To assess the quality of the information that patients receive in the informed consent document signed prior to surgery.
Materials and methodsCross-sectional study of a sample of cancer patients admitted for surgery at the University Hospital San Cecilio of Granada in 2011. After checking the inclusion criteria and obtaining their consent, demographic data were collected and procedure data, and a questionnaire “ad hoc” to assess the quality and comprehensiveness of the information provided in the informed consent.
Results150 patients were studied. The majority (109 over 150) said they had received sufficient information, in appropriate language, and had the opportunity to ask questions, but only 44.7% correctly answered three or more issues related to anaesthesia. University education level, knowledge of the intervention, information about the anaesthesia problems and appropriate language were associated.
ConclusionsAlthough systematic informed consent is regularly obtained, half of the patients did not comprehend the anaesthesia risks. Variables primarily related to the information received were associated with the quality of the response, but not with patient characteristics.
Valorar la calidad de la información recibida sobre los contenidos que se detallan en el documento de consentimiento informado que han firmado previamente los pacientes, mediante las respuestas que estos dan a un cuestionario abierto.
Material y métodosEstudio transversal de una muestra de pacientes oncoló gicos ingresados para cirugía en el Hospital Universitario San Cecilio de Granada durante el año 2011. Tras comprobar los criterios de inclusión y recabar su consentimiento se recogieron datos demográficos y del proceso, y un cuestionario ad hoc para valorar la calidad y comprensión de la información suministrada en el consentimiento informado.
ResultadosSe estudiaron 150 pacientes. La mayoría (109 de 150) contestó que había recibido suficiente informació n, con un lenguaje adecuado y la posibilidad de preguntar dudas, pero solo el 44,7% contestó correctamente a 3 o más de las 4 cuestiones realizadas sobre problemas relacionados con la anestesia. Se asociaron a la asimilación de la información recibida el nivel de estudios universitario, el conocimiento de la intervención a realizar, haber recibido información sobre los problemas derivados de la anestesia, considerar que la información recibida había sido suficiente y en un lenguaje adecuado.
ConclusionesA pesar de la obtención sistemática del consentimiento informado, casi la mitad de los pacientes ignora los riesgos de la anestesia. Se asociaron con la calidad de la respuesta fundamentalmente las variables relacionadas con la información recibida, pero no las características del paciente.
Spanish law establishes that patients have the right to be informed before receiving any healthcare action (Articles 156 of the Penal Code1 and 8–10 of the Law of Patient Autonomy,2 which state the “right of the patient to information and free choice once they have received adequate information”). In Andalusia, the Ministry of Health (Ordinance of July 8th, 2009)3 defines written informed consent as consent in writing that is reflected in a specific document that must be filed with the relevant medical history, including both the clinical information provided to the patient or their representative and their agreement to undergo the intervention or clinical procedure to be performed.
The information must be comprehensive, adequate, accurate, truthful and faithful and also made clear and understandable to the patient or his/her family members who must give consent on the patient's behalf. This requirement means that informed consent should not only provide information, but also ensure that the patient understands all the terms, guaranteeing a proper doctor-patient interaction.4 In general, there exists an increasing awareness of the need for patient information as well as the need for using new alternatives to enhance the ability of decision making through improved understanding.5
However, few studies have evaluated the comprehension of informed consent; some have analysed patient understanding of the risks of the procedure, while others have focused on knowledge about benefits, alternatives, and the overall procedure.6 Most of these previous studies have concluded that knowledge and understanding of surgical treatments and/or anaesthesia risk are low for patients,7,8 with added difficulties for older patients or those with lower levels of education. Surgical patients are generally poorly informed about their illness and the proposed treatments. In particular, these patients are not sufficiently informed about the risks of anaesthesia9 and are therefore poorly equipped to make autonomous decisions regarding their treatment.5,7 In Spain, according to data published in 2007,10 almost one-half of all health professionals do not know what informed consent is (including its component parts) and also do not know the law that regulates informed consent and the philosophy with which it was created. Most professionals think of informed consent as a professional tool to protect against possible lawsuits and also feel that these documents are difficult to read and difficult for patients to understand, which leads to an information overload that insufficiently explains the procedure or intervention requiring consent.
In this study, we sought to evaluate the quality of the information received in informed consent documents using answers to an open questionnaire.
Materials and MethodsThis cross-sectional study was conducted at the San Cecilio University Hospital in Granada between March and December 2011.
Reference PopulationCancer patients undergoing surgery served as the reference population. Each patient signed an informed consent form for general, regional or local anaesthesia, which is available at http://www.juntadeandalucia.es/salud/export/sites/csalud/galerias2/documentos/ci2/anestesia_general_y_local.pdf (Accessed 15.03.13), during the pre-anaesthetic consultation performed prior to hospital admission. This document provided enough information about the anaesthetic procedure, risks, discomfort, side effects and benefits with sufficient clarity to allow understanding by quick reading or a simple explanation.
Eligible PopulationEligible patients were those admitted for surgery in the General Surgery and Gastroenterology, Urology and Gynaecology units at the San Cecilio University Hospital.
Selection Criteria- 1.
Capacity to participate in the study and complete the self-administered questionnaire.
- 2.
Consent to participate in the study.
- 3.
Admission for surgery for the first time as a result of an oncologic process.
- 4.
Age over 18 years.
- 1.
Severe sensory disability that hampers the understanding and performance of tests to be used.
- 2.
Inability to speak Spanish fluently.
- 3.
Having an acute or chronic psychiatric condition.
- 4.
Severe cognitive impairment.
The final sample consisted of 150 patients admitted to the General Surgery and Gastroenterology, Urology and Gynaecology units and others selected at random during preoperative hospital admission. With this number of patients, it was possible to detect significant differences in percentage changes of 12 points on a benchmark of less than 18 points, with a power of 80% and an alpha error of 5%.
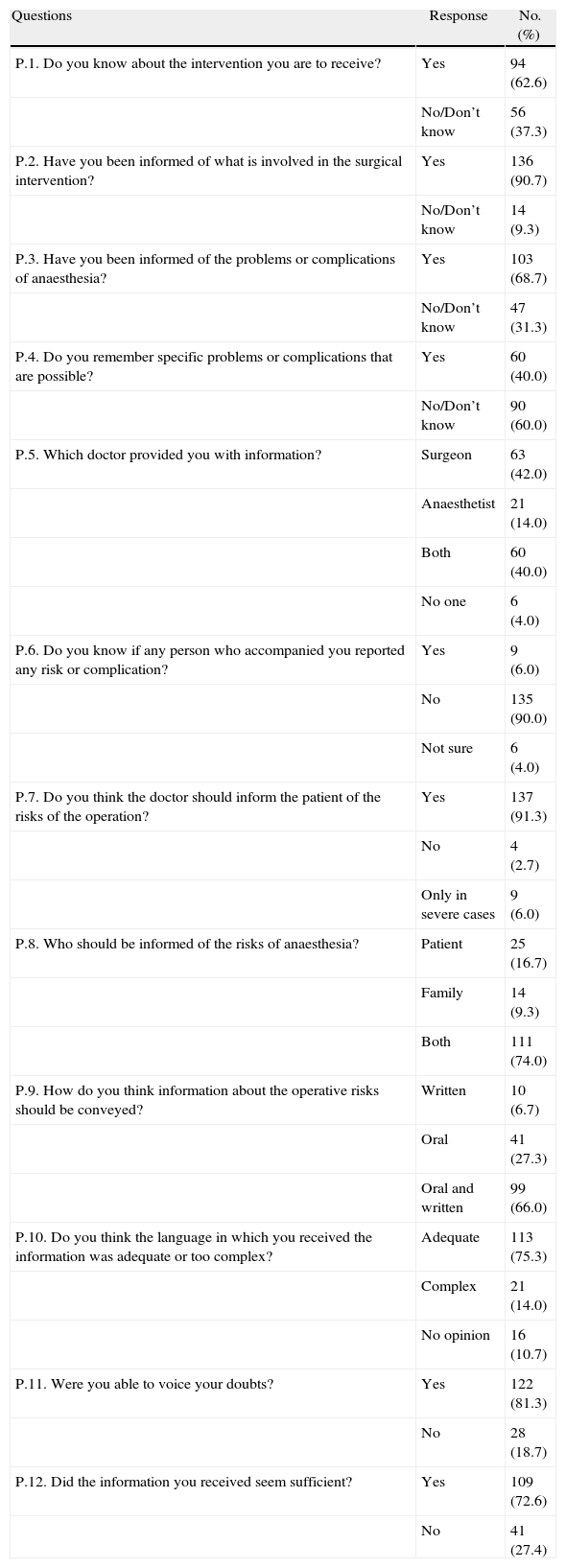
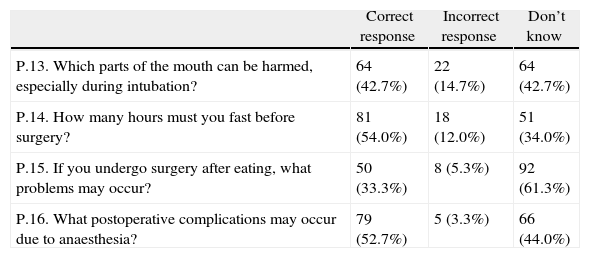
Collection of InformationAt the time of admission, after verification of inclusion criteria and obtaining consent for participation in the study, patients were given a questionnaire designed to address 16 items. The first 12 items addressed demographics (Table 1), and the 4 remaining assessed the understanding of the information received in the written informed consent. Finally, a review variable was constructed for the quality of the information, for which the correct answers to questions 13–16 (Table 2) were added. These questions referred, respectively, to the parts of the mouth that can be damaged by the endotracheal tube, potential problems that could occur if the intervention is performed after eating, the recommended preoperative fasting times and the postoperative complications that can occur as a result of anaesthesia. The quality of the information was poor when the number of correct responses was less than 2 and good when this number was 3 or 4.
Questions that Assess the Patient's Opinion About the Information Received.
| Questions | Response | No. (%) |
| P.1. Do you know about the intervention you are to receive? | Yes | 94 (62.6) |
| No/Don’t know | 56 (37.3) | |
| P.2. Have you been informed of what is involved in the surgical intervention? | Yes | 136 (90.7) |
| No/Don’t know | 14 (9.3) | |
| P.3. Have you been informed of the problems or complications of anaesthesia? | Yes | 103 (68.7) |
| No/Don’t know | 47 (31.3) | |
| P.4. Do you remember specific problems or complications that are possible? | Yes | 60 (40.0) |
| No/Don’t know | 90 (60.0) | |
| P.5. Which doctor provided you with information? | Surgeon | 63 (42.0) |
| Anaesthetist | 21 (14.0) | |
| Both | 60 (40.0) | |
| No one | 6 (4.0) | |
| P.6. Do you know if any person who accompanied you reported any risk or complication? | Yes | 9 (6.0) |
| No | 135 (90.0) | |
| Not sure | 6 (4.0) | |
| P.7. Do you think the doctor should inform the patient of the risks of the operation? | Yes | 137 (91.3) |
| No | 4 (2.7) | |
| Only in severe cases | 9 (6.0) | |
| P.8. Who should be informed of the risks of anaesthesia? | Patient | 25 (16.7) |
| Family | 14 (9.3) | |
| Both | 111 (74.0) | |
| P.9. How do you think information about the operative risks should be conveyed? | Written | 10 (6.7) |
| Oral | 41 (27.3) | |
| Oral and written | 99 (66.0) | |
| P.10. Do you think the language in which you received the information was adequate or too complex? | Adequate | 113 (75.3) |
| Complex | 21 (14.0) | |
| No opinion | 16 (10.7) | |
| P.11. Were you able to voice your doubts? | Yes | 122 (81.3) |
| No | 28 (18.7) | |
| P.12. Did the information you received seem sufficient? | Yes | 109 (72.6) |
| No | 41 (27.4) |
Questions that Assess Patient Understanding of the Information Received.
| Correct response | Incorrect response | Don’t know | |
| P.13. Which parts of the mouth can be harmed, especially during intubation? | 64 (42.7%) | 22 (14.7%) | 64 (42.7%) |
| P.14. How many hours must you fast before surgery? | 81 (54.0%) | 18 (12.0%) | 51 (34.0%) |
| P.15. If you undergo surgery after eating, what problems may occur? | 50 (33.3%) | 8 (5.3%) | 92 (61.3%) |
| P.16. What postoperative complications may occur due to anaesthesia? | 79 (52.7%) | 5 (3.3%) | 66 (44.0%) |
Additional study variables included age (years old), sex, marital status (married or other), educational level (no education, primary, secondary or university), work status (employed, retired, housewife or other), living arrangement (living alone or with others), anaesthetic risk (ASA category) and previous anaesthesia (no or yes).
Statistical analysis was performed using the Stata 10.0 package. For qualitative variables, the frequencies were estimated and used to verify the Chi square associations. For quantitative variables, we estimated the mean and 95% confidence interval and used the analysis of variance as a way to compare means.
ResultsThis study included a total of 150 patients with a mean age of 58.3±12 years (median 60; range 28–83), of which 69 (46.0%) were male and 81 (54.0%) were female. The majority of patients were married (78.0%), not living alone and had 2 or more children. over one-half of the sample population had only primary school or no schooling. Almost 80% of the study population had previously undergone anaesthesia. The conditions leading to admission were tumours, including gastrointestinal tumours, in 65 cases (43.3%); gynaecological or urological in 72 (58.0%); and other processes in 13 (8.7%).
Table 1 lists the variables referring to the information provided. Over 90% of patients acknowledged having been informed, although one-third of them did not know what type of intervention would be performed. Regarding the problems associated with anaesthesia, almost 70% of patients stated they had been informed, but only 40% recalled specific risks. The vast majority of patients believed both they and their family should be informed about the risks of intervention and that the message must be both verbally communicated and written. Most of the patients answered that they had received sufficient information, in an appropriate language, and had been able to ask questions. Only 19% said they were not able to raise any doubts or questions they may have had.
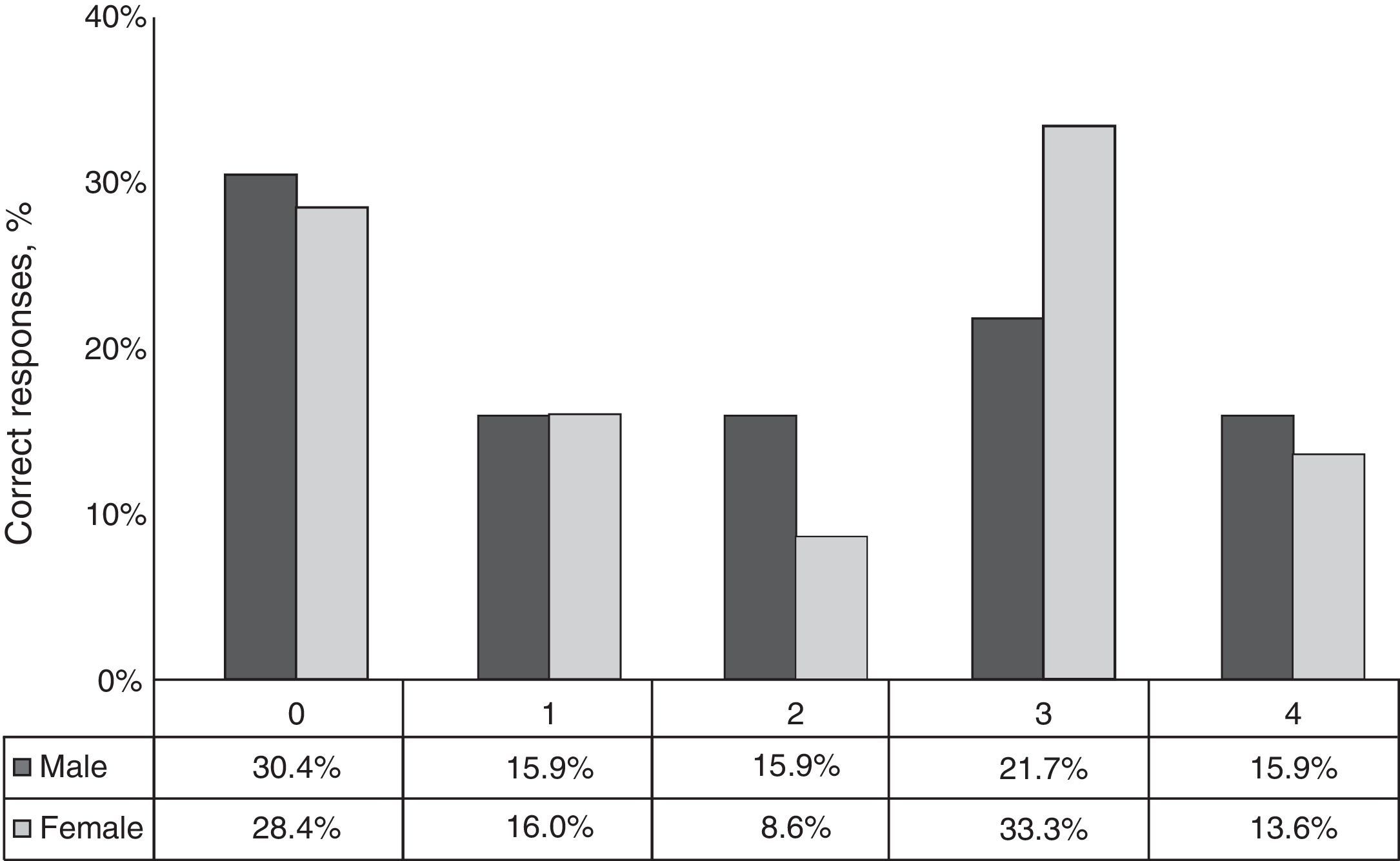
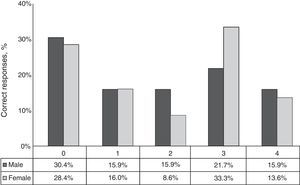
The questions to assess comprehension (Table 2) were open-ended and classified as correct or incorrect according to what was reflected in the signed informed consent form. Most of the responses that were classified as incorrect were because the patient did not know what to answer; 44 patients (29.3%) did not answer any questions correctly, and only 42 (28.0%) answered questions 3 and 22 (14.7%) with 4 correct answers. Fig. 1 shows the data stratified by gender; there were no statistically significant differences between men and women. These data imply that only 42.7% of patients understood the information received during informed consent for anaesthesia.
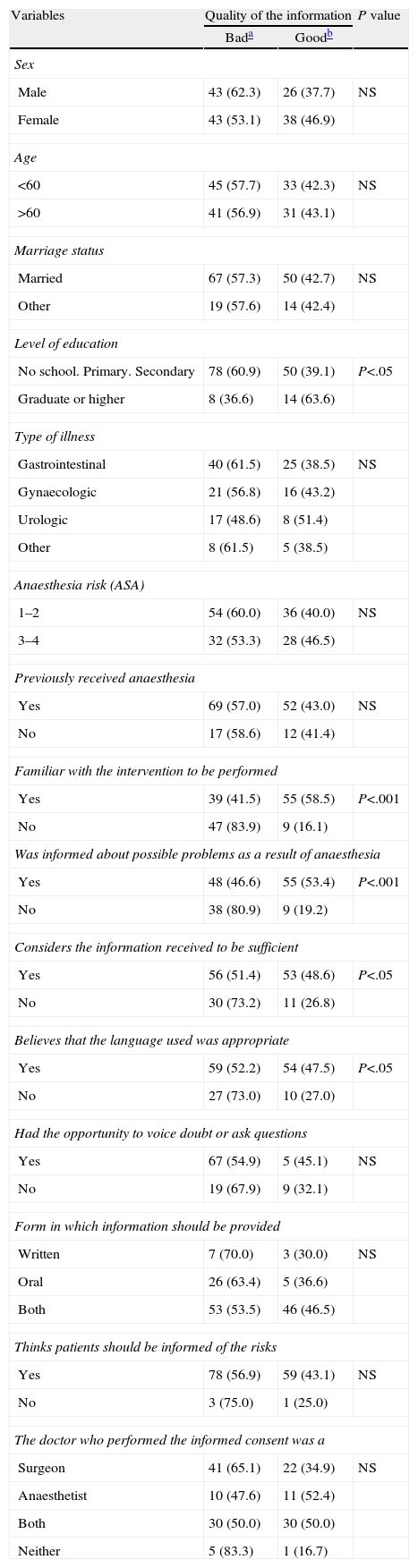
We next studied the comprehension of information stratified by the remaining variables (Table 3). No significant differences were seen in terms of patient characteristics, except regarding the level of education when comparing subjects with higher education to the rest, and there were no differences when stratified by the type of disease process, anaesthesia risk or history of anaesthesia. There was, however, a significantly higher percentage of correct answers among those who said they had received information about the anaesthesia process; these patients considered the information they received to be sufficient and provided in an appropriate language, or these subjects claimed to know the type of intervention that would be performed. Even so, the percentage of incorrect responses in these patients ranged between 41% and 51%. The type of doctor who administered the informed consent was not significantly associated with the percentage of correct answers, nor was the opportunity to ask questions or patient preferences regarding the way they should receive the information.
Variables Associated With the Quality of the Information Provided.
| Variables | Quality of the information | P value | |
| Bada | Goodb | ||
| Sex | |||
| Male | 43 (62.3) | 26 (37.7) | NS |
| Female | 43 (53.1) | 38 (46.9) | |
| Age | |||
| <60 | 45 (57.7) | 33 (42.3) | NS |
| >60 | 41 (56.9) | 31 (43.1) | |
| Marriage status | |||
| Married | 67 (57.3) | 50 (42.7) | NS |
| Other | 19 (57.6) | 14 (42.4) | |
| Level of education | |||
| No school. Primary. Secondary | 78 (60.9) | 50 (39.1) | P<.05 |
| Graduate or higher | 8 (36.6) | 14 (63.6) | |
| Type of illness | |||
| Gastrointestinal | 40 (61.5) | 25 (38.5) | NS |
| Gynaecologic | 21 (56.8) | 16 (43.2) | |
| Urologic | 17 (48.6) | 8 (51.4) | |
| Other | 8 (61.5) | 5 (38.5) | |
| Anaesthesia risk (ASA) | |||
| 1–2 | 54 (60.0) | 36 (40.0) | NS |
| 3–4 | 32 (53.3) | 28 (46.5) | |
| Previously received anaesthesia | |||
| Yes | 69 (57.0) | 52 (43.0) | NS |
| No | 17 (58.6) | 12 (41.4) | |
| Familiar with the intervention to be performed | |||
| Yes | 39 (41.5) | 55 (58.5) | P<.001 |
| No | 47 (83.9) | 9 (16.1) | |
| Was informed about possible problems as a result of anaesthesia | |||
| Yes | 48 (46.6) | 55 (53.4) | P<.001 |
| No | 38 (80.9) | 9 (19.2) | |
| Considers the information received to be sufficient | |||
| Yes | 56 (51.4) | 53 (48.6) | P<.05 |
| No | 30 (73.2) | 11 (26.8) | |
| Believes that the language used was appropriate | |||
| Yes | 59 (52.2) | 54 (47.5) | P<.05 |
| No | 27 (73.0) | 10 (27.0) | |
| Had the opportunity to voice doubt or ask questions | |||
| Yes | 67 (54.9) | 5 (45.1) | NS |
| No | 19 (67.9) | 9 (32.1) | |
| Form in which information should be provided | |||
| Written | 7 (70.0) | 3 (30.0) | NS |
| Oral | 26 (63.4) | 5 (36.6) | |
| Both | 53 (53.5) | 46 (46.5) | |
| Thinks patients should be informed of the risks | |||
| Yes | 78 (56.9) | 59 (43.1) | NS |
| No | 3 (75.0) | 1 (25.0) | |
| The doctor who performed the informed consent was a | |||
| Surgeon | 41 (65.1) | 22 (34.9) | NS |
| Anaesthetist | 10 (47.6) | 11 (52.4) | |
| Both | 30 (50.0) | 30 (50.0) | |
| Neither | 5 (83.3) | 1 (16.7) | |
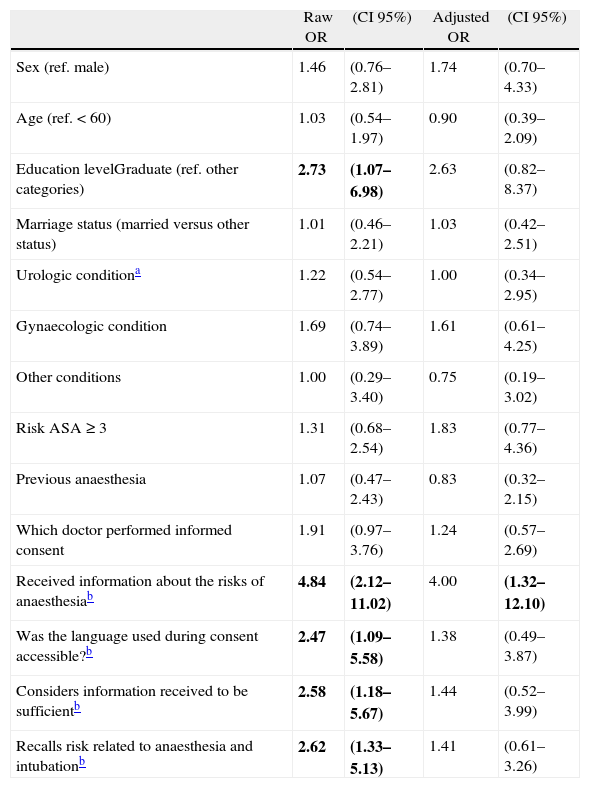
Finally, crude and adjusted odds ratios (OR) were calculated to evaluate the effect of different variables on the quality of the final responses (Table 4). The only variable that demonstrated a significant independent effect was that the patient had been informed of the potential risks of anaesthesia.
Effect of Variables on the Quality of the Responses.
| Raw OR | (CI 95%) | Adjusted OR | (CI 95%) | |
| Sex (ref. male) | 1.46 | (0.76–2.81) | 1.74 | (0.70–4.33) |
| Age (ref.<60) | 1.03 | (0.54–1.97) | 0.90 | (0.39–2.09) |
| Education levelGraduate (ref. other categories) | 2.73 | (1.07–6.98) | 2.63 | (0.82–8.37) |
| Marriage status (married versus other status) | 1.01 | (0.46–2.21) | 1.03 | (0.42–2.51) |
| Urologic conditiona | 1.22 | (0.54–2.77) | 1.00 | (0.34–2.95) |
| Gynaecologic condition | 1.69 | (0.74–3.89) | 1.61 | (0.61–4.25) |
| Other conditions | 1.00 | (0.29–3.40) | 0.75 | (0.19–3.02) |
| Risk ASA≥3 | 1.31 | (0.68–2.54) | 1.83 | (0.77–4.36) |
| Previous anaesthesia | 1.07 | (0.47–2.43) | 0.83 | (0.32–2.15) |
| Which doctor performed informed consent | 1.91 | (0.97–3.76) | 1.24 | (0.57–2.69) |
| Received information about the risks of anaesthesiab | 4.84 | (2.12–11.02) | 4.00 | (1.32–12.10) |
| Was the language used during consent accessible?b | 2.47 | (1.09–5.58) | 1.38 | (0.49–3.87) |
| Considers information received to be sufficientb | 2.58 | (1.18–5.67) | 1.44 | (0.52–3.99) |
| Recalls risk related to anaesthesia and intubationb | 2.62 | (1.33–5.13) | 1.41 | (0.61–3.26) |
In bold: statistically significant data.
In a sample of patients who previously signed pre-anaesthesia consents, our results indicate that most patients reported having received sufficient information in an appropriate language and with the opportunity to ask questions about the process. However, questions that assessed the understanding or assimilation of the information demonstrated very poor retention; only 63% of patients knew about their planned intervention, and less than one-half of patients correctly answered more than 3 of the 4 questions assessed. This finding means that this informed consent met the 2 aspects highlighted by the Law of Patient Autonomy2: the obligation to disclose information and the obligation to obtain authorisation by the patient to perform the clinical intervention. However, the ultimate purpose of informed consent, as is clear from the Law, is to provide the patient with a decision tool, which is not feasible if the patient fails to understand and assimilate the information that is provided.
These results are consistent with those reported by the Hospital del Mar in 2007. This previous study consisted of 291 documented informed consent forms, and 133 patients were interviewed. Eleven percent reported not having received explanations, and only one-half of the patients admitted to fully understanding the risks and benefits.11 Other authors have also reported a low level of understanding and limited participation in the decision process.8,9 Advanced age and other factors that influence the ability of communication, such as education, level of education and ethnicity, may also have a significant impact on understanding and therefore the decision made concerning treatment.7 In our cases, neither age nor sex showed a significant influence. Additionally, although there was a slight difference in favour of those with university education levels in the crude analysis, after adjustment for potential confounders, only having received information on anaesthesia risks maintained an independent effect. In fact, our results place greater importance on the characteristics of the information provided than patient-related variables.
Although understanding is an important component of informed consent and greater attention has focused on the need to promote effective communication and patient understanding,7,8,12 there is no validated and widely accepted tool to evaluate patient understanding.5 This study used the retention of a series of variables related to anaesthesia included in the written document provided to the patient, and we assumed that there was a good understanding when we obtained at least 3 correct answers. We did not include general knowledge about the intervention, benefits or alternatives, which are dimensions identified by Schenker et al.6 for the evaluation of comprehension, because we were interested primarily in assessing knowledge about the risks of anaesthesia. It is assumed that the delivery of the text of the consent acts as positive reinforcement of verbal information, although it is possible that the difficulty associated with reading these documents prevents or at least limits this effect.13
Informed consent is more than a simple signature on a piece of paper14; it is a process that requires a competent physician, the appropriate transmission of information, sufficient time to discuss the pros and cons of the different alternatives that can be offered to the patient and the use of some form of feedback to ensure patient understanding of the information received.5,15 It is possible that the low level of comprehension revealed in our data was due to the lack of interaction between physician and patient or the consideration of informed consent as an administrative act with no more than a strictly legal significance.16 Despite systematically obtaining informed consent, one-half of the patients assessed were unaware of the risks associated with anaesthesia.
Our results demonstrate the need to contextualise the information provided during informed consent, not as a duty but as a tool to assist in patient information. The professional must take a proactive stance in assessing the understanding of information and understand this as a process that facilitates and strengthens the doctor-patient relationship and enhances the degree of adherence.
AuthorshipJosé Guillén-Perales participated in the conception of the work and has been responsible for the selection and inclusion of patients. As one of the parties involved in obtaining informed consent, he did not participate in data gathering, although he did actively participate in the analysis and interpretation of data and in drafting the manuscript.
Aurelio Luna-Maldonado led the work since its inception, contributing to the formulation of objectives and selecting the key to assessing the quality of information issues. Finally, he has participated in the revision of the various versions of the manuscript and has approved the final version.
María Fernández-Prada was responsible for collecting the information about treatments and performed the purification and analysis of the preliminary data. She also contributed to the literature search and drafting the manuscript.
José Francisco Guillén-Solvas and Aurora Bueno-Cavanillas led the data analysis and writing of the results and also participated in the literature review and final editing of the manuscript.
All authors have approved the final version of the manuscript.
Financial DisclosureNone.
Conflicts of InterestThere were no conflicts of interest.
We appreciate the collaboration of our colleagues in the anaesthesia unit and the patients who generously participated, allowing the collection of information necessary for the development of this work.
Please cite this article as: Guillén-Perales J, Luna-Maldonado A, Fernández-Prada M, Guillén-Solvas JF, Bueno-Cavanillas A. Calidad de la información en el proceso del consentimiento informado para anestesia. Cir Esp. 2013;91:595–601.
Part of the following results were presented as a poster at the XVII National and VI International Congress of the Spanish Society of Preventive Medicine, Public Health and Hygiene, which was held in Cartagena, June 5–7, 2013.