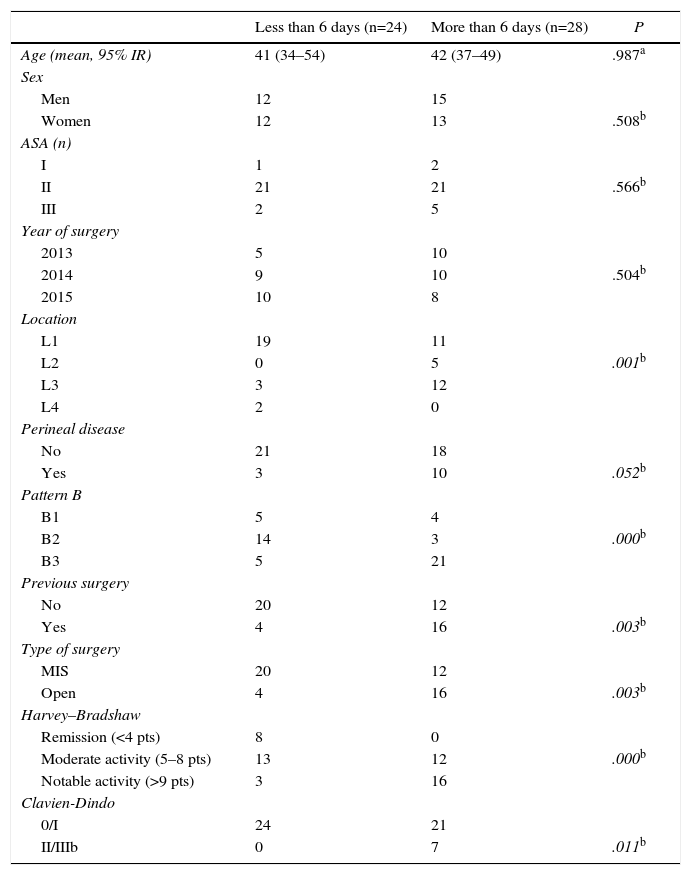
Table 2 demonstrates the results of the univariate analysis comparing the patients with a hospital stay longer or shorter than 6 days. We have observed that the location of the disease (L1 vs L2–3), pattern (B2 vs B3), existence of perianal disease, prior abdominal surgery, type of surgery performed (MIS vs laparotomy), Harvey–Bradshaw activity index (above or below 9 points) and the Clavien-Dindo grade (0–1 vs II/III) were associated with the hospitalization duration being shorter or longer than 6 days, respectively.
Univariate Study (Postoperative Hospital Stay Longer or Shorter Than 6 Days).
| Less than 6 days (n=24) | More than 6 days (n=28) | P | |
|---|---|---|---|
| Age (mean, 95% IR) | 41 (34–54) | 42 (37–49) | .987a |
| Sex | |||
| Men | 12 | 15 | |
| Women | 12 | 13 | .508b |
| ASA (n) | |||
| I | 1 | 2 | |
| II | 21 | 21 | .566b |
| III | 2 | 5 | |
| Year of surgery | |||
| 2013 | 5 | 10 | |
| 2014 | 9 | 10 | .504b |
| 2015 | 10 | 8 | |
| Location | |||
| L1 | 19 | 11 | |
| L2 | 0 | 5 | .001b |
| L3 | 3 | 12 | |
| L4 | 2 | 0 | |
| Perineal disease | |||
| No | 21 | 18 | |
| Yes | 3 | 10 | .052b |
| Pattern B | |||
| B1 | 5 | 4 | |
| B2 | 14 | 3 | .000b |
| B3 | 5 | 21 | |
| Previous surgery | |||
| No | 20 | 12 | |
| Yes | 4 | 16 | .003b |
| Type of surgery | |||
| MIS | 20 | 12 | |
| Open | 4 | 16 | .003b |
| Harvey–Bradshaw | |||
| Remission (<4 pts) | 8 | 0 | |
| Moderate activity (5–8 pts) | 13 | 12 | .000b |
| Notable activity (>9 pts) | 3 | 16 | |
| Clavien-Dindo | |||
| 0/I | 24 | 21 | |
| II/IIIb | 0 | 7 | .011b |
With the limited number of cases and the relatively high number of categories per variable, the parsimonious model that best adjusts to this situation contains the modified Harvey–Bradshaw variable as dichotomic (higher or lower than 9 points of activity) and the type of surgery conducted (MIS vs laparotomy). A Harvey–Bradshaw greater than 9 points has an OR of 6.49 (95% CI: 1.46–28.8) for a hospital stay of more than 6 days, and laparotomy has 4 times more risk for hospitalization longer than 6 days than MIS (OR 0.23; 95% CI: 0.05–0.95).
DiscussionThe median hospital stay obtained in this series (8 days; IR 5–11) is greater than expected and also somewhat more prolonged (1–2 days more) than that obtained after scheduled surgery for colorectal cancer in our own hospital.
As expected, the patients with an elevated rate of preoperative clinical activity (more symptomatic or ill), with more complex disease (fistulizing or perforating pattern) and more invasive surgery (prior interventions, need for open approach), had a longer hospitalization, which demonstrates that this parameter has more to do with the characteristics of the disease than with the type of patient. In the series that we present, a score greater than 9 points in the Harvey–Bradshaw scale and the open surgery type were the 2 variables that were statistically associated with a higher risk for hospitalization longer than 6 days.
Some variables, such as age or ASA, typically associated with prolonged hospitalization in most surgical processes, have no application in this group of patients, who are generally young and without severe systemic diseases (87% were ASA I or II). Likewise, the low rate of complications (85% were Clavien-Dindo 0 or I, and only 2% grade IIIb) diminished the statistical value of this variable that is also generally associated with prolonged hospitalization. Other studies have indicated the advantages of laparoscopic surgery in the surgical treatment of CD7 and in the series that we present almost 2/3 of the patients were treated with MIS; nevertheless, its utilization is related with previous surgical history and the existence of an inflammatory-perforating pattern or complex intraabdominal disease.8
Recently, the measurement of C-reactive protein (CRP) levels has been introduced in clinical practice during the postoperative period as a predictive measurement for postoperative complications, which promotes early hospital discharge in cases that present a drop in reference levels. Patients with CD that is not strictly fibrostenotic present elevated levels of preoperative CRP, and their decreasing pattern during the postoperative period could be different or more gradual than in cases without IBD. In the series presented, these levels were not routinely measured, so we do not have data in this regard. A study about risk factors for postoperative septic complications after resection with anastomosis due to CD found that preoperative CRP levels >10mg/L or rather an ascending preoperative pattern were associated with an increase in postoperative intraabdominal complications.9 More studies are required to confirm the predictive value for postsurgical complications of pre- and postoperative CRP levels in cases of CD.
The ambispective nature of this study does not allow us to assess the importance of the previous correction of frequent preoperative problems presented by patients with CD and their influence on hospital stay. These include the treatment of intraabdominal abscesses by means of percutaneous drainage prior to the intervention, the correction of anemia or iron deficiency (common in these patients), or the need for nutrition (enteral or parenteral) prior to surgery. Our study only registered hospital stay, and many of these measures are done when patients are hospitalized, either by the gastroenterology or surgery departments. In any event, these optimization measures, which are effective for reducing postoperative morbidity (especially infections and anastomotic complications),4,10 follow the recommendations of FTS guidelines for surgical prehabilitation.
The transverse medical–surgical approach for this disease, headed by a multidisciplinary team, together with the optimization of the surgical scenario by the application of an FTS program, should ensure the conceptual framework and perioperative management of CD. Fig. 1 presents a diagram of the optimization of the perioperative period in association with FTS protocols for patients with IBD in general and CD in particular.11
Modified from De Oca11: perioperative optimization associated with the FTS protocol for IBD. MIS: minimally invasive surgery; IBD: inflammatory bowel disease; FTS: fast-track surgery; MDT: multidisciplinary team; SP: surgical process.
The main weakness of this present study is that, although mobilization from the first day, restrictive fluid therapy, multimodal analgesia and the early initiation of oral intake were the norm in all patients, the 8 points of the FTS protocol were not applied in all cases. There was also no precise record of the causes for non-implementation or quality control of preoperative information (degree of comprehension) in relation to the FTS protocol. Some patients prefer not to be woken early to drink the prescribed carbonated beverage; in other instances, it is necessary to modify the preoperative medication (gabapentin, dexamethasone, etc.) for different justified reasons, but the specific causes for incompliance were not recorded for all points and, therefore, we cannot analyze its influence on the result of the program. Given the nature of this study, another aspect that is difficult to clarify is whether the higher or lower degree of compliance of the FTS protocol was due to the variables selected and studied or to others that were not collected in the present study, such as socio-familiar factors or specific symptoms (long-term bowel obstruction with notable loop dilatation, use or not of simultaneous stoma, etc.).
Patients with CD who require surgery also need information that is related to the nature of their disease (treatment alternatives, expectations after surgery and possible complications) as well as specific information about the surgical process. Active collaboration is also necessary during post-op, which is a fundamental aspect recognized in FTS protocols. The existence of specific liaison nursing staff for IBD is important for rapid and correct transfer of patients between the gastroenterology unit and surgery, for reestablishing/modifying medication, and for coordinating any studies that are required. However, without specific training, this is insufficient as a substitute for information of the surgical process, as in our series.
To conclude, CD is not an impediment for implementing FTS protocols that are preferably associated with MIS. Nonetheless, unlike other surgical processes, prolonged hospitalization is more due to the type of disease than due to other patient factors, which require a tailored program. Patients with IBD, and particularly CD, require 2 types of complementary measures: first of all, a specific preoperative optimization program to treat the complications frequently observed prior to surgery (requiring a multidisciplinary approach among radiologists, gastroenterologists and surgeons dedicated to this disease); and second, a program of perioperative FTS measures, with special attention given to the transference of care.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Enriquez-Navascués JM, Elorza G, Placer C, Timoteo A, Velaz L, Borda N, et al. Rehabilitación multimodal y cirugía intestinal por enfermedad de Crohn: Factores asociados a estancia hospitalaria prolongada. Cir Esp. 2016;94:531–536.
This study has been presented at the 20th National Meeting of the Spanish Association of Coloproctology and the Coloproctology Division of the AEC, in Elche, Spain, May 18–20, 2016.