The aim of our study was to analyze the short-term outcomes of laparoscopic surgery for a no medical responding ileocolic Cohn's disease in a single center according to the presence of obesity.
MethodsA cross-sectional study was performed including all consecutive patients who underwent laparoscopic resection for ileocecal Crohn's disease from November 2006 to November 2015. Patients were divided according to body mass index ≥30kg/m2 in order to study influence of obesity in the short-term outcomes. The following variables were studied: characteristics of patients, surgical technique and postoperative results (complications, reintervention, readmission and mortality) during first 30 postoperative days.
ResultsA total of 100 patients were included (42 males) with a mean age of 39.7±15.2 years (range 18–83). The overall complication rate was 20% and only 3 patients had an anastomotic leak. Seven patients needed reoperation in the first 30 days postop (7%). The median postoperative length of hospitalization was 5.0 days. Operative time was significantly longer in patients with obesity (130 vs 165min, P=.007) but there were no significant differences among the postoperative results in patients with and without obesity.
ConclusionsThis study confirmed that laparoscopic approach for ileocecal Cohn's disease is a safety and feasible technique in patients with obesity. In this last group of patients we only have to expect a longer operative time.
El objetivo de este estudio fue analizar los resultados postoperatorios de la cirugía laparoscópica por enfermedad de Crohn ileocecal en un único centro, en relación con la presencia de obesidad en los pacientes.
MétodosEstudio observacional y comparativo incluyendo a todos los pacientes consecutivos sometidos a cirugía electiva laparoscópica por enfermedad de Crohn ileocecal desde noviembre del 2006 hasta noviembre del 2015 en un único centro. Los pacientes se dividieron en 2 grupos con relación a si el índice de masa corporal fue inferior o no a 30kg/m2. Se estudiaron las características de los pacientes y de la técnica quirúrgica, y los resultados postoperatorios (complicaciones, reintervención, reingreso y mortalidad) durante los 30 días posteriores a la cirugía.
ResultadosSe incluyó a 100 pacientes (42 varones) con una edad media de 39,7 ± 15,2 años (rango 18-83). El porcentaje global de complicaciones fue del 20% y 3 pacientes tuvieron una dehiscencia de la anastomosis ileocólica. Siete pacientes requirieron reintervención en toda la serie (7%) y la estancia hospitalaria fue de 5 días. No hubo diferencias en los resultados entre ambos grupos pero los pacientes con obesidad requirieron un tiempo operatorio significativamente superior (130 vs 165 minutos, p=0,007).
ConclusionesEn nuestra experiencia, el abordaje laparoscópico en el tratamiento de la enfermedad de Crohn ileocecal es una técnica adecuada. La obesidad no es una contraindicación y no aumenta el número de complicaciones aunque prolonga significativamente el tiempo operatorio.
There is great variability in the prevalence of Crohn's disease in different European countries. While Great Britain has a reported incidence of between 5.9 and 11.1 cases per 100000 inhabitants, the rate in Spain is between 0.9 and 6.6 cases per 100000 inhabitants.1 This disease commonly affects the ileocecal area and, when medical treatment is not effective, or if complications appear, surgical treatment is indicated.2
Laparoscopy is the approach of choice in colon cancer. In the surgical treatment of ileocecal Crohn's disease, this approach has also been used for years.3–5 However, despite the fact that a meta-analysis has revealed the advantages of this approach,6 there are no long-term published series to provide information about some of the technical aspects, the results obtained and the most frequent complications.
Obesity is a medical and social problem with data indicating an epidemic increase in our setting.7 In the United Kingdom, this situation is particularly serious, possibly due to social factors and the impact of their diet.8 Although Crohn's disease usually presents with weight loss, the association between obesity and this disease has been increasing in daily clinical practice.9 Therefore, there is also a growing interest in determining how this comorbidity affects the surgical results of Crohn's disease.10,11
The objective of this study was to define the influence of obesity on the results of laparoscopic surgery in ileocecal Crohn's disease.
MethodsWe designed an observational, comparative study to retrospectively analyze the surgical technique and results (morbidity and mortality) of laparoscopic treatment for ileocecal Crohn's disease. Data for these variables had been prospectively recorded in a specialized colorectal surgery unit.
The study was approved as a clinical audit (according to current legislation) and all patients signed an informed consent form for the use of their data in this study.
The patients included were divided into 2 groups according to the presence or absence of obesity, defined as a body mass index (BMI) greater than 30kg/m2. The main objective was to determine the short-term outcomes (operative and morbidity/mortality results) and, therefore, the percentage of patients who experienced long-term disease recurrence was not included in this analysis.
We included patients with ileocecal Crohn's disease who underwent elective laparoscopic surgery in our unit during the study period. The indication for surgery was determined at the periodic multidisciplinary meeting of all the specialists involved in the management of these patients at our hospital (gastroenterologists, surgeons, radiologists and nutrition specialists). In all the included cases, histology studies confirmed the disease in the resected specimens. In our unit, a laparoscopic approach was indicated in all cases except those in which higher surgical difficulty is expected (based on the experience of the surgeon) due to the presence of previous abdominal surgery, previous intestinal resection due to Crohn's disease, or presence of a phlegmon-type inflammatory process. Patients who underwent emergency surgery or direct laparotomy (not after conversion) were excluded from the study.
Study VariablesWe analyzed the demographic, disease and operative data as well as the results of all consecutive patients who had been treated surgically for ileocecal Crohn's disease between November 2006 and November 2015.
The variables that had been recorded prospectively in the unit database, and were then analyzed, included the following: patient age, sex, BMI (kg/m2), anesthetic risk measured by the ASA scale, operative time, incision for the extraction of the surgical specimen and its size in centimeters, stoma, intraoperative blood loss, postoperative complications according to the Clavien–Dindo classification,12 reoperations and their causes, overall hospital stay and hospital readmission during the first 30 days post-op, and, last of all, mortality. Anastomotic dehiscence was defined as the discharge of intestinal luminal content at an anastomosis between 2 hollow viscera, which had been diagnosed: radiologically, with a water-soluble contrast enema or CT scan showing the presence of a purulent collection adjacent to the anastomosis; clinically, with evidence of extravasation of intestinal content or gas through the wound or drain; endoscopically; or, as a surgical finding during reoperation.13
Surgical Technique and Perioperative ManagementAll surgical interventions were performed directly by one of the 6 surgeons dedicated exclusively to colorectal surgery at our hospital or by properly supervised residents toward the end of their training period.
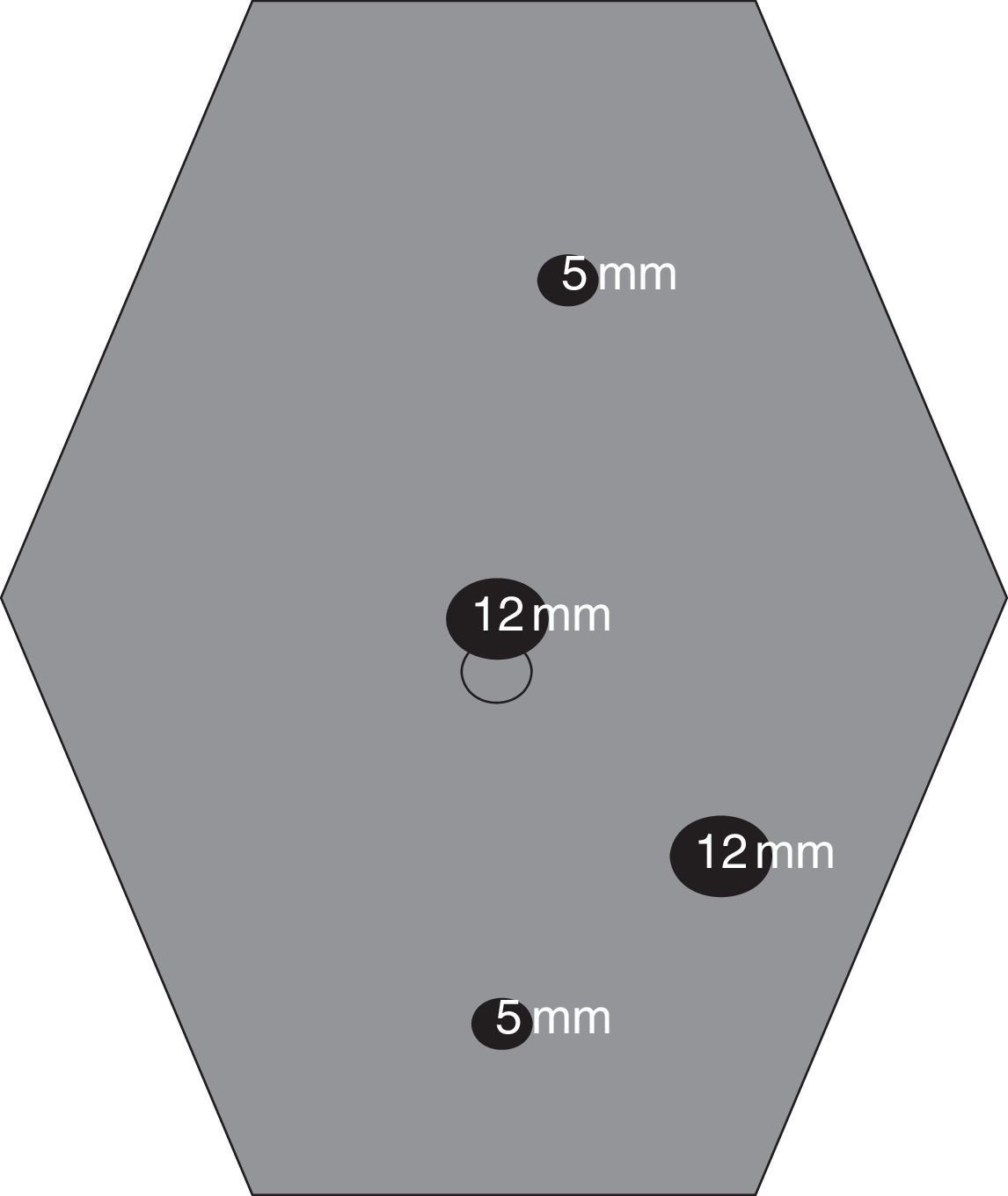
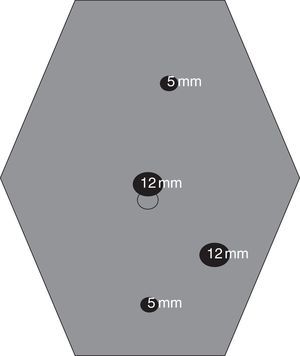
In our unit, which had been selected for participation in the laparoscopic surgery training program in Great Britain (LAPCO program14), the technique was standardized for teaching purposes and published.15 Except in unique cases, it involves the use of 4 trocars (Fig. 1) and usually a midline periumbilical assistance incision for the extraction of the surgical specimen. The anastomoses are created extracorporeally in most cases.
All patients were included in a postoperative multimodal rehabilitation program or Enhanced Recovery Program.16 Mechanical bowel preparation was not used, and intravenous antibiotic prophylaxis included gentamicin and metronidazole. Patients received prophylaxis for thromboembolic disease and initiated oral intake the same day of the surgical procedure. No intra-abdominal drainage was used.
Either an ileocolic anastomosis with or without a protective stoma or terminal ileostomy without anastomosis was performed depending on the patient's general condition and the local situation (small bowel wall edema, etc.). The ileocecal anastomosis was carried out with mechanical or manual suture, as decided by the surgeon. For the mechanical method, a side-to-side technique was used with an ileocecal mechanical suture (GIA® 80mm, Covidien, USA). At the discretion of the surgeon, hemostatic reinforcement of the anastomosis was performed with long-term absorbable monofilament suture (PDS®, Ethicon, Johnson & Johnson, USA). For manual suturing, the technique was end-to-end with interrupted 3/0 long-term absorbable sutures (PDS® Ethicon, Johnson & Johnson, USA or Vicryl® Ethicon, Johnson & Johnson, USA).
Statistical AnalysisThe data were collected prospectively in a database. Quantitative variables are presented with absolute numbers (and/or percentages), mean and standard deviation or median and range in parentheses. Quantitative variables were compared using Student's t test, after verification that the variable distribution followed the law of normality. The categorical variables were compared with the chi-squared test (or with Fisher's exact test when required from a statistical standpoint). Differences were considered statistically significant when the bilateral P-value was less than .05. The statistical analysis was carried out with the SPSS® version 21.0 software (IBM®, USA).
ResultsIncluded PatientsOut of 118 patients treated laparoscopically in the study period, a total of 100 consecutive patients (42 men) were included, with a mean age of 39.7±15.2 years (range 18–83) and a mean BMI of 24.9±5.3kg/m2 (range 16–42).
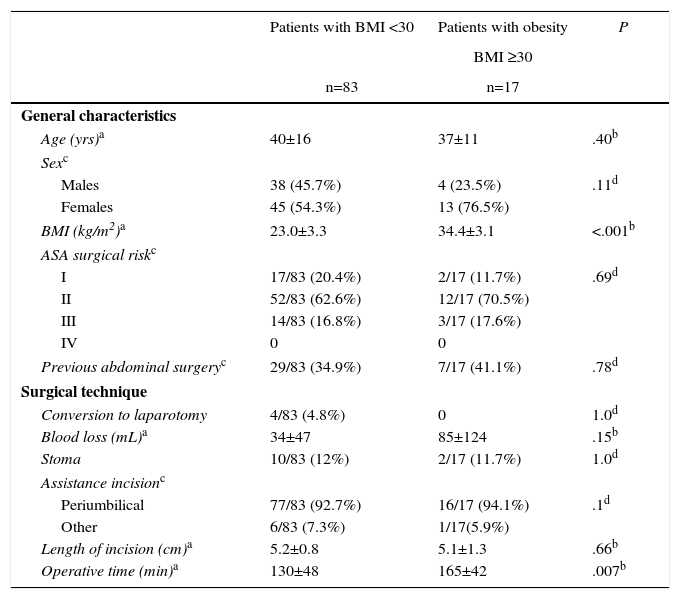
Table 1 shows the characteristics of the patients divided into 2 groups according to the presence of obesity. These data were similar between the two groups, with the exception of BMI (P<.0001). In 36 cases, there was previous abdominal surgery, involving previous gastrointestinal resection due to Crohn's disease in 18 (18%).
Characteristics of the Patients and Surgical Procedures in Both Groups.
| Patients with BMI <30 | Patients with obesity | P | |
|---|---|---|---|
| BMI ≥30 | |||
| n=83 | n=17 | ||
| General characteristics | |||
| Age (yrs)a | 40±16 | 37±11 | .40b |
| Sexc | |||
| Males | 38 (45.7%) | 4 (23.5%) | .11d |
| Females | 45 (54.3%) | 13 (76.5%) | |
| BMI (kg/m2)a | 23.0±3.3 | 34.4±3.1 | <.001b |
| ASA surgical riskc | |||
| I | 17/83 (20.4%) | 2/17 (11.7%) | .69d |
| II | 52/83 (62.6%) | 12/17 (70.5%) | |
| III | 14/83 (16.8%) | 3/17 (17.6%) | |
| IV | 0 | 0 | |
| Previous abdominal surgeryc | 29/83 (34.9%) | 7/17 (41.1%) | .78d |
| Surgical technique | |||
| Conversion to laparotomy | 4/83 (4.8%) | 0 | 1.0d |
| Blood loss (mL)a | 34±47 | 85±124 | .15b |
| Stoma | 10/83 (12%) | 2/17 (11.7%) | 1.0d |
| Assistance incisionc | |||
| Periumbilical | 77/83 (92.7%) | 16/17 (94.1%) | .1d |
| Other | 6/83 (7.3%) | 1/17(5.9%) | |
| Length of incision (cm)a | 5.2±0.8 | 5.1±1.3 | .66b |
| Operative time (min)a | 130±48 | 165±42 | .007b |
In the entire series, 4 cases were converted to laparotomy (total conversion 4%), all of them due to technical difficulty caused by the presence of abundant adhesions from previous surgeries. In the majority of patients, a periumbilical midline incision (93%) was used for the extraction of the resected specimen, and in 12 cases an ileostomy was performed after resection (8 end and 4 lateral ileostomies as “protection” of the ileocolic anastomosis, as the surgeon considered them at high risk for anastomotic dehiscence due to the treatment with elevated doses of steroids).
Total operative time was 136±48min (range 60–310). Table 1 summarizes the characteristics of the surgical intervention for both groups. The only statistically significant difference was prolonged operative time in patients with obesity (130min vs 165min, P=.007).
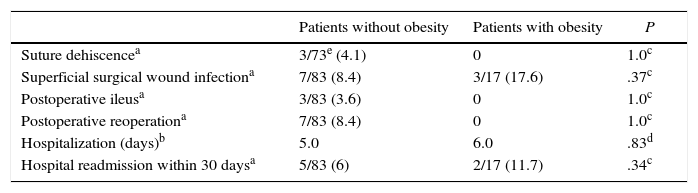
Postoperative ResultsIn the entire series, 20 patients had some type of complication (20%). Only 3 patients in the whole series (out of the 88 who underwent ileocolic anastomosis without a protective stoma) presented anastomotic dehiscence (3.4%). Seven patients required reoperation during the first 30 days post-op (3 for anastomotic dehiscence, 2 for intestinal obstruction due to adhesions and internal hernia, and 2 for hemorrhage). During the first 30 days post-op, 14 patients were treated in the emergency room for various reasons (14%) and 7 were readmitted to hospital (7%): one for intestinal obstruction, one for an intra-abdominal collection that required percutaneous drainage, one for late-onset anastomotic dehiscence, one due to superficial infection of the surgical wound and 3 due to abdominal pain without a clear cause at discharge.
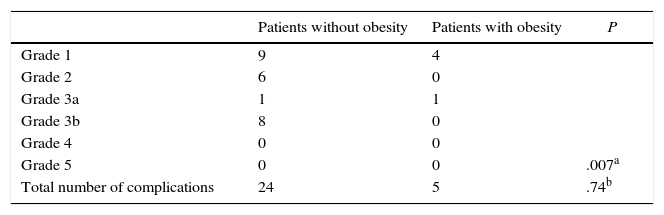
Median overall hospital stay was 5 days. Tables 2 and 3 summarize the most relevant postoperative data for each group, as well as all complications. There were no statistically significant differences between the two groups, except for the type of complications according to the Clavien–Dindo classification12 (P=.007). There was no mortality throughout the series.
Postoperative Results in Both Groups.
| Patients without obesity | Patients with obesity | P | |
|---|---|---|---|
| Suture dehiscencea | 3/73e (4.1) | 0 | 1.0c |
| Superficial surgical wound infectiona | 7/83 (8.4) | 3/17 (17.6) | .37c |
| Postoperative ileusa | 3/83 (3.6) | 0 | 1.0c |
| Postoperative reoperationa | 7/83 (8.4) | 0 | 1.0c |
| Hospitalization (days)b | 5.0 | 6.0 | .83d |
| Hospital readmission within 30 daysa | 5/83 (6) | 2/17 (11.7) | .34c |
The results of the present study suggest that obesity is not a contraindication for the laparoscopic approach of ileocecal Crohn's disease, as it does not increase the rate of complications. Nonetheless, operative times may be longer.
Our study describes a series with one of the largest numbers of cases treated with this surgical technique published in the literature. It is a direct result of the preferential dedication to minimally invasive surgery at our hospital. However, this study also has certain limitations. We were not able to analyze the effect of the presentation type of Crohn's disease, preoperative medication (e.g. immunomodulators) or preoperative blood work levels because these data did not form part of the variables studied. The objective of the study was to determine general postoperative results and the influence of obesity, since this is an increasingly frequent comorbidity in our environment.
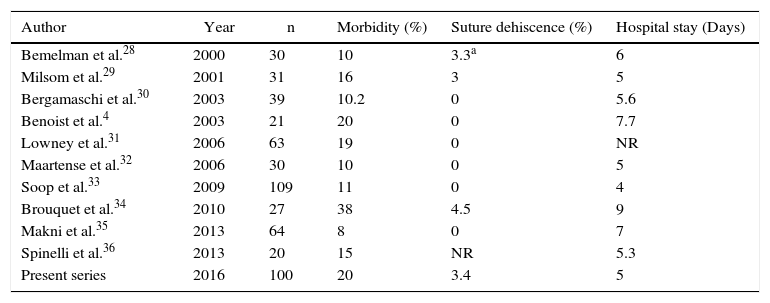
In this series, our conversion-to-laparotomy rate was 4%, and our percentage of anastomotic dehiscence was 3.4%. Table 4 summarizes the results of the different series published in recent years using the same surgical technique. When our results are compared with the different series published by experienced groups, it can be observed that conversion rates varied widely between 1% and 16%,6,17,18 and the percentage of dehiscence was between 0% and 4.5%.10,19 Also, in most series the hospital stay of these patients was around 5 days, as in our results.
Summary of the Results in the Published Series About the Laparoscopic Approach of Crohn's Disease in the Ileocecal Area.
| Author | Year | n | Morbidity (%) | Suture dehiscence (%) | Hospital stay (Days) |
|---|---|---|---|---|---|
| Bemelman et al.28 | 2000 | 30 | 10 | 3.3a | 6 |
| Milsom et al.29 | 2001 | 31 | 16 | 3 | 5 |
| Bergamaschi et al.30 | 2003 | 39 | 10.2 | 0 | 5.6 |
| Benoist et al.4 | 2003 | 21 | 20 | 0 | 7.7 |
| Lowney et al.31 | 2006 | 63 | 19 | 0 | NR |
| Maartense et al.32 | 2006 | 30 | 10 | 0 | 5 |
| Soop et al.33 | 2009 | 109 | 11 | 0 | 4 |
| Brouquet et al.34 | 2010 | 27 | 38 | 4.5 | 9 |
| Makni et al.35 | 2013 | 64 | 8 | 0 | 7 |
| Spinelli et al.36 | 2013 | 20 | 15 | NR | 5.3 |
| Present series | 2016 | 100 | 20 | 3.4 | 5 |
n: number of patients included; NR: no reported.
In any event, it is interesting to note that in 4 cases of our series we performed anastomoses with the protection of a lateral ileostomy, as is standard in some cases of lower anterior resection. While this technique is performed in many colorectal surgery units, it has been very rarely reported in the literature, especially after suture dehiscence.20,21 Although it is necessary to consider the possible complication of excessive hydroelectrolytic loss, it could contribute to minimizing the risk of anastomotic dehiscence in selected cases of ileocecal resection or even right hemicolectomy due to cancer.22
In our experience, obesity was not associated with either a higher conversion rate or more complications, even though operative times were significantly higher. These results are controversial, but other groups obtained the same conclusions in a non-homogeneous series including 93 cases of ileocecal involvement.23 In addition, in an elegant recent study, measuring body fat volume by CT proved to be a decisive factor for the presence of complications while it also influenced operative time.24
The results of our study were obtained in the setting of a specialized unit with extensive experience in laparoscopic surgery. In fact, our hospital was one of the participating institutions in the LAPCO laparoscopic surgery training program offered to specialists in colorectal surgery throughout Great Britain,14,15 which can be a determining factor for the results of this series.25
The influence of the laparoscopic approach on cancer outcomes in colorectal cancer has been a point of controversy for years.26 The influence of this approach on postoperative inflammatory phenomena and their possible effect on postoperative immune status has been a focus of attention and debate.27 Furthermore, we still do not know how these phenomena could influence long-term results in Crohn's disease. It would therefore be very interesting to observe the influence of this approach on disease recurrence results, so we are conducting a longitudinal, prospective study to find the answers to these questions.
In our experience, the laparoscopic approach in the treatment of ileocecal Crohn's disease is an appropriate technique. Obesity is not a contraindication and does not increase the number of complications, although it significantly prolongs the operative time.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Parés D, Shamali A, Flashman K, O’Leary D, Senapati A, Conti J, et al. Cirugía laparoscópica en el tratamiento de la enfermedad de Crohn del área ileocecal: impacto de la obesidad en los resultados postoperatorios inmediatos. Cir Esp. 2017;95:17–23.