There are some circumstances in which the descending colon does not reach the pelvis to complete a colorectal anastomosis without tension. Re-establishing intestinal continuity by interposing small bowel as a bridge between the colon and the rectum could be an acceptable surgical alternative.
MethodsWe describe the interposition of one or two segments of small bowel as a way of restoring continuity of the colon and rectum in three patients in whom it was not possible to perform a colorectal anastomosis without tension due to ischemic colon, synchronous cancer or difficulty in accessing the supramesocolic space, respectively.
ResultsIntestinal continuity was re-established in all patients with no significant morbidity and good intestinal function.
ConclusionThe interposition of small bowel segments between the colon and the rectum should be considered as a valid surgical option when it is not possible to achieve a well-perfused, tension-free pelvic colorectal anastomosis.
Existen algunas circunstancias en las que el colon descendente no es válido, está ausente o no alcanza la pelvis para realizar una anastomosis colorrectal sin tensión. Una de las opciones quirúrgicas posibles para recuperar la continuidad digestiva es realizar una interposición de intestino delgado entre el colon y recto a anastomosar.
MétodosSe describe a 3 pacientes en los cuales era imposible la realización de una anastomosis colorrectal sin tensión por presentar afección síncrona en el recto y el colon izquierdo, un colon izquierdo isquémico y un compartimento supramesocólico inabordable, respectivamente, practicándose en los 3 una interposición de una o 2 asas de intestino delgado, como puente o forma de reconstrucción del tránsito entre el colon y el recto.
ResultadosLos pacientes recuperaron la continuidad digestiva sin morbilidad significativa. La función intestinal resultante ha sido buena. La endoscopia de seguimiento mostró inicialmente una discreta inflamación de la mucosa del intestino delgado que ha desapa-recido posteriormente.
ConclusiónCuando el colon descendente es insuficiente para una anastomosis pélvica bien irrigada y sin tensión, la interposición de intestino delgado entre el colon y el recto es una alternativa válida y a tener en cuenta para este fin.
There are several clinical circumstances in which it is impossible to perform a well-irrigated, tension-free colorectal pelvic anastomosis despite complete mobilization of the splenic flexure and transverse colon to the middle colic artery (MCA) on one side and the rectum or rectosigmoid junction on the other.
Some of these situations can be anticipated preoperatively, such as cases of splenic colon cancer in a patient with a prior left colectomy or synchronous cancer in the rectum/rectosigmoid junction and descending/splenic colon, for example. Others arise as unexpected intraoperative findings, like the existence of fibrotic diverticular disease, splenic flexure that is untreatable or previous supramesocolic surgery. There are also cases of intraoperative complications secondary to accidental injury of the marginal artery of the colon or severe arteriosclerosis and separation of the inferior mesenteric artery (IMA) at its origin.
One option for reconstructing the digestive tract under these circumstances may be the interposition of the small intestine between the colon and rectum.
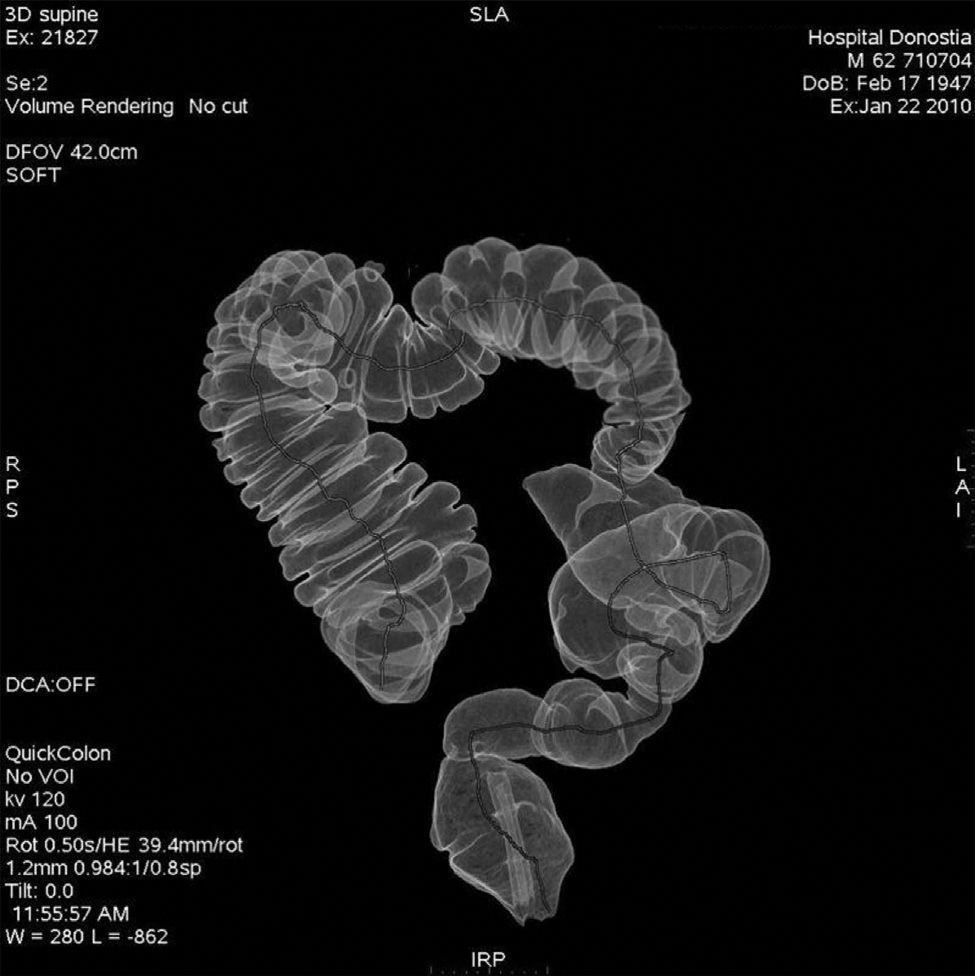
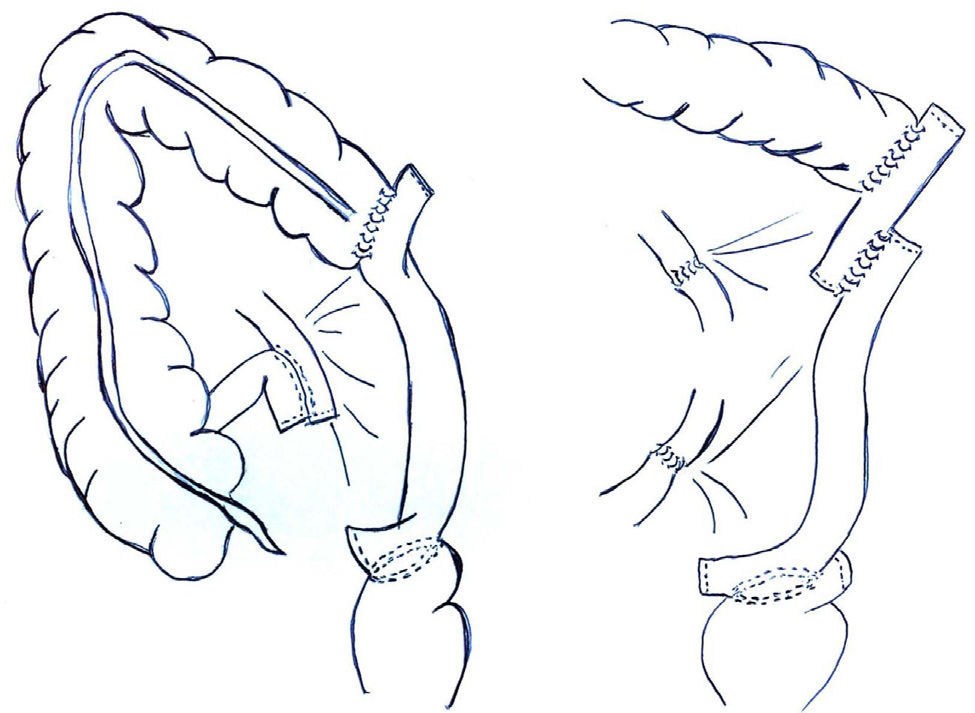
We have performed interposition of the small intestine in 3 male patients. The first patient, aged 61, presented synchronous cancer of the upper rectum and descending colon, although it was later found during surgery that the latter was actually located in the descending slope of the splenic flexure. After fully mobilizing the rectum and colon up to the MCA and verifying that it was not possible to perform a transverso-rectostomy, the tract was reconstructed with 2 loops of small intestine between the colon and rectum (the superior from the jejunum and the inferior from the ileum) so that the interposition between the colon and rectum was shorter and more direct, even though this entailed performing more anastomoses. The postoperative period was uneventful. The patient developed diarrhea during the first 3 months, which disappeared gradually. Currently (3 years later), the patient has correct gastrointestinal function, with no need for medication. The initial follow-up colonoscopy showed mild inflammation of the small intestine that disappeared within one year (Fig. 1).
Subsequently, we have used interposition of the intestine in two other occasions: a 71-year-old patient with sigmoid cancer and ischemia of the descending colon after central ligation of the IMA and inadvertent damage to the marginal artery while mobilizing the splenic flexure, and another 66-year-old patient with an unapproachable supramesocolic compartment due to complications from previous surgery. In both cases, a single loop of ileum was used as interposition (Fig. 2). In none of the three cases a protective stoma was used. No major complications were recorded, and the functional results in both cases are satisfactory.
In situations where it is not possible to carry out a well-irrigated, tension-free pelvic colorectal anastomosis after fully mobilizing both structures, the 2 most widely known and used surgical alternatives are ileorectal anastomosis and “ascendo-rectostomy”. Both cases require expanding the colectomy.
In the former case, a total colectomy is performed, with well-known functional results and consequences that may be undesirable in older patients or in cases that require removal of the rectum. The second alternative requires removing the transverse colon (whose main function is solidifying the feces), dividing the right colonic blood vessels and completely mobilizing the right colon, performing a 180° counter-clockwise rotation while using the ileocolic vessels as an axis, which must be carefully preserved to reconstruct the tract by means of an anastomosis between the ascending colon and rectum.1,2 Although it has been well described in the literature, it is not an easy procedure to perform, especially in patients with thick/fatty mesocolon, short colon, previous surgery or arteriosclerosis, which occasionally requires going through the mesentery to reach the pelvis. While the ileocecal reservoir, as described by Von Flüe, can be used under some of the circumstances mentioned, it is more of a reconstruction procedure instead of an attempt at improving the functionality of the anterior resection of the rectum with total mesorectal excision.3
To our surprise, we only found 2 articles in the medical literature on the interposition of the small intestine between the colon and the rectum when it is impossible to carry out a tension-free pelvic anastomosis. One dates from 1927, in which the author indicates the use of this technique although without ever using it,4 and the other is a clinical report published in 2008.5
The main advantages of the interposition of the small intestine are the good functional results observed and the avoidance of having to carry out extensive mobilizations or to remove healthy functional colon. Furthermore, this may also benefit patients with medical-surgical problems and a tendency toward diarrhea. Its main and obvious disadvantage is the need for more anastomoses (3 when one loop is used and 4 or 5 when 2 are used), although it is performed with better vascularized ends when compared with an ascending colon rotated on its vascular pedicle. The inflammation of the interposed ileum was transitory. Nonetheless, the risk for developing carcinoma in the long-term in this segment is difficult to anticipate, and it is therefore recommended to comply with the follow-up protocol for colorectal cancer.
We believe that the interposition of the small intestine is a valid surgical technique that can help surgeons in these situations, which fortunately are infrequent.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Enríquez-Navascues JM, Rodríguez A, Placer C, Saralegui Y, Carrillo A. Interposición de intestino delgado entre el colon y el recto como forma de lograr una anastomosis pélvica sin tensión. Cir Esp. 2013;91:602–604.