Pneumomediastinum is a rare clinical entity characterized by the presence of air in the mediastinum. Its secondary iatrogenic origin due to a minor dental process is extremely rare and requires a high rate of suspicion for diagnosis.
We present the clinical case of a 67-year-old patient, with no medical history of interest, who came to the Emergency Department 8 h after having a dental filling procedure of the first and second lower left premolars. The patient described that, during the polishing phase of the procedure (performed with rotary instruments that dispense air and water), the patient experienced the abrupt onset of pressure in the left hemifacial region. Her odontologist observed edema of the surrounding mucosa, with increased volume of the soft tissue to the ipsilateral periobital area. Given the suspected diagnosis of an allergic reaction secondary to the local anesthetic, the patient was immediately administered corticosteroid treatment. However, the patient reported progressive worsening and onset of oppression in the cervicothoracic region, at which time she was referred from the dental clinic to our medical center.
Upon arrival, the patient was hemodynamically stable, afebrile, eupneic, with an SpO2 of 96%. On physical examination, we observed subcutaneous emphysema in the facial and cervical regions. Exploration of the oral cavity showed no notable alterations. On pulmonary auscultation, vesicular murmur was preserved; on cardiac auscultation, crackles were synchronous with the heartbeat in the precordial region (Hamman's sign).
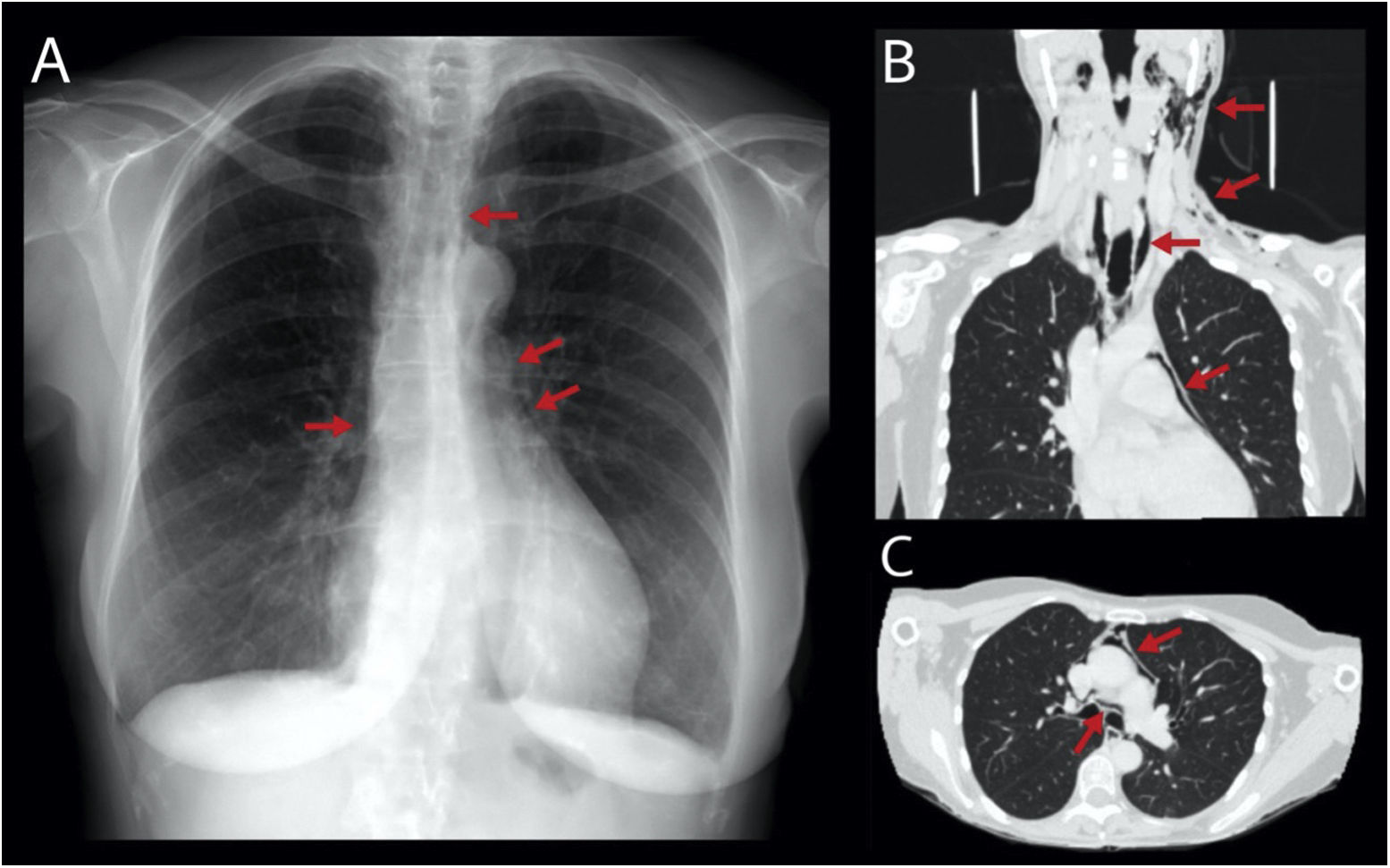
Chest X-ray confirmed the diagnostic impression of pneumomediastinum (Fig. 1A). Another secondary etiology of the pneumomediastinum was ruled out by cervical-thoracic CT scan, which demonstrated the presence of subcutaneous emphysema in the facial and bilateral cervical regions with intrathoracic extension and pneumomediastinum, but no other associated lesions (Fig. 1B/C). As the patient had no associated history of trauma injuries nor any other endoscopic/surgical procedure, and given the low etiological suspicion of any esophageal, airway or pulmonary lesions, we ruled out further diagnostic studies.
The patient was admitted to monitor the progression of her symptoms and condition, administering empirical analgesic and antibiotic treatment. She was discharged 72 h after presenting favorable evolution, ruling out infectious complications.
The use of dental rotary instruments that produce pressurized air are known risk factors for the appearance of secondary pneumomediastinum.1 Although any tooth could be involved, the molars are the most frequently affected as they have a closer relationship with the deep spaces of the head and neck.2
Proper patient anamnesis and physical examination are essential to establish a correct diagnosis and rule out other causes of secondary pneumomediastinum.
As described in other case reports,3 treatment of pneumomediastinum associated with dental procedures can be conservative, with gradual resorption and favorable evolution. Empirical antibiotic therapy is recommended as a preventive measure against potential infectious complications caused by the migration of oral flora into the subcutaneous tissue and mediastinum through the injured oral mucosa, resulting in cellulitis or the development of mediastinitis.
This case report presents limitations inherent to its format and the low incidence of this complication, as we describe the symptoms and evolution of only one patient. Despite this, given the possibility of the appearance of this iatrogenic complication and given its potential seriousness, it is necessary for all healthcare professionals who perform dental procedures to be aware of this pathology.
In conclusion, the appearance of subcutaneous emphysema and/or chest tightness in a patient during or after performing a dental procedure should be considered a sign of alarm. The procedure should be terminated and the patient referred to a hospital for diagnostic-therapeutic management.