Mesenchymal tumours of the oesophagus are rare; gastrointestinal stromal tumours (GIST) and leiomyomas are the most frequent.1
Schwannomas of the digestive tract are mainly located in the stomach and bowel. Their oesophageal location is extremely rare, and few cases have been reported.2,3 We present a case of oesophageal schwannoma with an atypical form of presentation that has not been previously described.
A 31-year-old woman consulted her primary care doctor for having dysphonia for 2 weeks. Her condition was considered functional dysphonia, at which time she was referred to an ENT specialist. Seven days later, she came to the emergency room with headache, confusion and sudden dyspnoea. Blood work, LDH and tumour markers (CEA, CA 19.9, AFP, β-hCG and β2-microglobulin) were normal. On examination, the Boterman sign was detected, along with distension of the right jugular vein, facial oedema and cyanosis when the arms were raised.
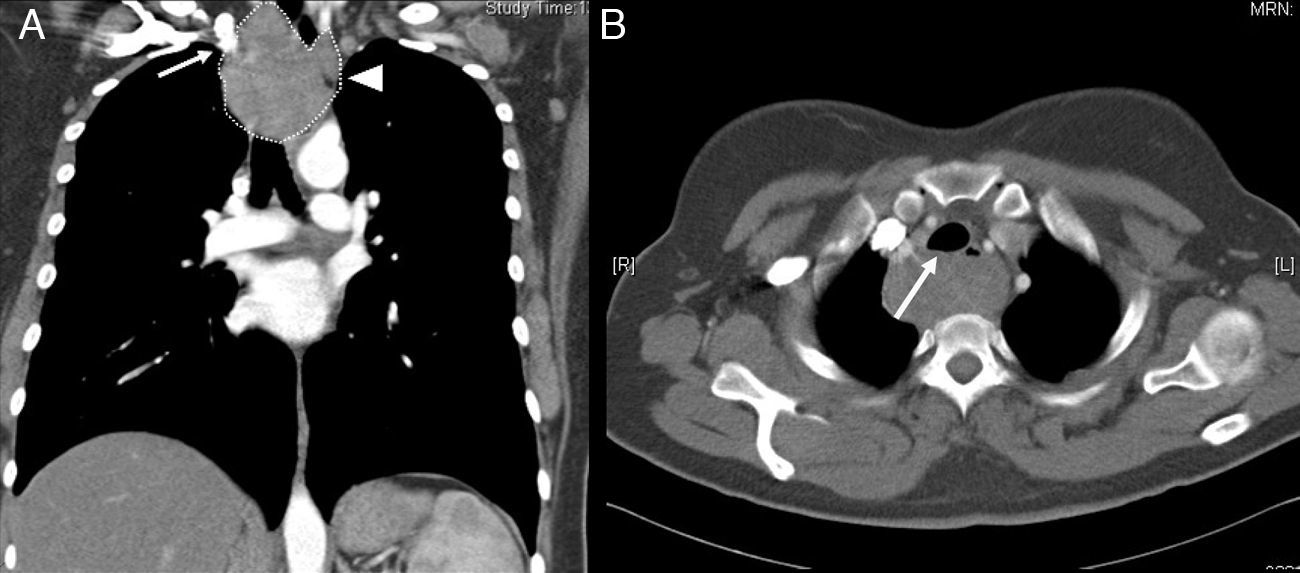
Chest radiography showed evidence of a mass in the mid and superior mediastinum that was approximately 7cm. Computed tomography (CT) revealed a well-defined mass measuring 4.1cm×6.4cm×7.6cm at the anteroposterior, transversal and craniocaudal axes, respectively, without calcifications and limited vascularisation. The lesion was situated posterior to the right thyroid lobe, oesophagus and trachea, which was displaced forward. No lymphadenopathies or metastases were observed (Fig. 1). Laryngoscopy showed the right vocal cord in paramedian position, and video-assisted bronchoscopy detected a reduction in the tracheal lumen of 50% due to extrinsic compression. Bronchial aspiration, brushing and transbronchial needle aspiration were negative for malignancy. Endoscopy showed no mucosal lesions or morphological alterations suggestive of neoplastic infiltration.
Given these findings, urgent surgery was indicated. Video-assisted thoracoscopy was first used because of the diagnosis and uncertain origin of the mass, and to exclude the possibility of intrathoracic metastases that may not have been seen on CT. Once the oesophageal origin of the mass was confirmed, oesophagectomy was performed in 3 phases with gastric pull-up using manual cervical oesophagogastric anastomosis.
The specimen measured 7cm×8cm×4.5cm, was dependant on the oesophagus, and presented no areas of mucosal ulceration. Upon slicing, the consistency was firm, the colour whitish and appearance fibrillar; all of these factors implied a mesenchymal origin.
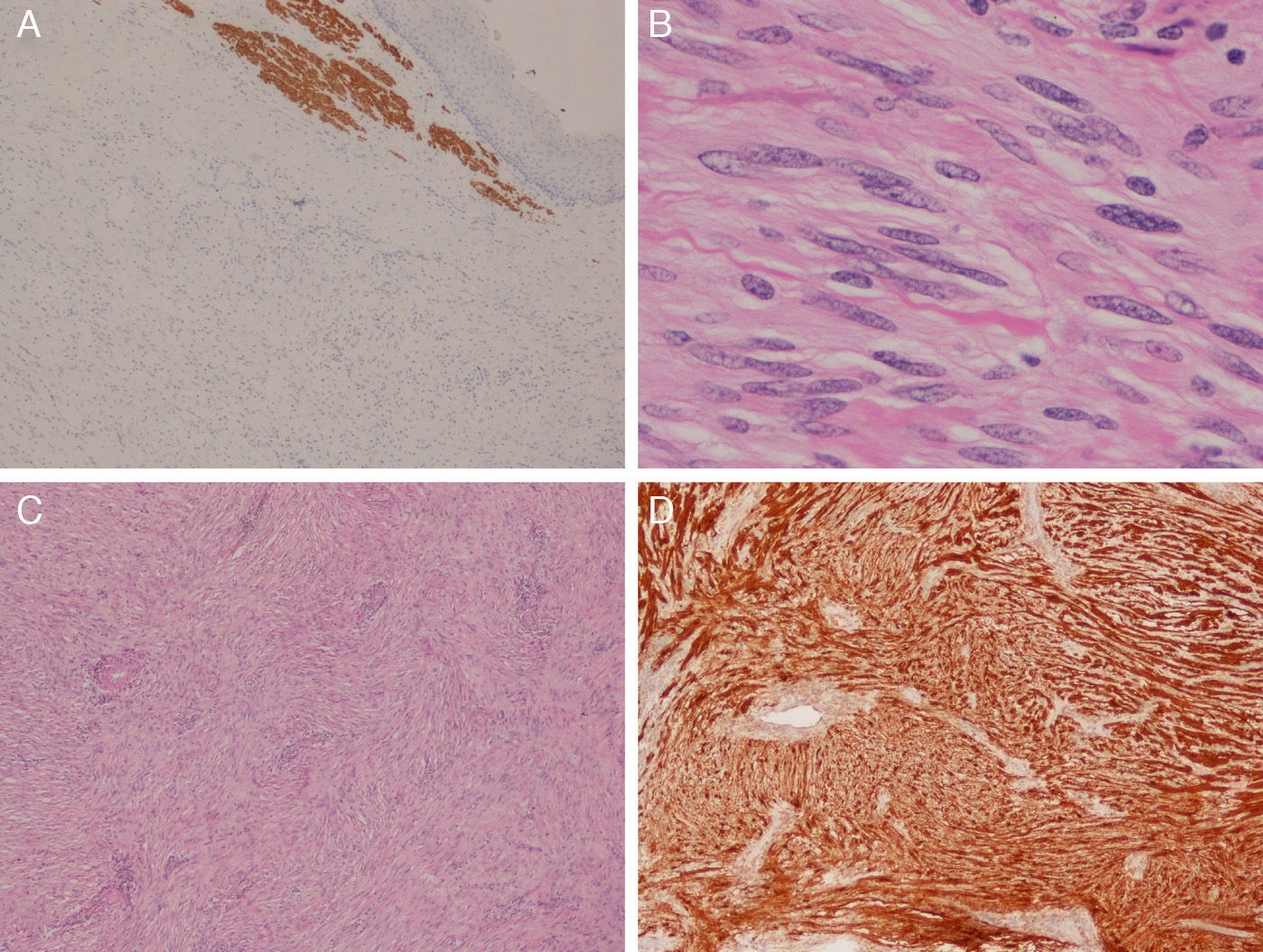
The microscopic study observed an absence of necrosis, lack of nuclear atypia and a mitotic rate lower than 5 per field, all of which are benign histological characteristics of peripheral nerve sheath tumours.2 Immunohistochemistry studies were positive for anti-s100 protein antibody and non-reactive for the antibodies anti-CD117, CD34, smooth muscle actin and desmin. Given said findings, the diagnosis of oesophageal schwannoma was reached (Fig. 2). The patient's condition progressed satisfactorily and she was discharged from the hospital on the 10th day post-op. Six months later, there have been no signs of recurrence, dyspnoea or altered phonation. The examination of the vocal cords by laryngoscopy was normal, which confirmed that the compression of the recurrent laryngeal nerve by the mass was the cause of the initial dysphonia. The symptoms of mental confusion and headaches attributed to the compression of the superior cava improved significantly after hospital discharge.
Microscopic images of the tumour: (A) positivity for desmin in the oesophageal muscle (above) and negativity in the tumour (below) (desmin, ×40); (B) high-magnification image showing nuclear morphology and absence of cytological atypia (HE, ×400); (C) low-magnification image showing the general appearance of the lesion (HE, ×100); (D) intense and diffuse staining for S100 protein (×100).
Chaterlin and Fissore4 described a benign oesophageal schwannoma for the first time in 1967. Even though cases have been reported with patterns of malignancy, most of these were benign and in Asian women in the fifth decade of life.3 More frequently, they are located in the upper oesophagus. Nonetheless, we have not found a correlation between this location and the possible link with the different muscle and nerve fibres of the cervical and thoracic regions. The most frequent initial symptom is dysphagia, followed by dyspnoea. Less frequent are palpitations, chest pain, cough and stridor.3,5 Our patient had a peculiar presentation of dysphonia, sudden dyspnoea and symptoms of confusion that required urgent surgery.
Preoperative diagnosis is difficult due to the radiological, clinical and endoscopic similarities with other mesenchymal tumours. As the lesion is submucosal, ultrasound results can be normal, as in our case, and the definitive diagnosis is made after surgical resection. In addition, the macroscopic appearance can be identical to that of GIST or leiomyomas. In the description of a series of benign schwannomas of the gastrointestinal tract, Daimaru et al.6 indicated how difficult it was to distinguish them from other oesophageal mesenchymal tumours.
In our case, positivity for the S100 protein and the lack of reactivity for CD117 and CD34 ruled out GIST. The negativity for actin and desmin helped distinguish it from a leiomyoma.7
The cervical approach (described by other authors as a less invasive alternative) was also discussed, but the limited surgical field, uncertain behaviour and possibility of firm adhesions to the superior vena cava led us to dismiss this option and opt for oesophagectomy with lymphadenectomy. Furthermore, there are reports of large tumours occupying large areas adjacent to the muscle layer that produce extensive defects in the mucosa, causing oesophagectomy to be necessary. Finally, the enucleation of submucosal tumours by means of thoracoscopy could be considered in tumours smaller than 2cm.5,8,9
We conclude that the diagnosis of oesophageal schwannoma should be considered in cases of mediastinal masses of the upper oesophagus associated with respiratory symptoms, dysphagia or alterations in phonation due to the frequency of the appearance of these symptoms.
Please cite this article as: Favre-Rizzo J, Lopez-Tomassetti Fernandez E, Sánchez-Ramos M, Hernandez-Hernandez JR. Schwannoma esofágico asociado a síndrome de vena cava superior. Cir Esp. 2016;94:108–110.