The objective of this survey is to find out the cumulated experience and the current situation of video-assisted thoracic surgery (VATS) for anatomical lung resections in Spain.
MethodsThis is a descriptive study performed from two independent surveys designed through the Survey Monkey® web platform. The first survey was aimed at 53 thoracic surgery departments from the public and state-assisted national health system. The second survey, of a personal nature, was directed at 315 thoracic surgeons in active service, including physicians at their residency program. The surveys were kept operative from 18/11/2014 to 15/01/2015.
ResultsThe first survey was answered by 32 (60%) departments and the second by 167 (53%) professionals. A total of 29 (91%) of the thoracic surgery departments represented recognized having some level of experience in this technique. However, a great proportion of departments, 15 (52%), counted less than 100 procedures and the cumulated time of experience was lower than 5 years in 19 (66%) departments. Among all the individual respondents, 126 (77%) admitted having performed the procedure at some point. Of those without any experience, at least 36 (95%) of them recognized that future training in this technique is one of their future professional objectives.
ConclusionsWaiting for future prospective national registries contribute further information about the expansion of this technique in our country, the results of the current survey show, up to now, the best reflection of clinical practice and opinion of the surgeons involved in the development of VATS.
El objetivo de esta encuesta es conocer la experiencia acumulada y situación actual de la cirugía torácica video-asistida (VATS) aplicada a las resecciones pulmonares anatómicas en España.
MétodosSe realizó un estudio descriptivo a partir de 2 encuestas independientes a través de la plataforma Survey Monkey®. La primera encuesta se dirigió a 53 servicios de cirugía torácica de la red sanitaria pública y/o concertada nacional. La segunda encuesta, de carácter personal, se destinó a 315 cirujanos torácicos en activo, incluyendo médicos residentes. Las encuestas permanecieron activas desde el 18 de noviembre del 2014 hasta el 15 de enero del 2015.
ResultadosLa primera encuesta fue contestada por 32 (60%) servicios y la segunda por 167 (53%) profesionales. Un total de 29 (91%) de los servicios que colaboraron, reconocieron tener algún tipo de experiencia en esta técnica. Sin embargo, la mayor parte de los mismos, 15 (52%), habían realizado menos de 100 procedimientos y el tiempo de experiencia acumulado fue inferior de 5 años en 19 (66%) servicios. Del total de encuestados de forma personal, 126 (77%) admitieron haber realizado esta técnica en alguna ocasión. De aquellos sin ninguna experiencia, al menos 36 (95%) reconocieron que la formación en esta técnica quirúrgica es uno de sus próximos objetivos profesionales.
ConclusionesEn espera de que futuros registros prospectivos nos aporten más información sobre la expansión de esta técnica en nuestro país, los resultados de la actual encuesta representan el mejor reflejo de la práctica clínica y opinión de los cirujanos implicados en el desarrollo de la VATS.
Since Roviaro performed a pulmonary lobectomy by video-assisted thoracic surgery (VATS) for the first time in 1991, the evolution and the implementation of this surgical technique have been especially challenging.1
The main reason why VATS applied in anatomic lung resections has been so criticized, especially for the treatment of lung cancer, is due to its controversial oncological radicality. Other reasons that have limited its progression are its perception of being an unsafe surgical technique, having a demanding learning curve and consuming greater material resources and surgical times.2
However, over the last decade there have been several systematic reviews and meta-analyses that have granted VATS a clear advantage in terms of mortality and morbidity and potential oncological benefits in cases of tumors in initial stages.3–5 Despite such evidence, little is known about the actual implementation of this technique beyond the published results from the databases of the European Society of Thoracic Surgeons (ESTS) and the Society of Thoracic Surgeons (STS).6,7 According to data of the ESTS collected in its Database Annual Report from 2015, 4074 (22%) of the 18486 lobectomies registered between 2011 and 2014 were conducted with VATS.8
The objective of the present survey, promoted by the Scientific Committee of the Sociedad Española de Cirugía Torácica (Spanish Society of Thoracic Surgery, SECT), is to determine the accumulated experience and current situation of VATS applied to anatomical lung resections in Spain, as well as the opinions of professionals on some of the most controversial issues surrounding this technique.
MethodsA descriptive study was carried out based on data attained from 2 surveys. To obtain a true reflection of the nation-wide experience of individual surgeons and surgery services, these 2 surveys were independent. The internet platform used was Survey Monkey®, and e-mail was used to collect anonymous responses. The list of e-mail addresses was provided by the Technical Secretary of the SECT to R.E., coordinator of the Scientific Committee of the Society, on November 1, 2014. All information was treated confidentially, in accordance with the current Organic Law of Data Protection.
The first survey was addressed to a single individual in representation of a surgery department. To this end, we contacted the 53 thoracic surgery services of the Spanish public and/or subsidized hospital network. The survey was active from November 18 to December 15, 2014, during which time 2 e-mail reminders were sent on December 9 and 14. A total of 32 (60%) services responded to the questions, and 30 (57%) questionnaires were fully completed.
The second survey was sent to the 315 active professionals, including thoracic surgery residents (médicos internos residents, MIR) and specialists (facultativos especialistas de área, FEA), all members of the SECT as of November 1, 2014. The survey remained active from December 16, 2014 to January 15, 2015, and 3 electronic reminders were sent on December 22nd and January 8th and 14th. The questionnaires were answered and returned by 167 (53%) individuals, and in 157 (50%) cases the surveys were completed in their entirety.
The results were expressed as valid percentages; in order to establish relationships between the answers to different questions, exclusion and comparison filters were used on the web platform. The concept of “VATS anatomical lung resection” was determined by the absence of rib retraction, regardless of the number of incisions and type of surgical material used, as well as by the individualization and division of all vascular elements and corresponding bronchus (although in anatomical segmentectomies individualized division of the segmental vein or veins was not considered essential). The pulmonary resections that were contemplated included: pneumonectomy, bilobectomy, lobectomy and anatomical segmentectomy.
Survey for Surgery Services (S)- (S1)
What is the approximate number of VATS anatomical lung resections performed by your surgery department to date?
- (S2)
Assuming your service has accumulated experience, how long ago did your department perform its first VATS anatomical lung resection?
- (S3)
Currently, what proportion of anatomical lung resections are performed with VATS in your department?
- (S4)
How many FEA fellows in your surgery service perform this technique as primary surgeon?
- (S5)
Regarding the training in this technique for MIR residents in your department, which of the following statements do you feel are correct?
- (P1)
What is your professional experience?
- (P2)
Approximately how many VATS anatomical lung resections have you conducted entirely by yourself to date?
- (P3)
If the previous answer was “None,” what are the reasons for this?
- (P4)
What are the training resources that you have utilized, regardless of your experience in this technique?
- (P5)
Compared with the thoracotomy approach, what is your opinion of VATS for the systematic lymph node dissection of the mediastinum in lung cancer?
- (P6)
How many incisions do you usually make?
- (P7)
If you do have experience in this technique, in which of the following advanced VATS procedures do you have experience?
- (S1)
A total of 32 (60%) services indicated their experience in this surgical technique. Of these, 3 (9%) services admitted that they had not performed any VATS procedures, 10 (31%) had experience with less than 50 cases, 5 (16%) between 50 and 100 cases, 7 (21%) between 100 and 200 cases, and 7 (21%) reported more than 200 procedures.
- (S2)
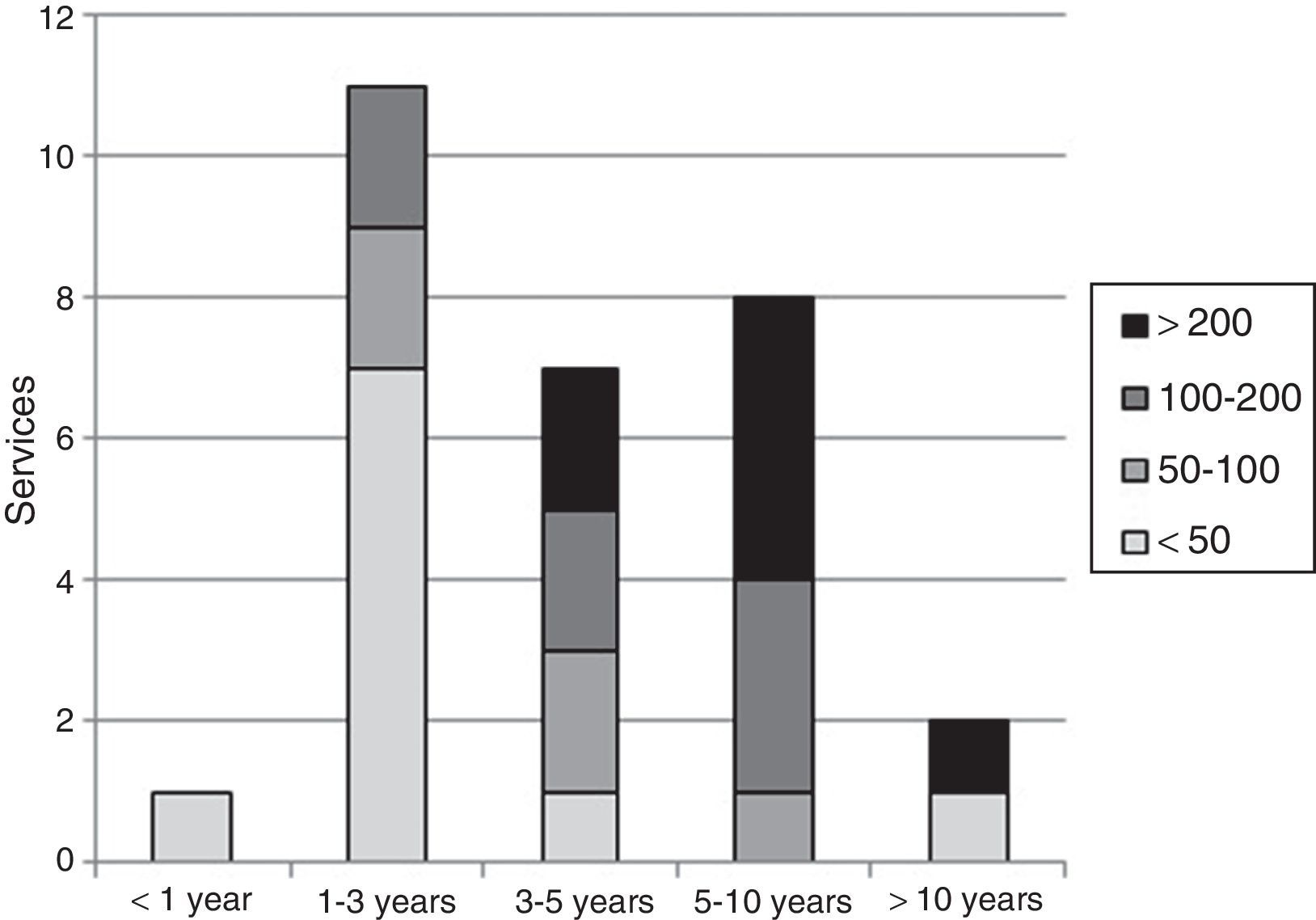
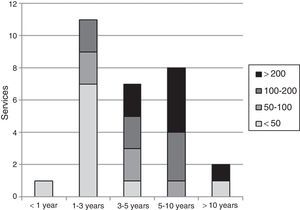
As for those departments that had performed VATS procedures, the accumulated experience times since the first case were: 1 (3%) less than one year, 11 (38%) between 1 and 3 years, 7 (24%) between 3 and 5 years, 8 (28%) between 5 and 10 years, and 2 (7%) more than 10 years (Fig. 1).
- (S3)
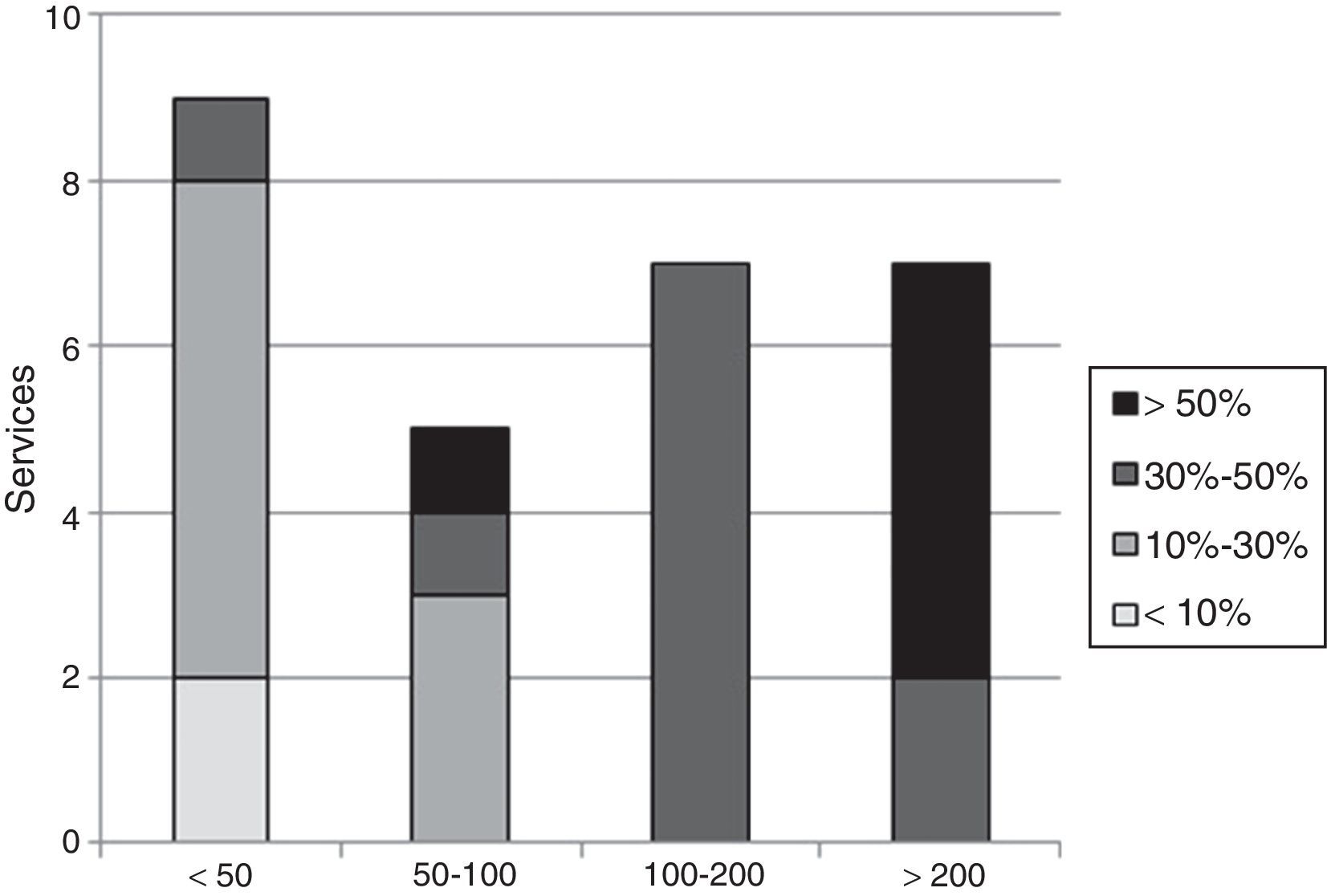
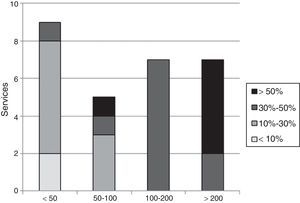
The distribution of surgery departments that indicated the percentage of procedures performed using VATS was: 2 (7%) services 0% of cases; 2 (7%) less than 10%; 9 (30%) between 10 and 30%; and 6 (20%) services more than 50% of cases (Fig. 2).
- (S4)
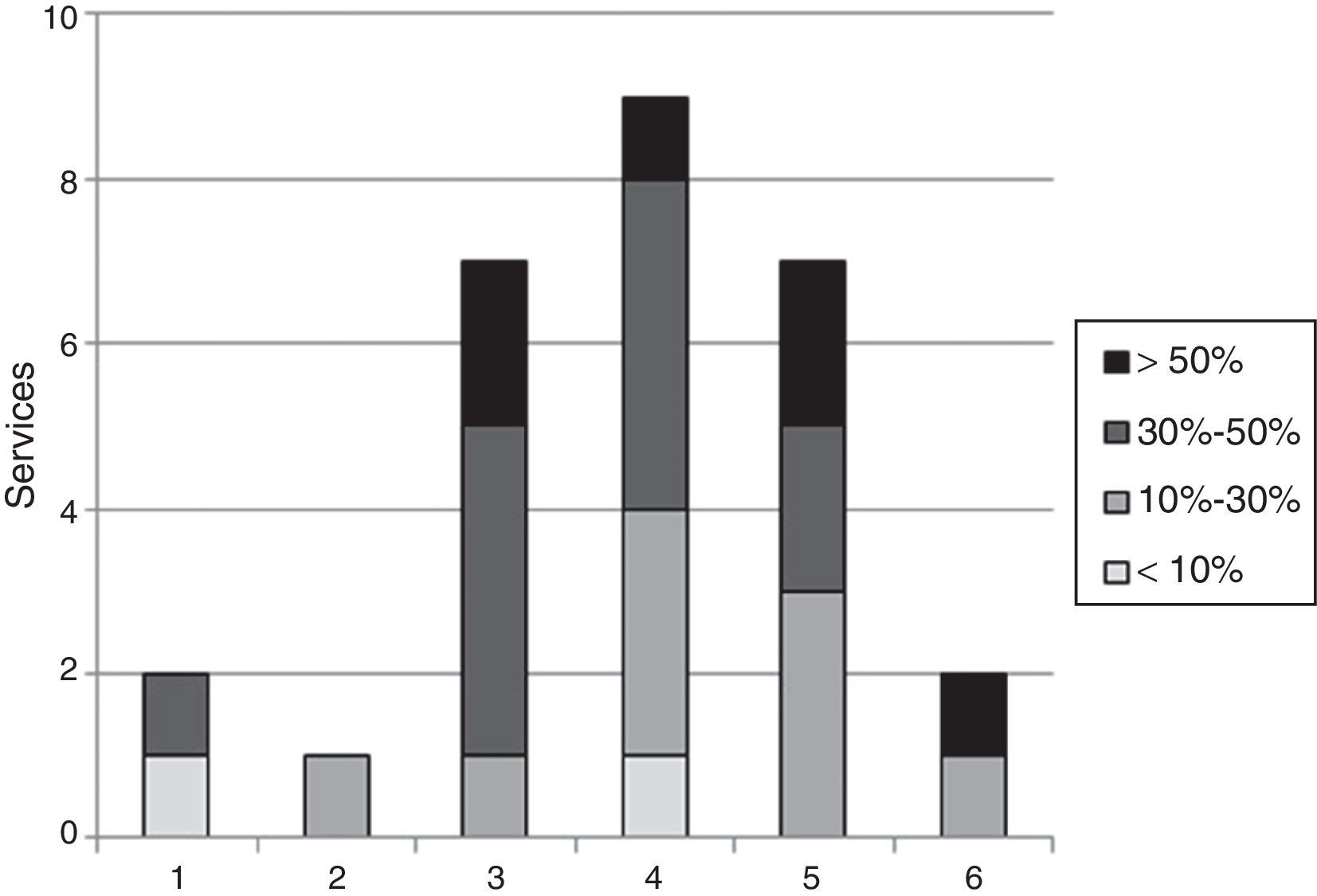
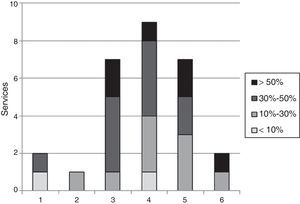
Regarding the number of specialists (FEA) who perform this procedure in each service, and after excluding those departments with no experience according to the responses of question S1, the distribution was as follows: in 2 (7%) departments, one FEA; in 2 (7%) services, 2 FEA; in 7 (24%) services, 3 FEA; in 9 (31%) services, 4 FEA; in 7 (24%) services, 5 FEA; and in 2 (7%) services, 6 FEA (Fig. 3).
- (S5)
A total of 30 surgery services expressed their opinion about MIR resident training in this technique. In 19 (63%) departments, residents performed this procedure as part of one of their teaching objectives, while 11 (37%) services considered that training in this technique should be dependent on adequate experience in open surgery. In 7 (23%) of the services, residents only participate as assistants in this technique, while 4 (13%) services admitted that they lacked teaching certification.
- (P1)
The distribution by experience of the 167 participating thoracic surgeons was: 38 (23%) MIR residents; 75 (45%) FEA specialists for less than 10 years; 28 (17%) FEA for 10 to 20 years; 18 (11%) FEA for 20 to 30 years; and 8 (5%) FEA for more than 30 years.
- (P2)
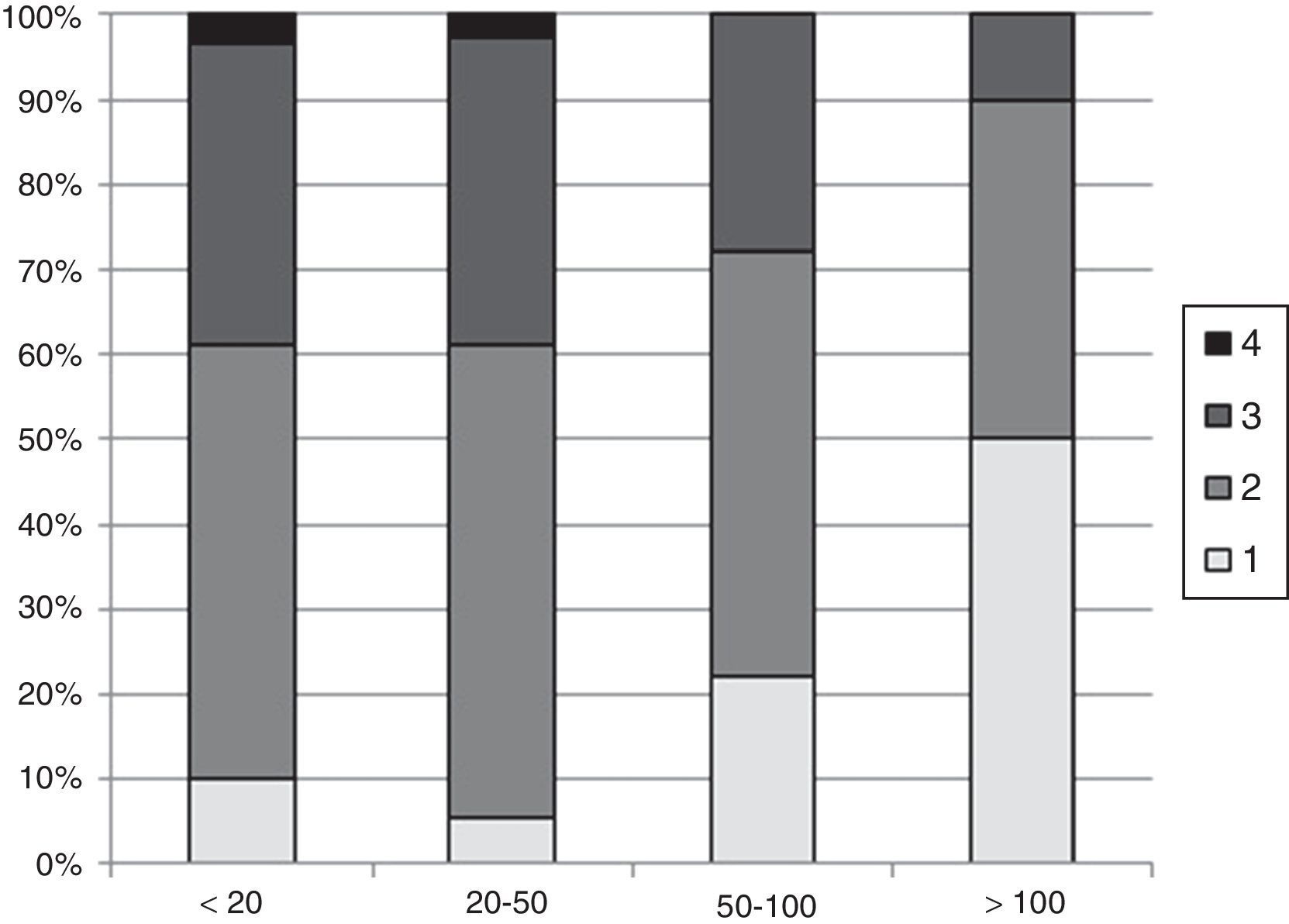
As for the number of VATS anatomical lung resections, a total of 164 responses (3 omissions) were received: 38 (23%) professionals admitted not having performed any procedures; 60 (37%) less than 20 cases; 36 (22%) between 20 and 50 cases; 20 (12%) between 50 and 100 cases; and 10 (6%) more than 100 cases.
- (P3)
Regarding the reasons given by the surgeons who had no experience in the VATS technique: 36 (95%) considered it necessary to complete their training; 5 (13%) surgeons admitted that some of their colleagues were opposed; 2 (5%) surgeons acknowledged a lack of interest or motivation; and 2 (5%) considered that there was not enough scientific evidence in favor of this technique.
- (P4)
The most frequently used training resource entailed attending live surgery and/or experimental surgery courses, in which a total of 122 (75%) surgeons had participated. The distribution of professionals according to the rest of the resources was: 44 (27%) training at national medical centers; 37 (23%) visits to foreign medical centers; and 16 (10%) other resources.
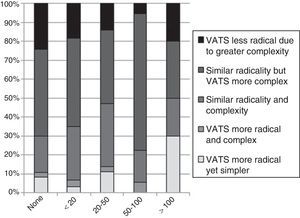
- (P5)
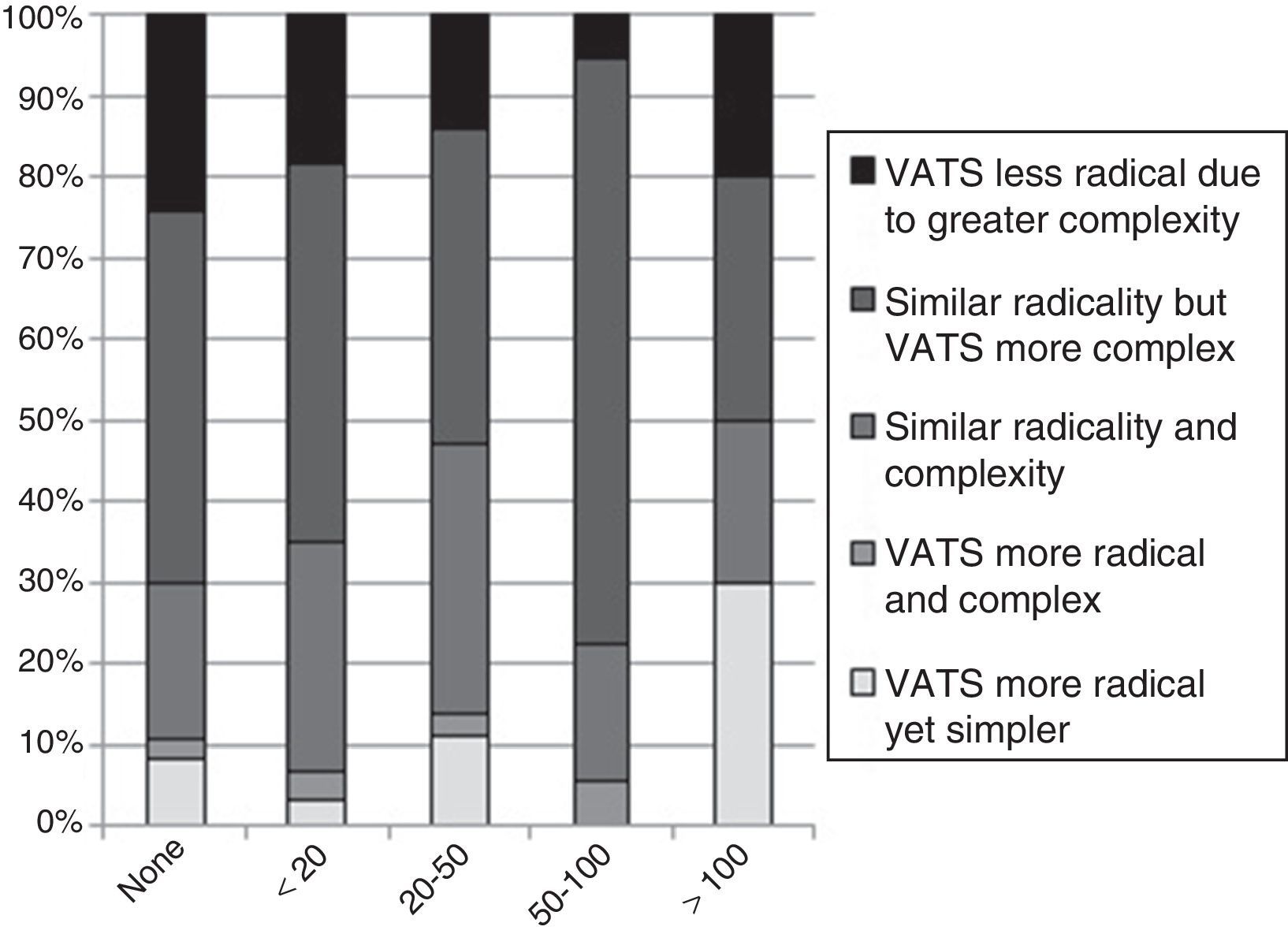
With regard to one of the most controversial aspects of VATS, lymphadenectomy, 75 (47%) professionals considered that VATS, although technically more complex, is equivalent to thoracotomy in terms of its oncological radicality. For 41 (25%) professionals, VATS and thoracotomy are comparable in radicality and technical difficulty. Another 28 (17%) thoracic surgeons considered that VATS is less radical due to its greater technical complexity. In contrast, 12 (7%) professionals stated that VATS is more radical and simple to perform, while another 5 (3%) consider VATS to be more radical although technically more complex (Fig. 4).
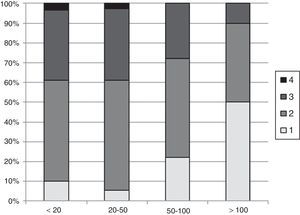
- (P6)
Regarding the number of incisions, the distribution of responses was as follows: 20 (14%) single incision; 72 (50%) 2 incisions; 48 (33%) 3 incisions; and 4 (3%) 4 incisions (Fig. 5).
- (P7)
The experience of individual surgeons in potentially more complex procedures than standard VATS lobectomy was: 60 (38%) anatomic segmentectomy; 22 (14%) pneumonectomy; 16 (10%) angioplasty and/or partial bronchoplasty; and 4 (3%) angioplasty and/or sleeve bronchoplasty. A total of 69 (44%) professionals stated they had not performed any of the mentioned procedures.
Although more than 20 years have elapsed since the first major VATS lung resection was performed in Spain by Loscertales et al., the true diffusion and implementation of this surgical technique took place in our country just over 5 years ago.9 Currently, the main clinical practice guidelines consider VATS the surgical technique of choice for the treatment of lung carcinoma in its initial stages.10,11 However, little is known about its actual implementation and the current opinion of thoracic surgeons and residents of the specialty about this surgical approach. Moreover, the limited international references in the literature refer to surveys carried out almost 20 years ago among specific collectives or at a non-national level.2,12 Therefore, any comparison with our results should be interpreted with caution.
One of the first surveys about the applicability and future of VATS was conducted by Mack et al. in 1996. The results of this survey, answered by 189 (83%) of the 229 members of the General Thoracic Surgery Club, reflected how 84% of the respondents considered, at that time, that VATS lobectomy was either an unacceptable technique or one in research phase.2
In 2012, Cao et al. conducted an international survey, in which a total of 838 (7.82%) thoracic surgeons participated out of the 10704 surgeons contacted. Of these, 422 (50.35%) admitted having some experience in VATS or robotic lobectomy as a form of lung cancer treatment. This percentage was nearly identical when only the group of European thoracic surgeons was considered: 148 (48.5%) out of 305. In our case, this figure was significantly higher, since 126 (77%) of the 164 thoracic surgeons and MIR residents contacted reported having performed procedures. However, in agreement with our results, 381 (92%) of the 416 surgeons with no experience in the study recognized that training in this technique was one of their future objectives.13 Along this line, it is noteworthy that in our country a very important proportion of surgeons have decided to complete their training in this technique by attending practical courses (75%), while others by means of internships at national (27%) and international (23%) medical centers.
Another important aspect related to the learning of this technique was the high percentage of respondents (63%) who declared that one of their objectives was that MIR should perform this technique during their training period. In addition, one of the classically accepted premises of adequate training in open surgery before training in video-assisted surgery was only supported by 37% of the respondents. In 2012, Boffa et al. published the results of a survey of 271 recently graduated American cardiothoracic surgeons who completed their specialization between 2006 and 2008. This survey, which sought to determine the self-reported domain of VATS lobectomy among respondents, was completed by 74 (88%) of the 84 participating general thoracic surgeons. Of these, a remarkable 86% acknowledged feeling competent in this surgical technique at the end of their residency at that time.14
As it is a nation-wide study, one interesting datum of our survey is the implementation of this technique by surgery services. Although 29 (91%) of the 32 participating surgery departments reported having performed VATS procedures, the actual percentage is likely to be relatively less, since it is presumed that lack of participation is related with inexperience or lack of interest in this technique. Taking into account that the survey was sent to 53 representatives of other services, we can conclude that at least 29 of the 53 (55%) had some experience in this surgical technique. Therefore, and with caution, we could estimate an actual percentage between 60% and 70% of surgery services nation-wide.
Although a significant proportion of the departments with some experience reported a limited number of cases (15 [52%] services less than 100 procedures) and time elapsed since the first procedure (19 [66%] services less than 5 years), it is noteworthy that in 17 (61%) and 6 (21%) of the services the proportion of VATS anatomical resections surpassed 30% and 50%, respectively. It is also worth noting that 89 (56%) of the professionals admitted having already performed potentially more complex procedures than the standard VATS lobectomy. As for the number of incisions, the biportal technique is the most commonly used (72 [50%]), while the single-port is utilized by only 20 (14%) professionals. In this context, as Gonzalez-Rivas et al. have published, these percentages are likely to increase in the future along with the experience of each hospital and surgeon.15
While we wait for the upcoming national prospective registry of anatomical lung resection by SECT to provide us with more information about the nation-wide clinical practice in this surgical technique and its implications, the results of this present survey are, to date, the truest reflection of the accumulated experience and opinions of surgeons involved in the future of video-assisted thoracic surgery in Spain.
FundingNo grants or other aid were received for the development of this manuscript.
Authorship- –
Study design: R. Embún, N. Martínez, S. Call, B. Olaiz, J. Zabaleta, R. Ramos
- –
Data acquisition: R. Embún
- –
Analysis and interpretation of the results: R. Embún, J. Galbis, N. Moreno
- –
Article composition: R. Embún
- –
Critical review and approval of the final version: N. Martínez, S. Call, B. Olaiz, J. Zabaleta, R. Ramos, J. Galbis, N. Moreno
The authors have no conflict of interests to declare.
We would like to thank all the thoracic surgeons who have collaborated, either in their own name or in representation of their surgery service, to make this survey study possible.
Please cite this article as: Embun R, Martínez Hernández N, Call S, de Olaiz Navarro B, Zabaleta J, Ramos R, et al. Cirugía torácica video-asistida y resecciones pulmonares anatómicas. ¿Dónde estamos? Encuesta nacional de la Sociedad Española de Cirugía Torácica. Cir Esp. 2017;95:24–29.
The results of this survey were presented at the 6th Conference of the Sociedad Española de Cirugía Torácica (Spanish Society for Thoracic Surgery) held on May 13–15, 2015, in Seville, Spain.