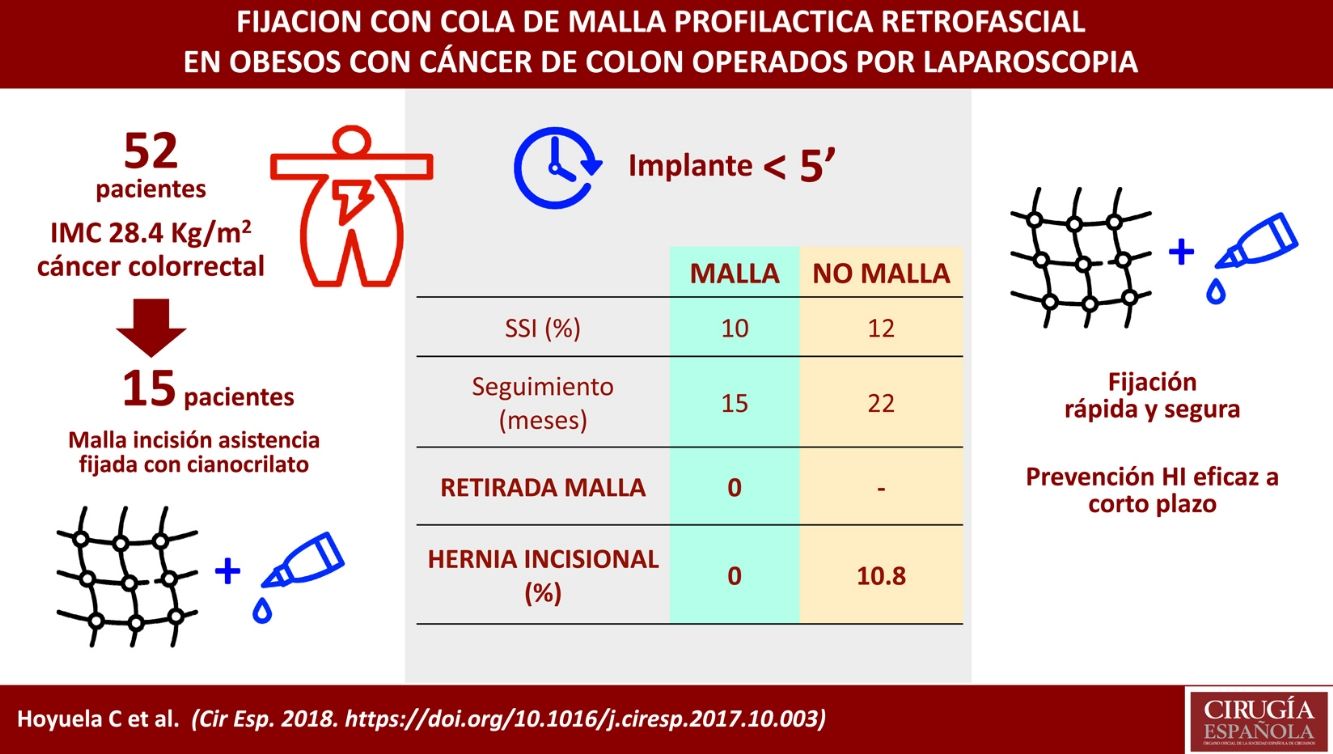
The rate of incisional hernia in high-risk patients (obesity, cancer, etc.) is high, even in laparoscopic surgery. The aim of this study is to evaluate the safety of the use of cyanoacrylate fixed prophylactic meshes in the assistance incision in overweight or obese patients undergoing laparoscopic colorectal surgery.
MethodsA prospective, non-randomized cohort study of patients undergoing elective laparoscopic resection for colorectal cancer between January 2013 and March 2016 was performed. Those with a body mass index greater than 25kg/m2 were evaluated to implant a prophylactic meshes fixed with cyanoacrylate (Histoacryl®) as reinforcement of the assistance incision.
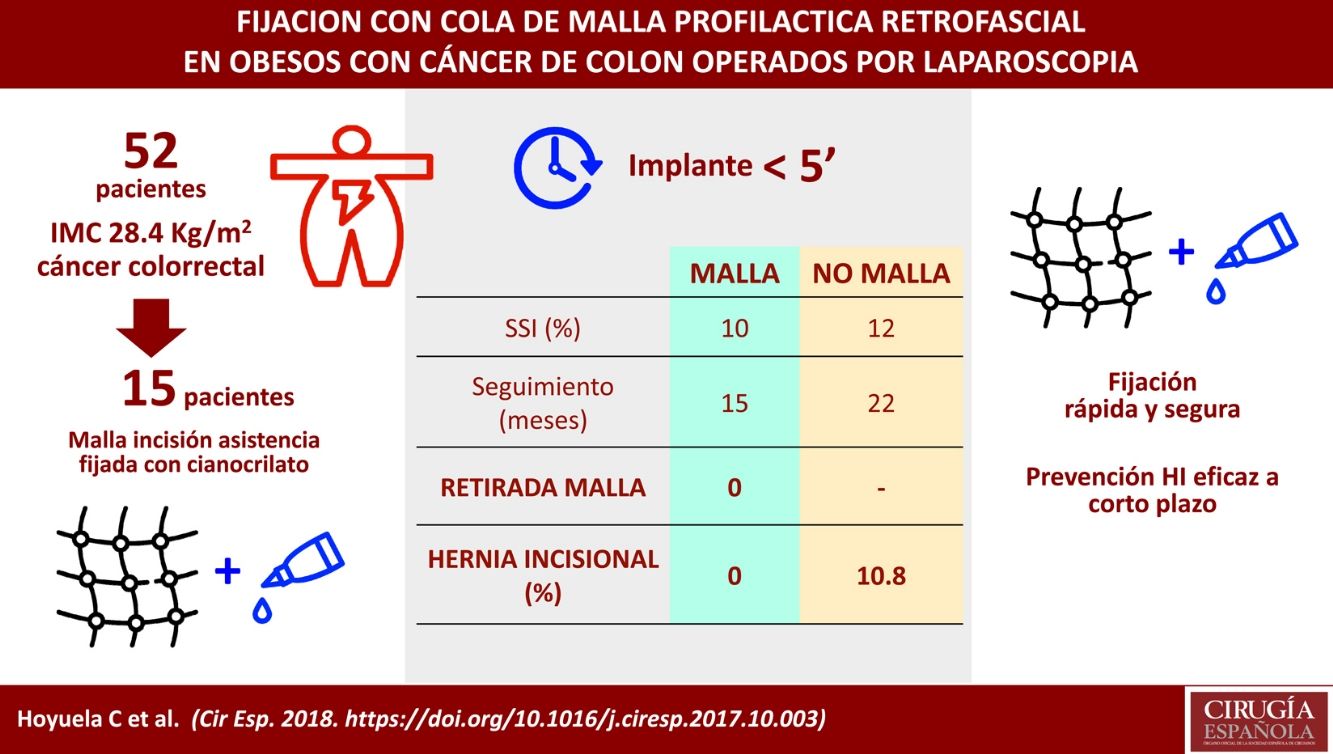
Results52 patients were analyzed (mean body mass index: 28.4±2kg/m2). Prophylactic meshes were implanted in 15 patients. The time to put the mesh in place was always less than 5min. There was no significant difference in wound infection rate (12% vs 10%). No mesh had to be explanted. Although the mean follow-up was shorter (14.1±4 vs 22.3±9 months), there were no incisional hernia in the mesh group. On the other hand, in the non-mesh group, 1 acute evisceration (2.7%) and 4 incisional hernia of the assistance incision were observed (10.8%). There were no significant differences between groups regarding trocar incisional hernia (6.6% vs 5.4%).
ConclusionsThe implantation of a reinforcement prophylactic mesh in overweight or obese patients undergoing laparoscopic colorectal surgery is safe and seems to reduce the short-term rate of incisional hernia. Fixation with cyanoacrylate is a rapid method that facilitates the procedure without additional complications.
La incidencia de hernia incisional en pacientes de riesgo (obesidad, cáncer, etc.) es elevada, incluso en cirugía laparoscópica. El objetivo de este estudio es evaluar la seguridad del empleo de mallas profilácticas retrofasciales fijadas con cianoacrilato en la incisión de asistencia en pacientes con sobrepeso sometidos a cirugía laparoscópica colorrectal.
MétodosEstudio prospectivo de cohortes, no aleatorizado, de pacientes sometidos a resección laparoscópica electiva por cáncer colorrectal entre enero de 2013 y marzo de 2016. Aquellos con índice de masa corporal superior a 25kg/m2 fueron evaluados para implantar una malla profiláctica fijada con cianoacrilato (Histoacryl®) como refuerzo de la incisión de asistencia.
ResultadosSe analizan 52 pacientes (índice de masa corporal medio: 28,4±2kg/m2). En 15 pacientes se implantó una malla profiláctica. El tiempo de implante siempre fue inferior a 5 minutos. No hubo diferencias significativas en la tasa de infección de herida (12 vs 10%). Ninguna malla requirió ser explantada. Aunque el seguimiento medio es menor (14,1±4 vs 22,3±9 meses), no ha aparecido hernia incisional en el grupo malla. Por el contrario, en el grupo no malla se han observado una evisceración (2,7%) y 4 eventraciones de la incisión de asistencia (10,8%). No hubo diferencias significativas entre los grupos respecto a hernia incisional de trócar (6,6 vs 5,4%).
ConclusionesLa implantación de mallas profilácticas en pacientes con sobrepeso u obesidad sometidos a cirugía laparoscópica colorrectal es segura y parece reducir la tasa de eventraciones a corto plazo. La fijación con cianoacrilato es un método rápido que facilita el procedimiento sin complicaciones adicionales.
The incidence of incisional hernia (IH) after laparotomy is between 9% and 22%, although it is likely that these figures are underestimated and could reach 35% in patients at risk.1–4 Identified risk factors include excess weight and obesity, aortic aneurysm surgery, or colostomy orifices.5 In these patients, the use of prophylactic mesh (PM) significantly reduces the incidence of incisional hernias.5–10
A higher-than-expected prevalence of IH (30%–39.9%) has also been observed in colorectal surgery, even after laparoscopic approaches.2,10,11 In fact, the incisional hernia rate of hand-assistance laparotomy in colorectal laparoscopy is similar to that of open surgery, although the place and type of incision used may be relevant.12,13
The appearance of an IH affects patient quality of life, motivates re-operations (occasionally urgent and with a risk of serious complications) and increases healthcare costs,2,14,15 so it is the inevitable objective of surgeons to reduce its incidence. This entails completing an adequate laparotomy closure in accordance with internationally accepted standards16 and adopting additional preventive measures in high-risk procedures and patient groups as indicated.2,7,14,17,18
Therefore, our group introduced the use of PM in 2015 to reinforce assistance incisions in patients undergoing laparoscopy who presented two associated risk factors: colon cancer and excess weight or obesity, with a body mass index (BMI) greater than 25.
The main objective of this study is to evaluate the safety of implantation of PM affixed with cyanoacrylate in the hand-assistance incisions of laparoscopic colorectal surgery and to report the main technical aspects of the procedure. Secondary objectives include the evaluation of the rates of early-onset incisional hernias, late-onset infection and chronic pain.
Material and MethodsWe present a non-randomized, prospective, controlled, observational cohort study. Included are 52 consecutive patients who underwent elective laparoscopic colon resection between January 2013 and March 2016, performed by a group of four surgeons. Since January 2015, patients diagnosed with colon cancer and a BMI greater than 25kg/m2 were evaluated for retrofascial PM implantation to reinforce the hand-assistance incision of laparoscopic surgery. All participants in the study gave their written consent prior to the operation. Exclusion criteria were: anesthetic contraindication for laparoscopy, emergency surgery, conversion to laparotomy, stomata, mesh placement in the suprafascial position or patient refusal.
To evaluate the safety of PM implantation and fixation with cyanoacrylate, the following postoperative abdominal wall complications were analyzed (30 days): infection (superficial or deep), dehiscence, hematoma and seroma.
Early-onset incisional hernias were defined as incisional hernias present on clinical examination or evident on abdominal CT during the first year of follow-up. The diagnosis of late-onset infection was determined by the presence of signs of inflammation, suppuration and/or positive culture, and appearance more than 30 days after surgery. Chronic pain was defined as persistent discomfort with a score ≥3 on the visual analog scale that persisted more than 3 months after surgery.19
The following variables have also been evaluated: age, gender, BMI, associated comorbidities (diabetes, use of anticoagulants), type of incision (midline, transverse lateral – subcostal or in the iliac fossa – and low transverse Pfannenstiel), wound size (measured at the incision of the aponeurosis), time used for mesh implantation, total surgical time and differences in hospital stay.
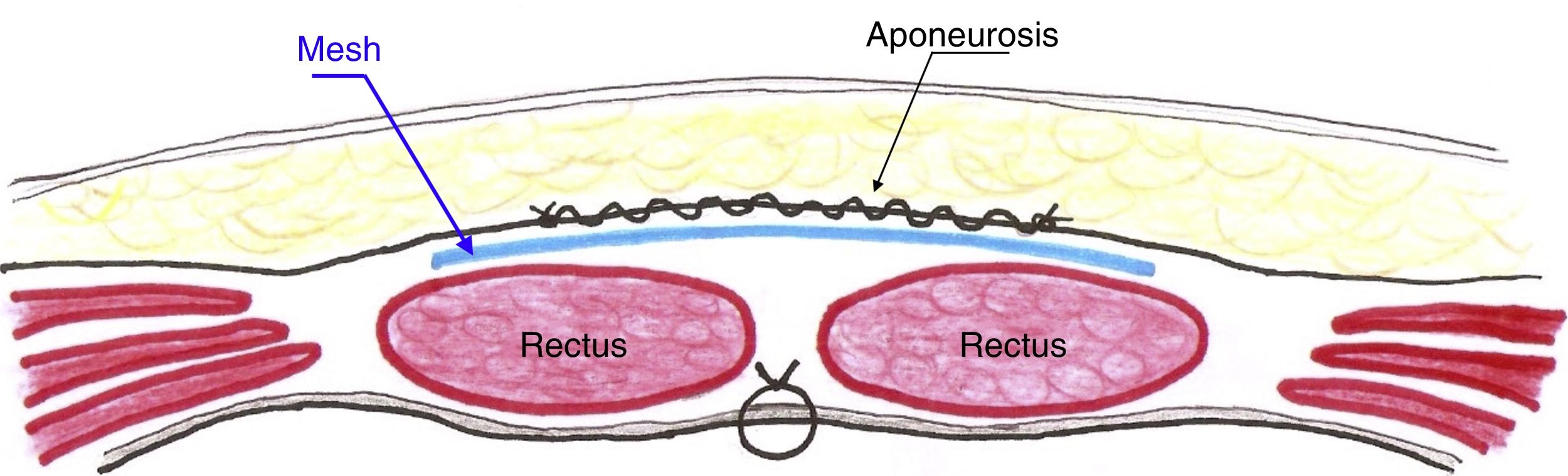
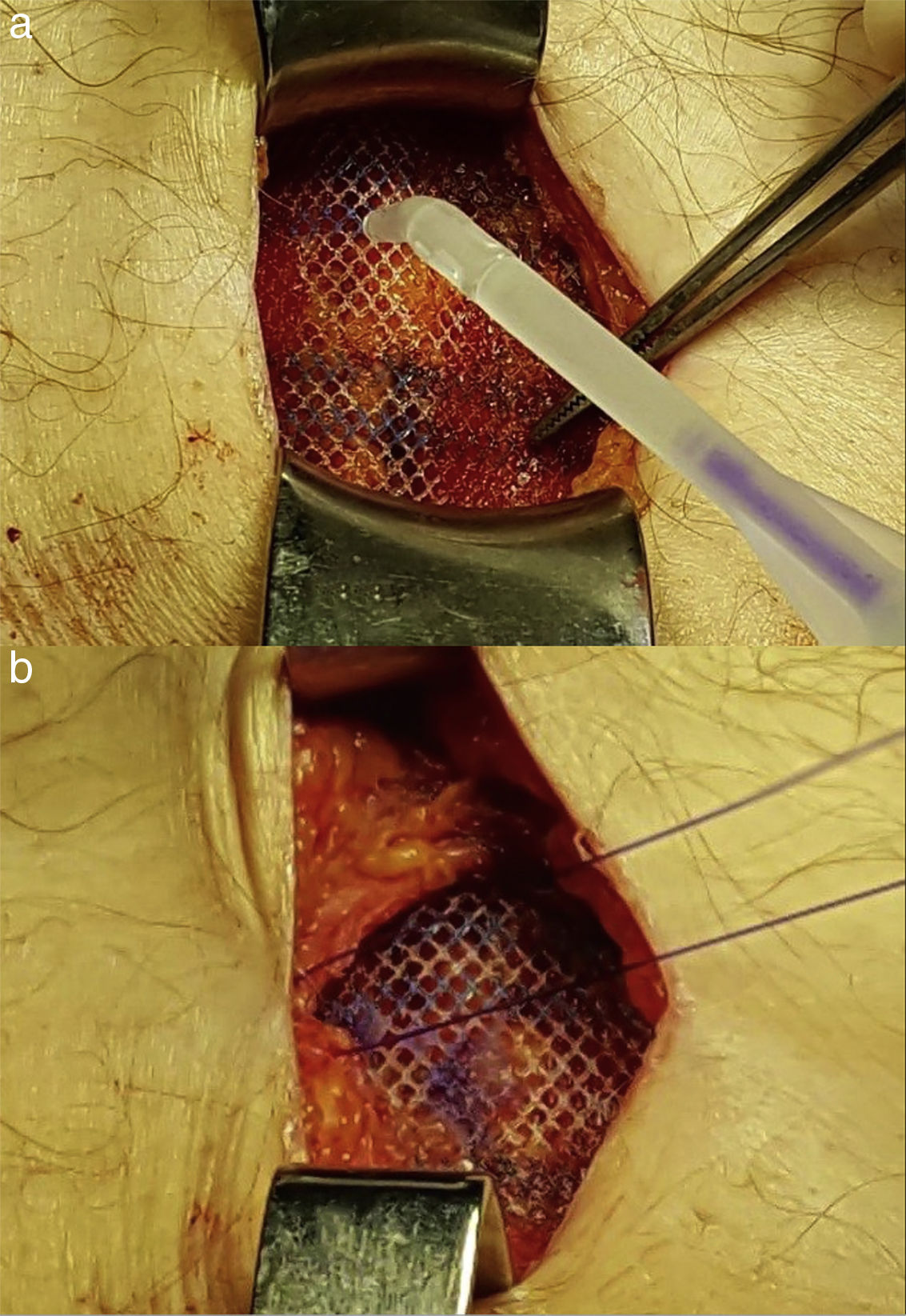
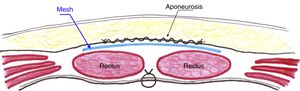
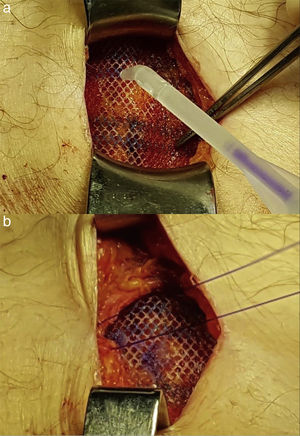
Surgical TechniqueAfter performing the assistance incision, a retrofascial and premuscular space is created where the mesh will be placed a posteriori (Fig. 1). Whether it is a vertical midline incision or a transverse incision, the recti abdominis muscles are easily detached from the anterior lamina of their sheath in a craniocaudal direction using blunt dissection. To access the abdomen and remove the surgical piece, the recti abdominis are separated along the midline, without cutting them. To prevent wound infection, in addition to the usual intravenous antibiotic therapy, a dual-ring wound protector is systematically used, and the wound is washed with abundant saline solution (1000cc) before closure. While not essential, the first step for closure of the incision is tobacco pouch or continuous peritoneal suture with 2/0 absorbable material (polyglactin – Vicryl®, Ethicon, Cincinnati, Ohio, USA, or polyglycolic acid – Novosyn® – B. Braun Surgical, Rubí, Spain). This suture line helps prevent an intestinal loop from accidentally coming into contact with the mesh. No suture is used to bring the recti closer to the midline. A low-weight, wide-pore polypropylene mesh (Optilene® 60g/m2, B. Braun Surgical, Melsungen, Germany) is placed on them after cutting to size so there are at least 3cm of overlap at the incisional margins. The mesh is affixed with a simple crown of cyanoacrylate drops (Histoacryl® – B. Braun Surgical) (Fig. 2) to the anterior surface of the recti. Finally, the fascia (anterior rectus sheath) is sutured continuously with very slow absorption monofilament material (size 0 poly-4-hydroxyburate, Monomax® – B. Braun Surgical), following a 4:1 ratio at least.20 In the event that the assistance incision is lateral, the mesh is implanted anterior to the internal oblique muscle and posterior to the aponeurosis of the external oblique using the same materials and steps to suture the different layers of the wall. Drainage is not used. The same abdominal closure technique (but without mesh implantation) was used to suture the incision in the patients of the non-mesh group.
The first clinical follow-up control took place in the outpatient clinic 7 days after surgery (or in the hospital if the patient remained hospitalized), and then 30 days, 3 and 6 months post-op, including a follow-up CT scan that was evaluated by an independent radiologist who was blind to the study. The clinical examination was carried out by the surgeon responsible and by another independent surgeon, who had not participated in the operation and was unaware of the presence or absence of the mesh.
Statistical AnalysisAll data were collected prospectively and included for analysis in an electronic database (Microsoft Access 2010 Microsoft Corporation, Redmond, Washington, USA). Although this is a non-randomized study, the groups were considered comparable; after accepting an alpha risk of 0.1 and a beta risk of 0.2 in a univariate comparison, the first group would require 13 subjects and 26 in the second group (ratio 2:1 between the number of subjects of both groups) to detect as statistically significant the differences between their proportions, expecting a reduction of the incisional hernia rate up to 10% in Group 1 (mesh) and assuming that the result of Group 2 (no mesh) would be 39.9%, in accordance with published data.2 The categorical variables were measured with frequencies and percentages, using the χ2 and Fisher's exact tests to compare both groups. The quantitative variables are expressed as means and standard deviation and were compared using the non-parametric Mann–Whitney U test. Statistical significance was established when P values were less than .05. The statistical analysis was performed with the IBM SPSS® Statistics program version 21.0 for Mac (IBM® Corp., Armonk, NY).
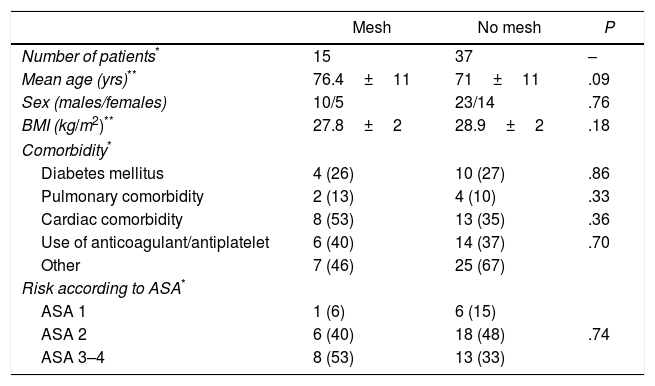
ResultsThis study analyzed a total of 52 patients with an average BMI of 28.4±2kg/m2, including 33 men and 19 women with an average age of 72.5±12 (range: 44–91). In 15 patients, a prophylactic mesh was implanted (mesh group). The demographic characteristics of the patients of both groups are summarized in Table 1.
Demographic Characteristics of the Patients of the Series.
| Mesh | No mesh | P | |
|---|---|---|---|
| Number of patients* | 15 | 37 | – |
| Mean age (yrs)** | 76.4±11 | 71±11 | .09 |
| Sex (males/females) | 10/5 | 23/14 | .76 |
| BMI (kg/m2)** | 27.8±2 | 28.9±2 | .18 |
| Comorbidity* | |||
| Diabetes mellitus | 4 (26) | 10 (27) | .86 |
| Pulmonary comorbidity | 2 (13) | 4 (10) | .33 |
| Cardiac comorbidity | 8 (53) | 13 (35) | .36 |
| Use of anticoagulant/antiplatelet | 6 (40) | 14 (37) | .70 |
| Other | 7 (46) | 25 (67) | |
| Risk according to ASA* | |||
| ASA 1 | 1 (6) | 6 (15) | |
| ASA 2 | 6 (40) | 18 (48) | .74 |
| ASA 3–4 | 8 (53) | 13 (33) | |
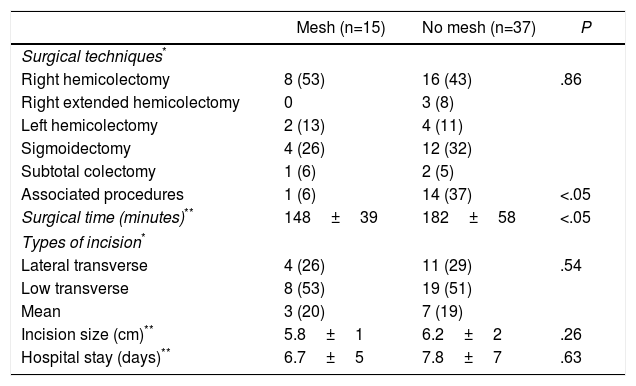
The mean surgical time was significantly lower in the mesh group (148 versus 182min), although in the non-mesh group (Table 2) a greater number of added procedures were performed (5 inguinal hernia repairs, 4 cholecystectomies, 2 bowel resections, one abdominal wall resection and an adnexectomy).
Surgical Techniques and Type of Incisions in Patients of the Series.
| Mesh (n=15) | No mesh (n=37) | P | |
|---|---|---|---|
| Surgical techniques* | |||
| Right hemicolectomy | 8 (53) | 16 (43) | .86 |
| Right extended hemicolectomy | 0 | 3 (8) | |
| Left hemicolectomy | 2 (13) | 4 (11) | |
| Sigmoidectomy | 4 (26) | 12 (32) | |
| Subtotal colectomy | 1 (6) | 2 (5) | |
| Associated procedures | 1 (6) | 14 (37) | <.05 |
| Surgical time (minutes)** | 148±39 | 182±58 | <.05 |
| Types of incision* | |||
| Lateral transverse | 4 (26) | 11 (29) | .54 |
| Low transverse | 8 (53) | 19 (51) | |
| Mean | 3 (20) | 7 (19) | |
| Incision size (cm)** | 5.8±1 | 6.2±2 | .26 |
| Hospital stay (days)** | 6.7±5 | 7.8±7 | .63 |
No differences were observed in the type of assistance incision used in the 2 groups (Table 2). The mesh placement time was always less than 5min (3.9±1).
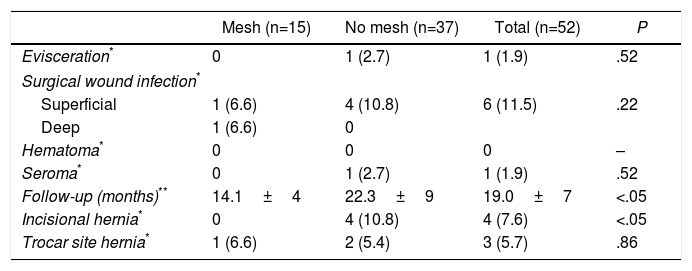
Table 3 summarizes short- and long-term abdominal wall complications. It should be noted that no adverse effects related to the use of cyanoacrylate were detected. We observed one evisceration (2.7%) in the non-mesh group on the fifth postoperative day in a cirrhotic patient who presented a synchronous lung neoplasm and eventually became the only death of the series 20 days after surgery (pneumonia and respiratory failure). Two other patients (3.8%) of the non-mesh group (but none in the mesh group) required laparoscopic re-operation (one due to suture dehiscence and another due to intestinal lesion), but the assistance incision was not manipulated. There were no significant differences in the wound infection rate of the series, although one deep infection was observed in the mesh group (Table 3). All of these cases were resolved with conservative treatment without requiring mesh removal (Clavien-Dindo I or II). No cases of late-onset infection were observed.
Short- and Long-Term Abdominal Wall Complications in Both Groups.
| Mesh (n=15) | No mesh (n=37) | Total (n=52) | P | |
|---|---|---|---|---|
| Evisceration* | 0 | 1 (2.7) | 1 (1.9) | .52 |
| Surgical wound infection* | ||||
| Superficial | 1 (6.6) | 4 (10.8) | 6 (11.5) | .22 |
| Deep | 1 (6.6) | 0 | ||
| Hematoma* | 0 | 0 | 0 | – |
| Seroma* | 0 | 1 (2.7) | 1 (1.9) | .52 |
| Follow-up (months)** | 14.1±4 | 22.3±9 | 19.0±7 | <.05 |
| Incisional hernia* | 0 | 4 (10.8) | 4 (7.6) | <.05 |
| Trocar site hernia* | 1 (6.6) | 2 (5.4) | 3 (5.7) | .86 |
Although the patient follow-up in the mesh group was shorter (14.1±4 vs 22.3±9 months), no patients in the mesh group have presented an incisional hernia of the hand-assistance incision to date. In contrast, herniated assistance incisions occurred in 4 patients of the non-mesh group (3 midline and one subcostal), which is a rate of 10.8%. These hernias appeared 10, 11, 16 and 18 months after the intervention. All hernias were clinically observable and confirmed with abdominal CT. Two out of the 4 patients have already undergone incisional hernia repair. No significant differences were found in terms of the additional appearance of a trocar site hernia (6.6% vs 5.4%). No patients in the series reported chronic pain during follow-up.
DiscussionThe results of this study support the concept that PM can significantly reduce incisional hernia incidence without increasing the rate of postoperative complications in selected patients, in this case, overweight or obese patients undergoing laparoscopic resection for colorectal cancer.
At present, the use of PM in at-risk patients is based on solid evidence. PM have shown their efficacy and safety in patients with colon cancer, even in emergency surgery and in the presence of peritonitis.2,11,21,22 On the other hand, the presence of a BMI greater than 25kg/m2 (overweight or obese) is an independent factor that increases the risk for incisional hernia exponentially.5,23 It seems clear, therefore, that patients who present both associated factors should be candidates for the implantation of prophylactic mesh. The incision site should also be considered, since midline laparotomy is the most frequently affected by incisional hernia.13 Reinforcement with a small wide-pore polypropylene mesh is a step that does not significantly increase the costs of the procedure and is cost effective.14
In the patients in this series, the mesh was affixed with cyanoacrylate (Histoacryl®). Its application is simple (even in obese patients), easily reproducible and hardly prolongs operative time since its application has been shown to be faster than sutures.24 In addition, non-traumatic fixation with glue would avoid additional secondary pain, and in this small group there has been no increased risk. An added positive factor is that this technique has been able to be applied in any type of assistance incision in laparoscopic surgery, including lateral incisions.
Although there is not enough evidence about which position is the best to implant the mesh, we have chosen to place it in a premuscular and retrofascial position to keep it away from the intestinal loops (reducing the risk of inclusion, occlusion or fistula) and partially protect it from a possible superficial infection of the surgical wound.25
It is precisely the possible wound complications associated with the use of prophylactic meshes (seroma, infection, chronic pain), and whether the presence of the mesh can hinder their treatment, which contributes to maintaining the controversy regarding its systematic use.17,26 Although the number of patients in the series with mesh is limited, the observed complications have been resolved without additional difficulties.
The size of the series as well as the absence of randomization can be considered limitations of this study. Likewise, the differences in follow-up require a longer period of time to reliably determine the incisional hernia rate in both groups, especially the mesh group. However, the technical homogeneity of the procedures (all cases were treated by the same team), thorough monitoring and follow-up (with no loss of patients), evaluation of a blinded independent radiologist and prospective data collection guarantee the reliability of the results, especially the differences in the incidence of incisional hernia.
In conclusion, the use of PM in patients with two associated risk factors (colon cancer and BMI>25kg/m2) is, in our opinion, safe and seems to reduce the rate of incisional hernias, although this claim should probably be confirmed by a randomized prospective study. Mesh fixation with cyanoacrylate (Histoacryl®) is a rapid method that facilitates the procedure with no additional complications.
Conflict of InterestsThe authors have no conflict of interests to declare.
This study was completed as part of the Doctorate Program in Surgery and Morphological Sciences of the Surgery Department at the Universitat Autònoma de Barcelona.
Part of this study was presented at the 39th Annual International Congress of the European Hernia Society in Vienna, May 24-27, 2017.
Please cite this article as: Hoyuela C, Juvany M, Trias M, Ardid J, Martrat A. Prevención de la hernia incisional mediante malla retrofascial fijada con cianoacrilato. Cir Esp. 2018;96:35–40.