Bile duct stenosis in the hepatic hilum is generally secondary to malignant lesions, although a small proportion is due to benign processes. This can sometimes make for a difficult preoperative differential diagnosis.
Hepatolithiasis is defined as the presence of calculi located proximally to the confluence of the left and right bile ducts. This disease is endemic in the Asia-Pacific regions, where its prevalence can reach 30%–50%,1 but it still remains a rare disease in Western countries, where it does not exceed 2%.2
Both entities are related, and intrahepatic lithiasis is considered a risk factor for the development of cholangiocarcinoma.3,4
We report the case of a 63-year-old woman who had undergone cholecystectomy 20 years earlier. She was referred to our consultation due to hepatic profile alterations found on a routine analysis: gamma glutamyl transpeptidase 371U/L (4–40U/L), aspartate aminotransferase 62U/L (0–35U/l), alanine aminotransferase 145U/L (0–35U/L), alkaline phosphatase 264U/L (40–140U/L) and total bilirubin 0.96mg/dl (0.3–1.4mg/dl).
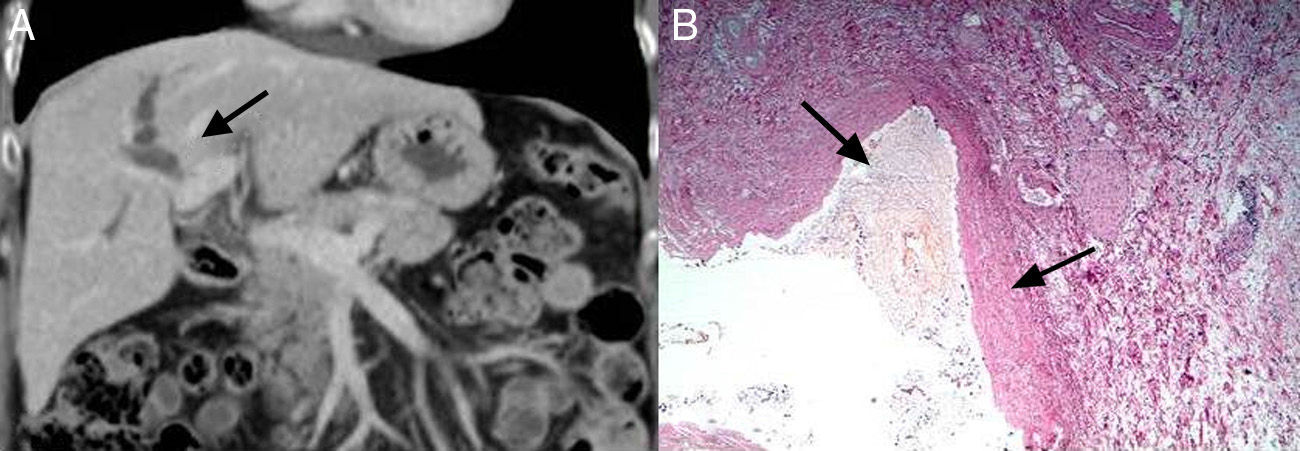
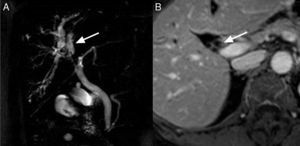
Abdominal ultrasound demonstrated a dilated right intrahepatic bile duct, although the cause was not able to be identified. Magnetic resonance cholangiography showed a dilated right bile duct with impaired signal in segment 8 at the right bile duct bifurcation, with contrast enhancement and thickening in the bile duct wall (Fig. 1A and B). Given the suspicion of cholangiocarcinoma, the patient was referred to our center. We continued the study by ordering computed tomography (CT) with three-phase multidetector liver study, which demonstrated dilatation of the right intrahepatic bile duct with a change in gauge of the right duct in the bifurcation of the right and left portal branches, with no clearly observed masses or lesions that would justify the stenosis (Fig. 2A). Tumor marker levels (CEA and CA 19.9) were within normal ranges.
(A) Computed tomography image showing dilatation of the right hepatic duct with a change in size at the bifurcation of the portal vein; (B) histology of the surgical specimen with hematoxylin/eosin stain (10×) showing a whitish calculus formation and fibrotic thickening of the bile duct wall. The epithelium presents areas of erosion, with no observed signs of histologic malignancy.
Due to the radiological findings and not being able to rule out cholangiocarcinoma, we decided to consider the process malignant and scheduled surgery for a radical oncologic resection. The procedure entailed right hepatic trisectionectomy with inclusion of segment 1, resection of the extrahepatic bile duct and lymphadenectomy of the hilar pedicle. Total liver volume was 1310 cc with a calculated remainder (left lateral segment) of 270 cc (21%). With this limited remnant, right percutaneous portal and segment 4 embolizations were used, after which an increased residual liver volume of 30% was achieved in the fourth week after the procedure.
During surgery, intraoperative ultrasonography was performed, showing only evidence of the right bile duct dilatation, with good portal flow and no nodular lesions. The planned surgical technique was performed and a sample from the left bile duct margin was sent for intraoperative biopsy, the result of which was absence of malignancy. The reconstruction of biliary continuity was performed with a Roux-en-Y hepaticojejunostomy. The operative time was 325min and did not require blood transfusion.
The patient presented no complications during the postoperative period and was discharged on the 6th postoperative day.
The macroscopic examination of the surgical specimen revealed the presence of 2 whitish calculus formations that were hard in consistency and completely obstructed the biliary lumen, with wall thickening. The microscopic study of the right hepatic duct demonstrated fibrous thickening of the wall with areas of erosion in the epithelium and no signs of malignancy (Fig. 2B).
CommentsPrimary hepatolithiasis is also known in far eastern countries as recurrent pyogenic cholangitis and oriental colangiohepatitis.5 It is a rare disease in our setting and generally does not present a difficult differential diagnosis with malignant lesions. Its pathogenesis is not entirely clear, but close relationships and associations have been seen with nutritional status, parasitic diseases, bacterial infection, bile stasis caused by postoperative stenosis, sclerosing cholangitis, Caroli's disease or neoplasms.2
There is a higher incidence of hepatolithiasis between the fifth and sixth decades of life.6
For diagnosis, noninvasive techniques such as ultrasound, magnetic resonance cholangiography and computed tomography are quite helpful and, in most cases, reveal intraluminal calculi. Nonetheless, direct cholangiography remains the gold standard for the location of anomalies within the ducts and the detection of small calculi.7 In the present case, preoperative imaging tests could not identify the presence of intraductal stones which, together with the contrast enhancement of the biliary wall, led us to the erroneous preoperative diagnosis of hilar cholangiocarcinoma. All the series of resected hilar cholangiocarcinomas reported 5%–15% false positives or pseudo Klatskin.8 Current recommendations lean toward surgical resection without the need for histologic confirmation9,10 because of the low morbidity and mortality of liver resections in experienced centers and the benefit obtained for patients in cases of pathologic confirmation of malignant process.
Please cite this article as: Vergara Suárez F, López Andújar R, Montalvá Orón E, Ramírez Ribelles C, Pérez Rojas J. Hepatolitiasis simulando un colangiocarcinoma hiliar. Cir Esp. 2013;91:535–537.