Bariatric surgery is becoming more and more common, and Roux-en-Y gastric bypass is one of the most widely used procedures today. It is well known that patients who undergo gastric bypass to treat obesity have a higher risk for cholelithiasis and choledocholithiasis.1 The rates of postoperative detection of gallstones can range between 22% and 71%, and cholecystectomy can be required in 7%–41% of patients who have undergone gastric bypass.2 Out of these patients, a very small percentage can have associated choledocholithiasis. We could say that the development of choledocholithiasis after gastric bypass is uncommon, although possible, and endoscopic exploration of the bile duct is technically challenging in this type of patients.3
In cases which are not accessible by standard endoscopy, as in the case of gastric bypass, transgastric endoscopic retrograde cholangiopancreatography assisted by laparoscopy could be a strategy to consider4 if the bile duct is not dilated or if there are no large gallstones embedded in the common bile duct, as in our case. The transcystic approach would be another valid option in these situations.
We propose a simple technique for the management of choledocholithiasis in patients who have undergone gastric bypass for morbid obesity that combines laparoscopic cholecystectomy with endoscopic retrograde cholangiopancreatography through a gastrostomy. The endoscope is inserted4 through a 15mm transgastric balloon trocar for obesity to access the papilla through the gastric remnant. This enables the surgeon to carry out sphincterotomy and the extraction of common bile duct calculi. As choledochotomy is not done, nor is a drain left in the bile duct, the technique is much simpler and much less aggressive. This is consequently beneficial for the patients’ progress, who are able to go home 24h later without any drain tubes.
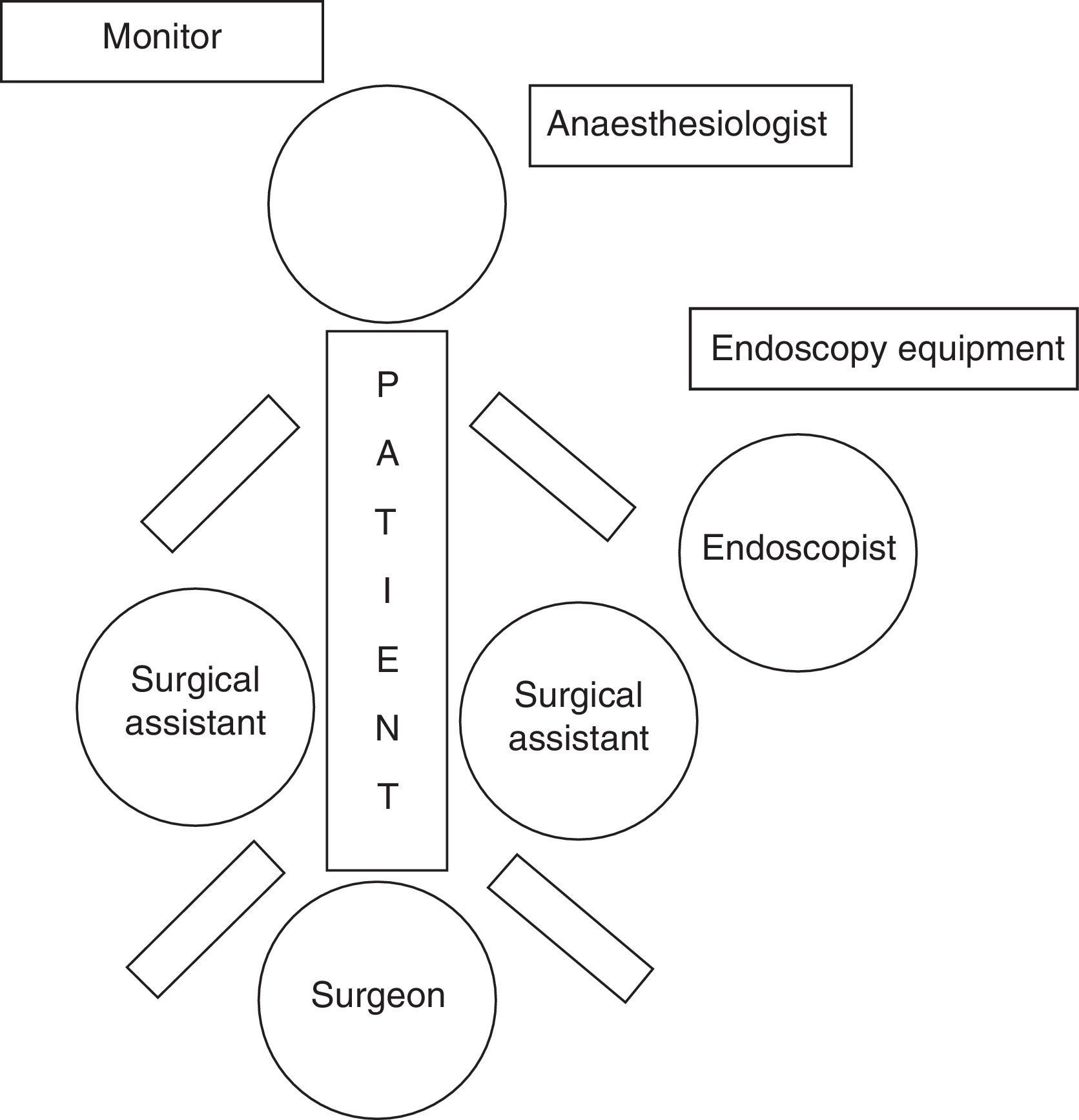
We present the case of a 34-year-old male with a history of laparoscopic gastric bypass for morbid obesity one year earlier. Presently, he came to the emergency department due to epigastric abdominal pain that had been progressing over several days and was associated with marked mucocutaneous jaundice, choluria, acholia and nausea without vomiting. Work up showed total bilirubin 8.4 and GPT 893. Abdominal ultrasound demonstrated no dilatation of the intra or extrahepatic bile duct; the gallbladder was distended, with no wall thickening, and contained several microlithiases. During hospitalisation, magnetic resonance cholangiopancreatography detected minimal dilatation of the intra and extrahepatic bile duct, as well as a non-dilated common bile duct measuring 7.5mm. A “crab leg” image was seen in the distal common bile duct, which was compatible with multiple choledocholithiases with cholelithiases. The patient was considered for laparoscopy-assisted transgastric endoscopic retrograde cholangiopancreatography in association with cholecystectomy in the same operation (Fig. 1).
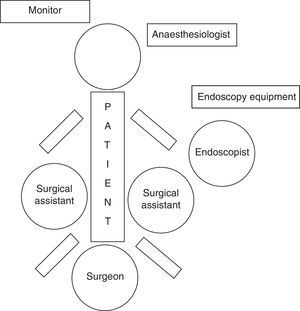
Our technique differs from others published in the literature by using a long balloon trocar that is usually utilised for morbid obesity surgery. In order to perform this surgery, the patient was positioned in supine decubitus with open legs or French position (Fig. 2). In this manner, endoscopy was done with sphincterotomy and the lithiasis and biliary sludge were removed by the balloon catheter. It is important to adjust the diameter of the endoscope with that of the trocar in order to avoid leakage of the air insufflated by the endoscopist. The procedure should be followed through the surgeon's optics. The gastrotomy was closed with intracorporeal suture and finalised with a standard laparoscopic cholecystectomy.5 The operative time was 165min.
The patient presented a postoperative period without incident and was discharged after 24h. One month after surgery, the patient was completely asymptomatic.
The main advantages provided by the use of the trocar-balloon in this type of cases are, first of all, that it is not necessary to release the gastric remnant, which in many patients presents numerous adhesions that can increase surgical time and morbidity. Second of all, it provides a leak-proof work area for the endoscopist, who requires continuous insufflation of air for the correct completion of the sphincterotomy, while providing very good manoeuvrability with the endoscope as the stomach is not attached to the abdominal wall like in other procedures described in the literature. As for the disadvantages of this approach, and according to the series examined, these include greater mobilisation of the surgical and endoscopic team, longer execution time and higher cost.6
Combined endoscopic-surgical approaches provide a valid, safe, feasible and reproducible strategy for the resolution of choledocholithiasis in select patients who have previously undergone a malabsorptive procedure for morbid obesity.7,8 It enables surgeons to resolve the pathology by means of a combined laparoscopic approach, without the need to initially propose open surgery or a more complex laparoscopic approach of the bile duct, resulting in less morbidity and shorter hospitalisation.9,10
In this technique, the interaction between the surgeon and endoscopist is essential for the procedure to be done correctly.
Conflict of InterestsThere are no conflicts of interests.
Please cite this article as: Melero Abellán A, Gumbau Puchol V, Mir Labrador J. Colangiopancreatografía retrógrada endoscópica transgástrica con asistencia laparoscópica para el tratamiento de la cole-coledocolitiasis en paciente intervenido de bypass gástrico. Cir Esp. 2016;94:111–113.