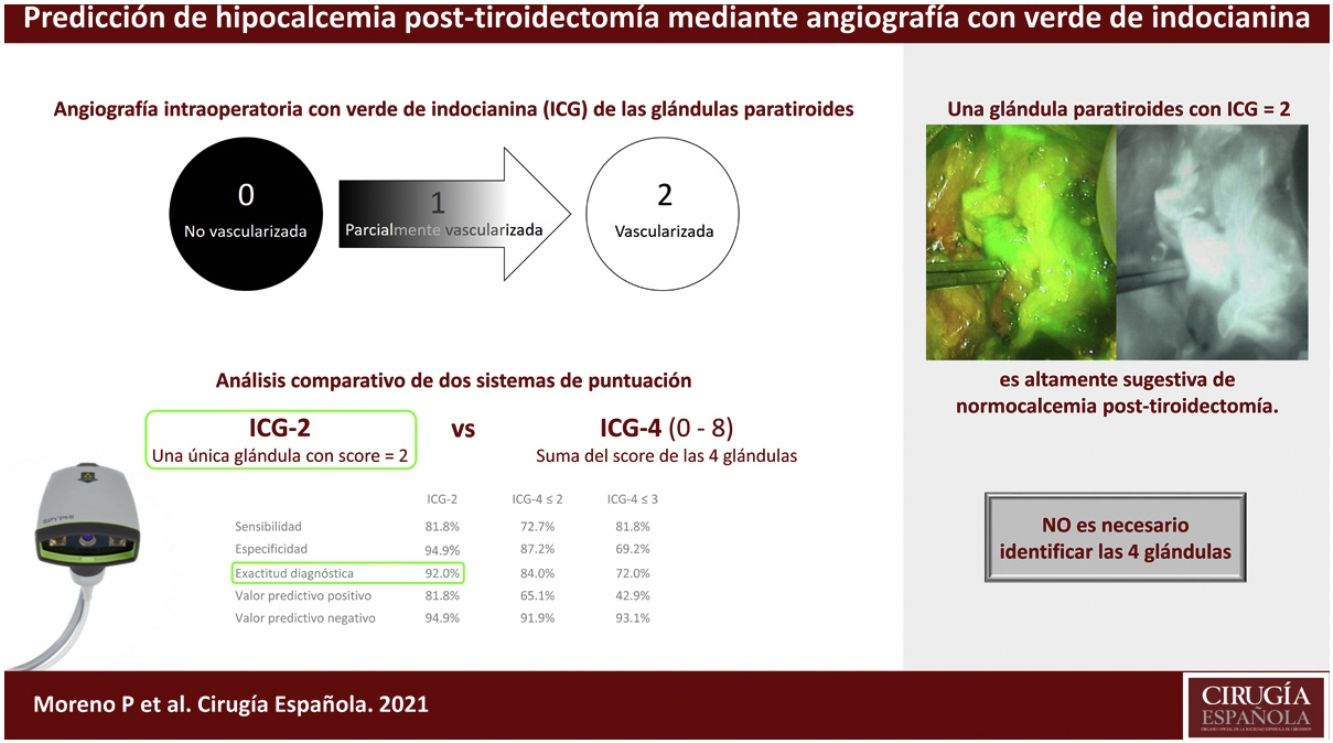
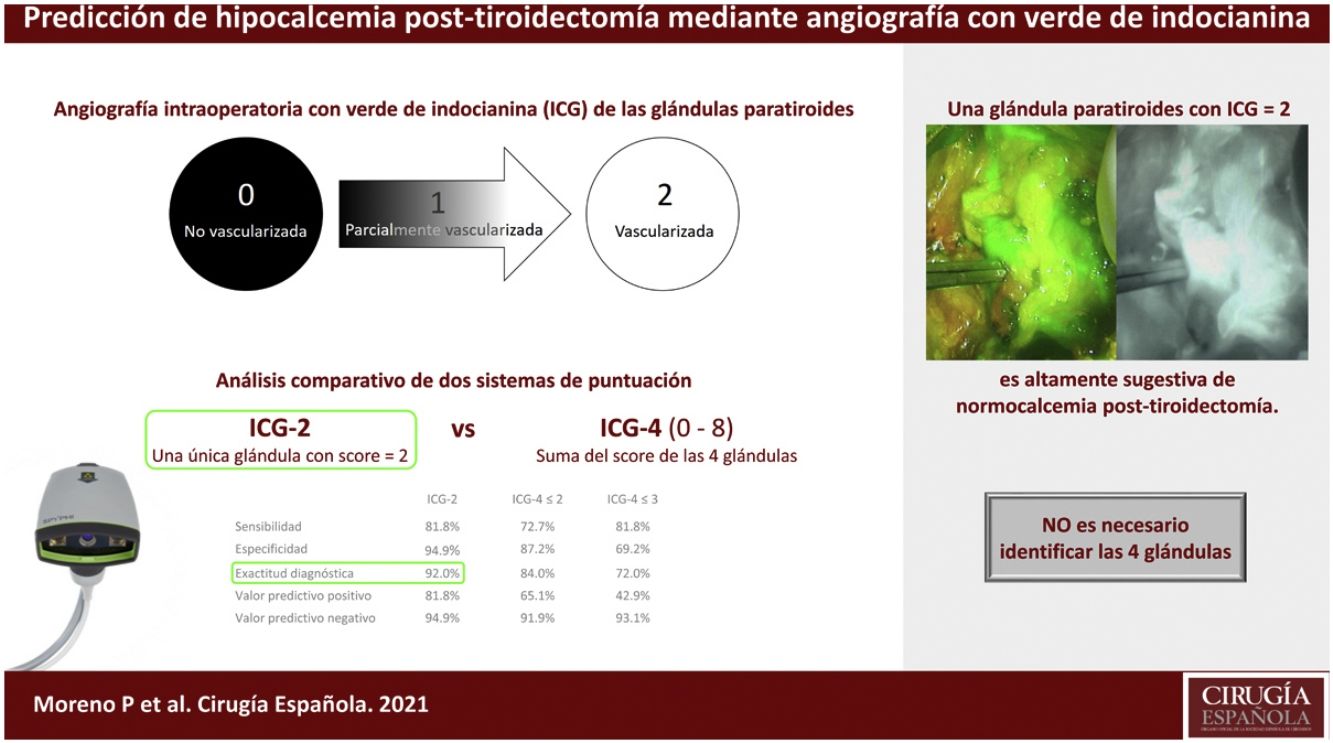
Indocyanine green (ICG) angiography of the parathyroids is useful in prediction of postthyroidectomy hypocalcemia. We compared the diagnostic accuracy of a single-gland ICG score of 2 with a score estimated by adding the viability value of the four glands (4-ICG).
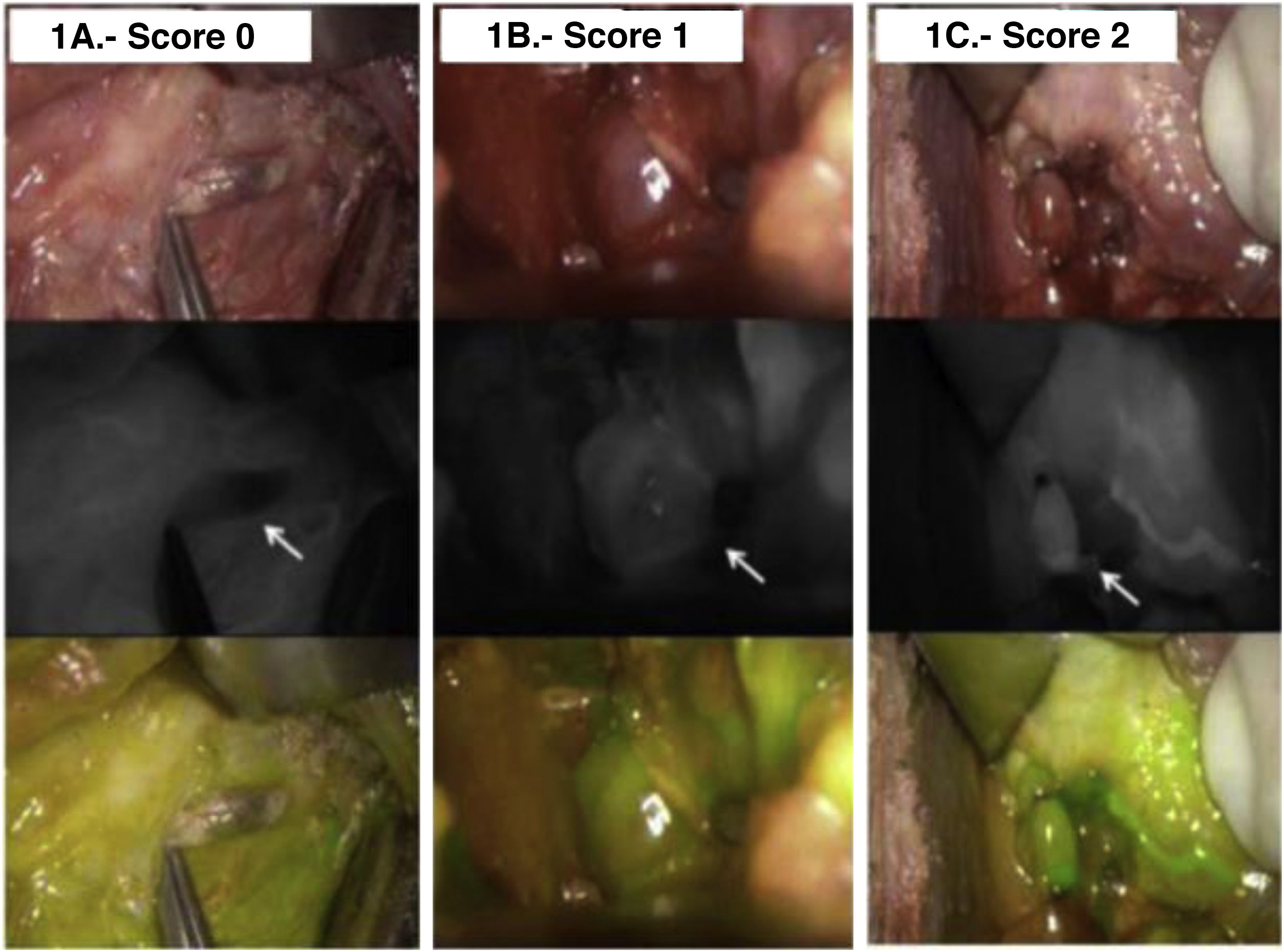
MethodsFifty patients (66% women, median age 49.4 years) underwent total thyroidectomy with identification of all 4 glands. The degree of ICG was classified as 0, black (nonvascularized), 1, gray/heterogeneous (partially vascularized), and 2, white (well vascularized).
ResultsThe diagnostic accuracy of the optimal cut-off of the 4-ICG sum score ≤3 was 84% (95% CI 70.9–92.8) lower than the diagnostic accuracy of 92% (80.8–97.8) of the ICG score 2. Both scores identified 2 false negative cases, but the rates of false positives were lower with the ICG score 2 (18.2% vs. 57.1%).
ConclusionsIdentification of single-gland ICG score of 2 has a higher diagnostic accuracy than 4-ICG sum score to predict immediate hypocalcemia after total thyroidectomy.
La angiografía de las glándulas paratiroides con verde de indocianina (ICG) es útil para predecir la hipocalcemia post-tiroidectomía. En este estudio se ha comparado la exactitud diagnóstica de una puntuación de la ICG de 2 con una puntuación estimada resultante de la suma del valor de viabilidad de las cuatro glándulas (ICG-4).
MétodosUn total de 50 pacientes (66% mujeres, mediana de edad 49,4 años) fueron operadas practicándose una tiroidectomía total con identificación de las 4 glándulas paratiroides. El grado de la ICG se clasificó como 0, color negro (no vascularizada), 1, gris/heterogéneo (parcialmente vascularizada) y 2, blanco (bien vascularizada).
ResultadosLa exactitud diagnóstica del umbral óptimo de la suma del ICG-4 de ≤3 fue del 85% (intervalo de confianza del 95% 70,9-92,8), inferior a la exactitud diagnóstica del 92% (80,8-97,8) del ICG-2. Con ambas puntuaciones se detectaron 2 casos de falsos negativos, pero las tasas de falsos positivos fueron menores con el ICG-2 (18,2% vs. 57,1%).
ConclusionesEl sistema ICG-2 predice con más exactitud la hipocalcemia post-tiroidectomía en el postoperatorio inmediato que el sistema ICG-4.
Intraoperative devascularization and damage to the parathyroid glands or parathyroid removal are frequently associated with early hypocalcemia after total or near total thyroidectomy. This complication that occurs in a variable percentage of patients, from less than 5% up to 49%1,2 increases the morbidity of thyroid surgery and the length of hospital stay. Transient hypoparathyroidism can become permanent in about 10% of patients, which results in the need of vitamin D and calcium supplementation for life, regular control visits, and increased risk of long-term complications.3,4 Therefore, there has been an increasing interest in the identification of predictors of postoperative hypoparathyroidism in patients undergoing extensive thyroid gland resection.
Perioperative measurement of parathyroid hormone (PTH) levels has been explored as an early predictive marker of the development of hypocalcemia after total thyroidectomy, but significant variation exists in the timing, type of assay, and thresholds of PTH in the literature. A recent systematic review of 69 studies comprising 9163 patients showed that studies of PTH parameters used to predict hypocalcemia are extremely heterogeneous, and that a priori definition of PTH thresholds is needed to ascertain the true prognostic significance of PTH in predicting postthyroidectomy hypocalcaemia.5 Also, PTH levels can monitor parathyroid function but cannot be used to assess the viability status of individual parathyroid glands during the surgical procedure. By contrast, intravenous angiography with indocyanine green (ICG) enables intraoperative real-time assessment of blood perfusion of the parathyroid glands according to the degree of ICG fluorescence on each gland, and emerging clinical experience reported so far has shown promising results.6–13
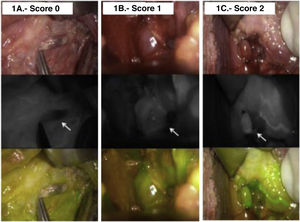
However, ICG angiography of the parathyroids is a relatively new technique and not known widely. It is usually assumed that only one working parathyroid gland is enough to maintain normocalcemia. Quantitative scoring systems based on a black and white scale depending on the amount of ICG flowing through the gland and categorized as 0, black (nonvascularized), 1, gray/heterogeneous (partially vascularized), and 2, white (well vascularized) have been successfully used for predicting early postoperative hypocalcemia after total thyroidectomy.12,13 Galvez-Pastor et al.12 showed that in patients with the four glands identified, a 4-ICG score calculated by adding the individual viability value of the four glands (range 0–8) showed a good discrimination in terms of predicting postoperative hypocalcemia. By contrast, in a previous study of our group it was found that a single-gland ICG score of 2 in any parathyroid gland was sufficient for accurate prediction of postoperative normocalcemia.13 Therefore, the primary objective of the study was to compare the diagnostic accuracy of a single-gland ICG score of 2 with the 4-ICG sum score to predict early postoperative hypocalcemia. A secondary objective was to define a more accurate cut-off point to predict hypocalcemia based on 4-ICG sum score.
MethodsDesign and participantsBetween May 2016 and October 2018, all consecutive patients diagnosed with thyroid diseases, the preferred treatment of which was elective total thyroidectomy, with or without central neck dissection, were included in a prospective cohort study. This was a single-center study carried out at the Endocrine Surgery Unit of an acute-care teaching hospital in L’Hospitalet del Llobregat, Barcelona, Spain. Inclusion criteria were identification of 4 parathyroid glands intraoperatively or if the sum of in situ glands plus autotransplanted plus those in the histopathological report was at least 4. Patients with previous thyroid and/or parathyroid surgery and those receiving calcium pills preoperatively were excluded. The study protocol (code ICG01) was approved by the Clinical Research Ethics Committee of Hospital Universitari de Bellvitge, and all patients gave written informed consent.
ICG angiography and viability of parathyroidsThyroid surgery was performed by a senior endocrine surgeon (P.M.Ll.) using a standard protocol of total thyroidectomy, with attention to prevent incidental parathyroidectomy or devascularization of the glands. Systematic search for parathyroid glands during total thyroidectomy was done. Also, once the thyroid specimen had been removed, it was actively searched for parathyroid glands, which were then prepared for reimplantation if needed. After the thyroid gland had been removed, ICG angiography of parathyroids was performed as previously described.12 A powdered vial of 25 mg of ICG was diluted in 10 mL of sterile water, and then 3 mL was administered, with repeated doses allowed until a maximum of 5 mg/kg was reached. After 1−2 min approximately, ICG-enhanced fluorescence imaging of each parathyroid gland was acquired using a near‐infrared camera (SPY-PHI, Stryker Endoscopy, San Jose, CA, USA). A white and black near-infrared view was obtained.
The black and white imaging was analyzed intraoperatively by the operating surgeon (P.M.-Ll.) and the degree of fluorescence was classified according to the color of the gland, reflecting the degree of perfusion. The color of the gland can vary from black (suggesting that it is not vascularized and likely non-viable), to white (suggesting that it is well vascularized and viable). Accordingly, glands were categorized as 0, black (nonvascularized); 1, gray/heterogeneous (partially vascularized), and 2, white (well vascularized) (Fig. 1). Both autotrasplanted and parathyroid glands identified in the histological pathology report are devascularized and scored as 0. For the purpose of the present study, a 4-ICG sum score was calculated according to the sum of individual viability values assigned to each gland (range 0–8) as previously described by Gálvez-Pastor et al.12 False negative cases were defined as those patients with at least one well perfused gland (score = 2) showing hypocalcemia, whereas false positive cases occurred in patients with no gland scored 2 and presenting normocalcemia.
The serum calcium level was measured using a colorimetric assay (reference 8.60–10.00 mg/dL [to convert to millimoles per liter, multiply by 0.25]). Criteria for the administration of calcium were the presence of symptoms of hypocalcemia or calcium levels less than 7.20 mg/mL in asymptomatic patients. Serum calcium levels were measured daily at 7:30 a.m. from the first postoperative day and previous to calcium intake if prescribed.
Statistical analysisFor a previous study aimed to assess the diagnostic value of ICG score 2,13 the sample size of 49 patients was estimated looking for a sensitivity (or specificity) of 85% of a single-gland ICG score 2 for the diagnosis of postoperative normocalcemia, with an alpha error of 0.05 and a maximum marginal error (d) of 0.1. The final sample was rounded to 50 patients. Then, taking advantage of these series of 50 patients, the present study analyzed the usefulness of the 4-ICG sum score versus ICG score 2, as well as the cut-off value of ≤3 ICG score as described by Gálvez-Pastor et al.12 Categorical data are expressed as frequencies and percentages, and quantitative data as mean and standard deviation (SD) or median and interquartile range (25th–75th percentile). Qualitative variables were compared with the chi-square test or the Fisher’s exact test, and continuous data with the Student’s t test or the Mann–Whitney U test according to conditions of application (the normal distribution of variables was assessed using the Shapiro–Wilk test for normality). The predictive ability of the 4-ICG sum score for predicting postoperative hypocalcemia was evaluated using the receiver operating characteristics (ROC) curve and the area under the curve (AUC). The sensitivity, specificity, positive and negative predictive values were calculated, as well as the best cutoff point defined as the highest product of sensitivity and specificity, which was ≤3 in the original study of Galvez-Pastor et al.12 and ≤2 when the 4-ICG sum score was calculated in the present series. Accordingly, the diagnostic accuracy for the detection of early postoperative hypocalcemia was compared in the following groups: 4-ICG score, the single-gland ICG score of 2, and the cut-off values ≤3 and ≤2 of the 4-ICG sum score. The Cochran’s Q test was used to compare two groups of nominal data. Statistical significance was set at P < 0.05. The statistical analysis was performed using R software (version 3.6) (R Foundation for Statistical Computing, Vienna, Austria).
ResultsFifty patients (17 men, 33 women) with a median age of 49.4 years (range 43.1–60.6) underwent total thyroidectomy because of thyroid cancer (n = 35), multinodular goiter (n = 13), and Graves disease (n = 2). Central neck dissection was performed in 30 patients.
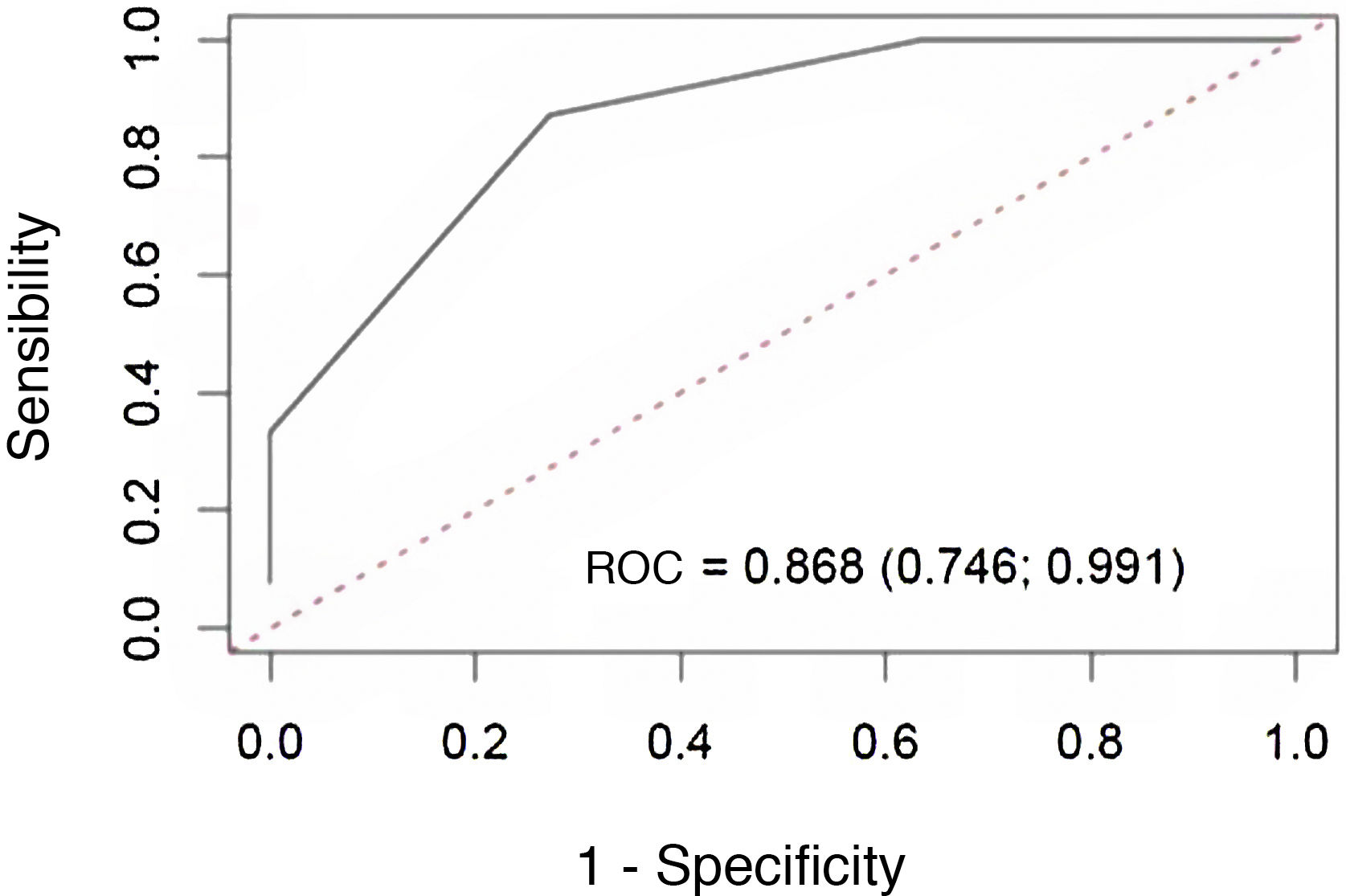
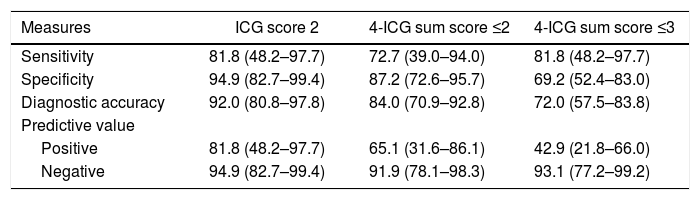
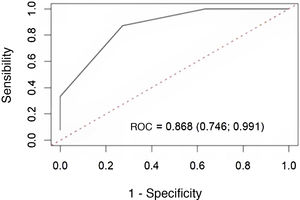
The median 4-ICG sum score was 4.0 (range 2.25–5.75). ROC curve analysis showed that the 4-ICG sum score had a good discrimination for predicting postoperative hypocalcemia (AUC = 0.868, 95% confidence interval [CI] 0.746–0.991) (Fig. 2). Using the ≤2 cut-off value, the diagnostic accuracy was higher than the 4-ICG score ≤3 (84% [95% CI 70.9–92.8] vs. 72% [57.5–83.8]), but lower than the diagnostic accuracy of 92% (80.8–97.8) of the single-gland ICG score of 2. As shown in Table 1, the sensitivity (82%), specificity (95%), positive predictive value (82%), and negative predictive value (95%) were also more favorable for the single-gland ICG score of 2 than for the cut-offs ≤2 and ≤3 of the 4-ICG sum score. Also, there were statistically significant differences in specificities between the single-gland ICG score 2 and the 4-ICG cut-off ≤3 (P < 0.0197).
Diagnostic accuracy of different cut-offs of intraoperative angiography with indocyanine green (ICG) of the parathyroid glands.
| Measures | ICG score 2 | 4-ICG sum score ≤2 | 4-ICG sum score ≤3 |
|---|---|---|---|
| Sensitivity | 81.8 (48.2–97.7) | 72.7 (39.0–94.0) | 81.8 (48.2–97.7) |
| Specificity | 94.9 (82.7–99.4) | 87.2 (72.6–95.7) | 69.2 (52.4–83.0) |
| Diagnostic accuracy | 92.0 (80.8–97.8) | 84.0 (70.9–92.8) | 72.0 (57.5–83.8) |
| Predictive value | |||
| Positive | 81.8 (48.2–97.7) | 65.1 (31.6–86.1) | 42.9 (21.8–66.0) |
| Negative | 94.9 (82.7–99.4) | 91.9 (78.1–98.3) | 93.1 (77.2–99.2) |
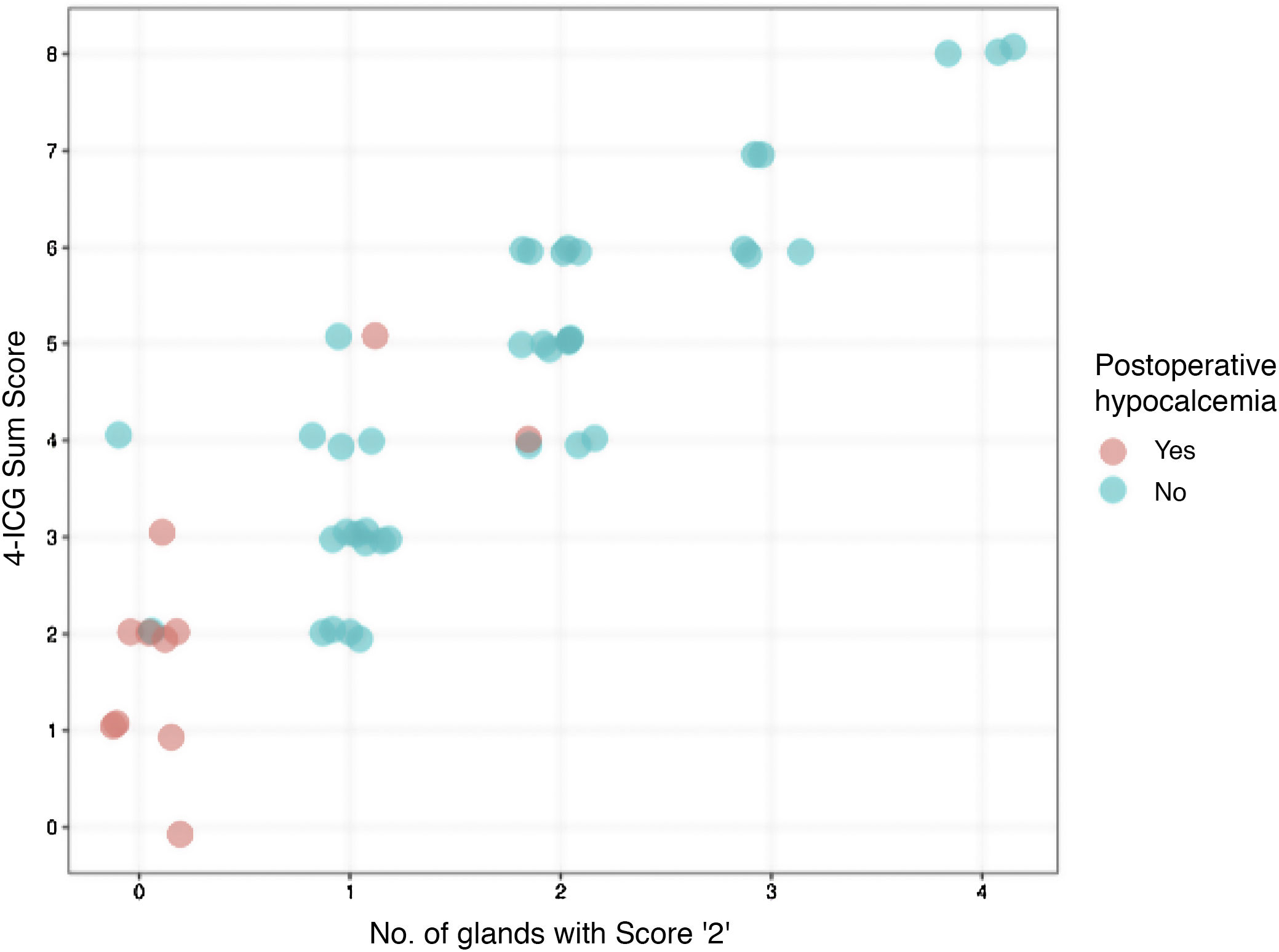
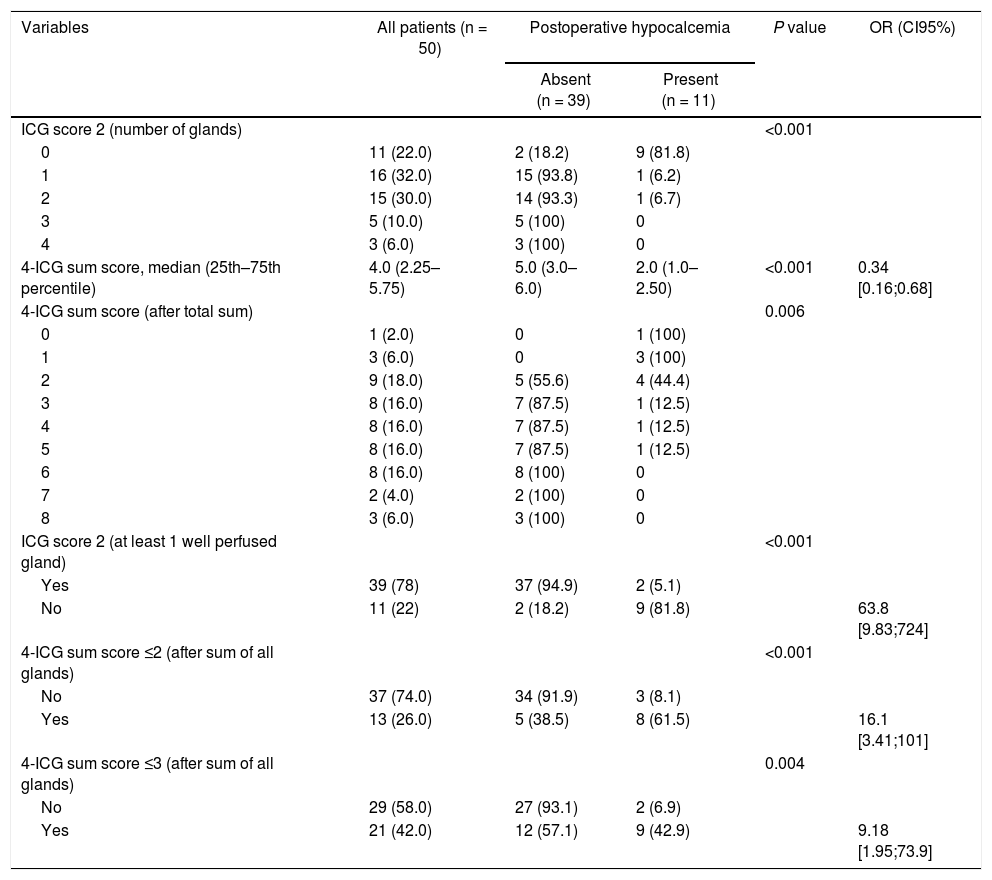
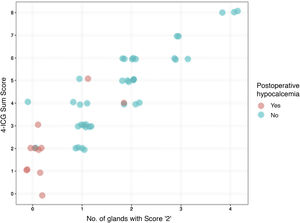
Calcium supplementation was required by 11 patients (22%) postoperatively. As shown in Table 2, the percentage of patients with hypocalcemia and a single-gland ICG score 2 were significantly lower than those with no gland scored 2 (5.1% vs. 81.8%, P < 0.001). Similarly, the need for calcium intake was significantly lower when negative vs. positive 4-ICG sum score ≤2 (8.1% vs. 61.5%, P < 0.001) as well as when negative vs. positive 4-ICG sum score ≤3 (6.9% vs. 42.9%, P = 0.004). Although both scores, the single-gland ICG score 2 and the 4-ICG sum score ≤3 coincided in the identification of 2 false negative cases, the single-gland ICG score 2 was superior to the 4-ICG sum score ≤3 in lower rate of false positives (18.2% vs. 57.1%). The comparisons of the performance of the single-gland ICG score 2 and the 4-ICG sum score in individual patients is shown in Fig. 3.
Distribution of patients according to results of intraoperative angiography with indocyanine green (ICG) of the parathyroid glands.
| Variables | All patients (n = 50) | Postoperative hypocalcemia | P value | OR (CI95%) | |
|---|---|---|---|---|---|
| Absent (n = 39) | Present (n = 11) | ||||
| ICG score 2 (number of glands) | <0.001 | ||||
| 0 | 11 (22.0) | 2 (18.2) | 9 (81.8) | ||
| 1 | 16 (32.0) | 15 (93.8) | 1 (6.2) | ||
| 2 | 15 (30.0) | 14 (93.3) | 1 (6.7) | ||
| 3 | 5 (10.0) | 5 (100) | 0 | ||
| 4 | 3 (6.0) | 3 (100) | 0 | ||
| 4-ICG sum score, median (25th–75th percentile) | 4.0 (2.25–5.75) | 5.0 (3.0–6.0) | 2.0 (1.0–2.50) | <0.001 | 0.34 [0.16;0.68] |
| 4-ICG sum score (after total sum) | 0.006 | ||||
| 0 | 1 (2.0) | 0 | 1 (100) | ||
| 1 | 3 (6.0) | 0 | 3 (100) | ||
| 2 | 9 (18.0) | 5 (55.6) | 4 (44.4) | ||
| 3 | 8 (16.0) | 7 (87.5) | 1 (12.5) | ||
| 4 | 8 (16.0) | 7 (87.5) | 1 (12.5) | ||
| 5 | 8 (16.0) | 7 (87.5) | 1 (12.5) | ||
| 6 | 8 (16.0) | 8 (100) | 0 | ||
| 7 | 2 (4.0) | 2 (100) | 0 | ||
| 8 | 3 (6.0) | 3 (100) | 0 | ||
| ICG score 2 (at least 1 well perfused gland) | <0.001 | ||||
| Yes | 39 (78) | 37 (94.9) | 2 (5.1) | ||
| No | 11 (22) | 2 (18.2) | 9 (81.8) | 63.8 [9.83;724] | |
| 4-ICG sum score ≤2 (after sum of all glands) | <0.001 | ||||
| No | 37 (74.0) | 34 (91.9) | 3 (8.1) | ||
| Yes | 13 (26.0) | 5 (38.5) | 8 (61.5) | 16.1 [3.41;101] | |
| 4-ICG sum score ≤3 (after sum of all glands) | 0.004 | ||||
| No | 29 (58.0) | 27 (93.1) | 2 (6.9) | ||
| Yes | 21 (42.0) | 12 (57.1) | 9 (42.9) | 9.18 [1.95;73.9] | |
Data as frequencies and percentages in parenthesis unless otherwise stated.
This study shows that the single-gland ICG score of 2 predicts parathyroid gland function in the immediate postoperative period better than the 4 ICG sum score, potentially avoiding exhaustive identification of parathyroid glands. The present results confirmed data of our previous study13 in which identification of at least one gland with an ICG score of 2 was suggestive of postoperative normocalcemia and no need of calcium supplementation. These results can be implemented easily in routine surgical practice.
The single-gland ICG score 2 has a higher diagnostic accuracy than a sum score of the viability values assigned to each individual gland based on the optimal cut-off value (4-ICG sum score ≤3) as reported in 32 patients in the previous study of Gálvez-Pastor et al.12 The overall 4-ICG sum score ranges from 0 to 8 but in the total sum value it is difficult to ascertain the actual number of viable glands, particularly in scores from 2 to 4. However, the optimal cut-off value of ≤3 cannot be considered indicative of the presence of viable glands (e.g. possible combinations of scores 0 and 1 in the four glands). In the original study of Gálvez-Pastor et al.12 this cut-off value showed a sensitivity, specificity, positive predictive value and negative predictive value for predicting postoperative hypocalcemia of 83%, 73%, 42% and 95%, respectively. In our present series of 50 patients, values of the 4-ICG sum score ≤3 were somewhat higher, but less favorable than the diagnostic accuracy associated with the single-gland ICG score 2 (92% [80.8–97.8] vs. 72% [57.5–83.8]).
The present results are consistent with other studies that have documented the usefulness of ICG angiography for in situ evaluation of parathyroid gland perfusion and function after thyroidectomy. In the study of Jin et al.7 of 26 patients in whom glands were scored from 0 to 2 on ICG angiography, postoperative PTH levels were in the normal range in 22 patients when at least one parathyroid gland with a single-gland ICG score of 2. In the four patients with no parathyroid gland with a single-gland ICG score of 2, two of them developed transient hypoparathyroidism.7
In the study of Vidal Fortuny et al.,10 146 patients with at least one well perfused gland on ICG angiograph (ICG score 2) were randomized to the intervention group (follow‐up assessment for symptoms of hypocalcaemia, no blood tests to determine calcium or PTH levels on postoperative day 1, and no oral calcium and vitamin D supplementation) or the control group (measurement of calcium and PTH levels on postoperative days 1 and 10–15, and systematic calcium and vitamin D supplementation until the first follow‐up appointment at 10–15 days). None of these patients presented with hypoparathyroidism, including those who did not receive calcium supplementation. However, 11 (22%) of the 50 excluded patients, in whom no well perfused parathyroid gland could be identified by angiography, presented with hypoparathyroidism, which was significantly different from the findings in randomized patients (P = 0.007).
Lang et al.6 reported 70 patients undergoing intraoperative ICG angiography after total thyroidectomy and the four glands were identified. Fluorescence light intensity cut-offs of 150% and 109% were established. No patients with a greatest fluorescent light intensity >150% developed postoperative hypocalcemia while 9 (81.8%) patients with a greatest fluorescent light intensity ≤150% did. Similarly, no patients with an average fluorescent light intensity >109% developed hypocalcemia while 9 (30%) with an average fluorescent light intensity ≤109% did. In a retrospective study of 210 patients who underwent total or near total thyroidectomy, ICG angiography was more accurate to guide autotransplantation compared with visual inspection, and there was a difference of having normal postoperative PTH levels when there were at least two normal parathyroids on ICG compared to those with less than two.14
Although the authors are aware that the sample size is an important limitation of the study, in agreement with previous data6,10–13 it seems that presence of one well perfused parathyroid gland using ICG angiography is a reliable way of predicting the absence of postoperative hypocalcemia avoiding the potential trauma associated to all parathyroid gland identification. Total thyroidectomy can be performed safely without the need of systematic calcium supplementation.
ConclusionThis study shows that identification of single-gland ICG score of 2 has a higher diagnostic accuracy than 4-ICG sum score to predict immediate hypocalcemia after total thyroidectomy. Besides, the diagnostic accuracy in prediction of early postthyroidectomy hypocalcemia of a single-gland ICG score 2 is superior to the best cut-off point derived from the 4-ICG score obtained by adding the individual viability scores of the four parathyroids.
FundingNo funding was received for this clinical study.
Authors’ contributionsP. Moreno Llorente: principal investigator, design de study, performed operations, collected and analyzed data, writing of the manuscript. A. García Barrasa, J.M, Francos Martínez, M. Alberich Prats and Mireia Pascua Solé: collected data and critically reviewed the manuscript. All authors have seen and approved the final draft.
Conflicts of interestNone to be declared.
The authors thank Bernat Miguel Huguet, PhD, for statistical analysis and Marta Pulido, MD, for editing the manuscript and editorial assistance.
Please cite this article as: Moreno Llorente P, García Barrasa A, Francos Martínez JM, Alberich Prats M, Pascua Solé M. Angiografía intraoperatoria con verde de indocianina (ICG) de las glándulas paratiroides para predecir la hipocalcemia postiroidectomía: análisis comparativo de 2 sistemas de puntuación (ICG-2 vs. ICG-4). Cir Esp. 2022;100:274–280.