Afferent loop obstruction is a rare and potentially serious complication after pancreaticoduodenectomy. Pannala et al.1 report a frequency of afferent loop obstruction after pancreaticoduodenectomy of 13%, although other authors report 2.5%.2 The mean time transpired between the procedure and this complication is 1.2 years, and the most frequent cause is radiation enteropathy (37.5%), followed by tumour recurrence (33%) and adhesions (17%).1
We present the case of a 54-year-old woman who was treated surgically for adenocarcinoma of the head of the pancreas, including a pancreaticoduodenectomy (Whipple technique) with Child's transmesocolic loop reconstruction. The histopathology study showed evidence of a ductal adenocarcinoma with lymph node involvement (pT3N1). The patient received adjuvant chemotherapy with gemcitabine and capecitabine. Fourteen months later and due to an increase in Ca 19.9–259U/L, a PET-CT study was conducted, which detected local recurrence anterior to the pole of the right kidney measuring 15mm and a maximum SUV of 5.1; treatment was therefore initiated with gemcitabine for 6 months. The follow-up PET-CT demonstrated the same lesion that was still the same size, but the maximum SUV was now 2.6. The patient was treated surgically and a tumour implant was located in the Morrison pouch, anterior to the right kidney and adjacent to the afferent loop (Fig. 1A), which was resected. The histology report identified the mass as pancreatic adenocarcinoma.
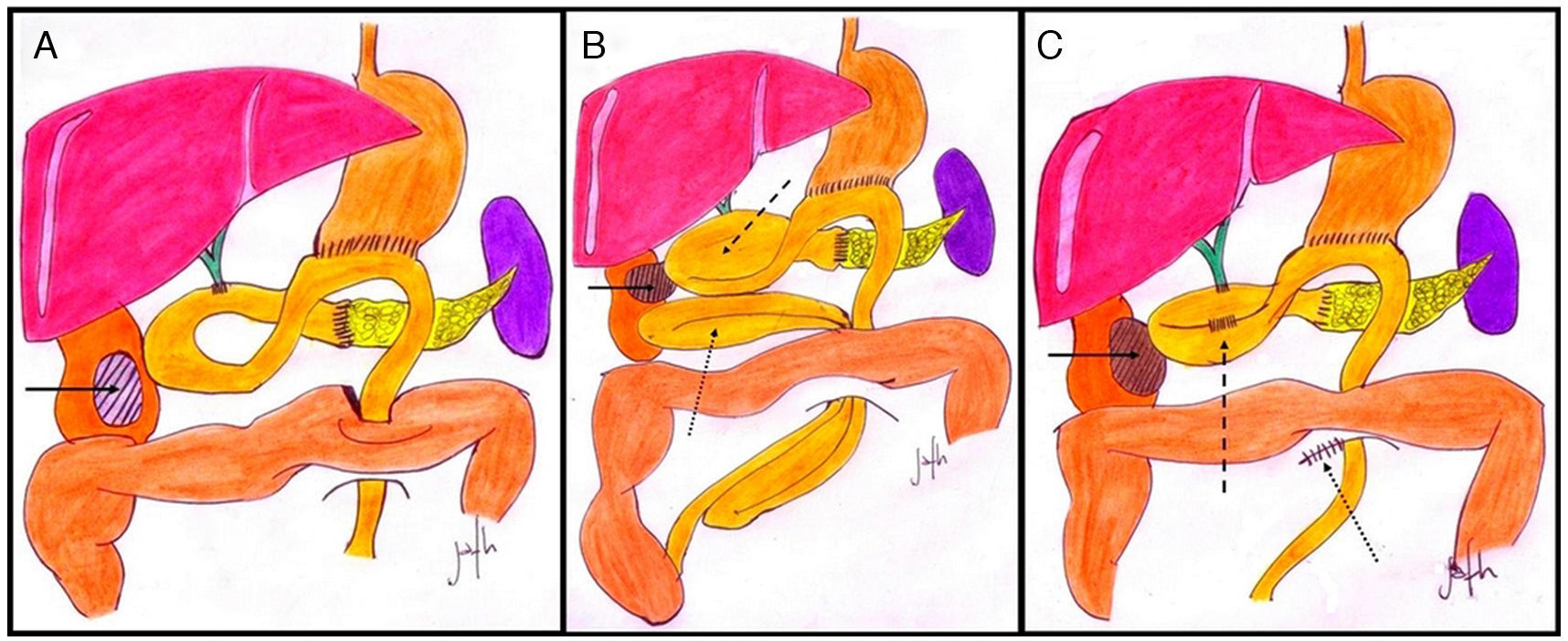
(A) Tumour implant anterior to the right kidney (solid arrow); (B) fibrosis at the pole of the right kidney (solid arrow), causing obstruction of the afferent loop (dashed arrow) and internal hernia of jejunal loops through the transmesocolic orifice (dotted arrow); (C) fibrosis at the pole of the right kidney (solid arrow), side-to-side jejunojejunal anastomosis of the afferent loop (dashed arrow), and reduction of jejunal loops with closure of the transmesocolic “buttonhole” (dotted arrow).
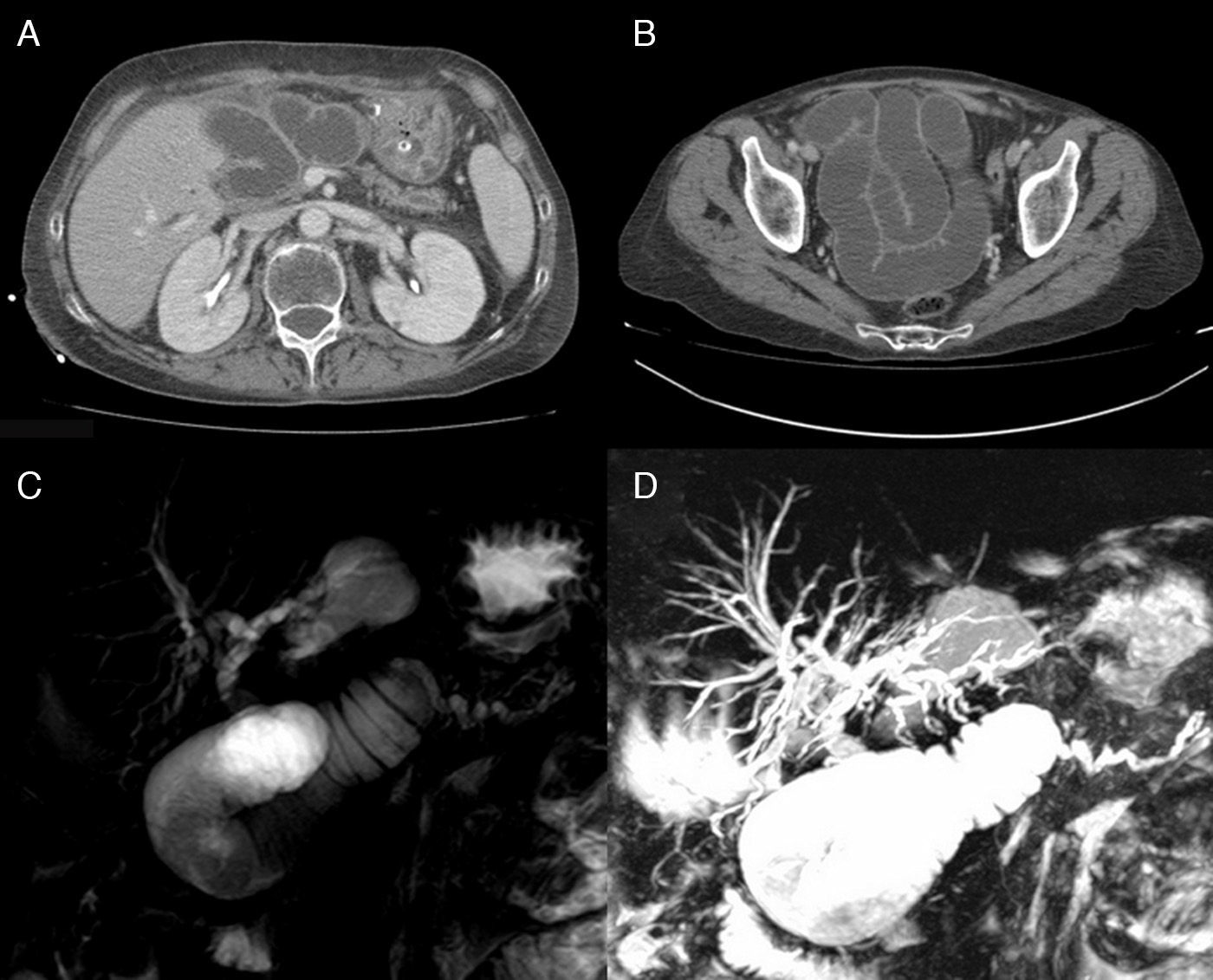
The patient came to the emergency room one month later due to fever, jaundice and abdominal pain. On physical examination, she presented jaundice of the skin and mucous membranes, abdominal distension, diffuse abdominal pain and pain upon percussion in the right lumbar fossa. Lab work-up showed: total bilirubin 6.36mg/dL, PCR 19mg/dL and 8710 leukocytes (neutrophils 83.5%). Abdominal ultrasound revealed dilatation of the intrahepatic bile duct and grade III right hydronephrosis due to stenosis of the ureteropelvic junction. CT scan (Fig. 2A and B), showed evidence of dilatation of the afferent loop and small bowel loops. Magnetic resonance cholangiopancreatography (MRCP) (Fig. 2C and D) reported a dilated bile duct, especially the left intrahepatic radicals, which presented beaded morphology and good passage through the hepaticojejunostomy. An upper gastrointestinal ultrasound through the afferent loop was not able to visualize the hepaticojejunostomy or pancreaticojejunostomy due to obstruction.
(A) Cross-sectional CT scan showing dilatation of the afferent loop and Wirsung duct; (B) cross-sectional CT image showing dilatation of jejunal loops in the pelvis; (C and D) reconstruction of MRCP showing obstruction of the afferent loop with dilatation of the Wirsung duct and extra- and intrahepatic bile duct.
With the diagnosis of right pyelonephritis, percutaneous nephrostomy was performed, and, given the diagnosis of cholangitis secondary to obstruction of the afferent loop, the patient was treated surgically. A retractile scar was found at the surgical site that was causing stenosis of the ureteropelvic junction of the right kidney and a bend with obstruction of the afferent loop, as well as an internal hernia in which the small bowel adopted a supramesocolic position through the mesocolic “buttonhole” (Fig. 1B). We proceeded with manual side-to-side jejunojejunostomy in the afferent loop (distended segment with collapsed segment), reduction of the herniated small bowel loop and closure of the mesocolic buttonhole (Fig. 1C). The postoperative period transpired without incident, the cholangitis was resolved, and the patient was discharged on the 8th day post-op.
There are several treatment options for the obstruction of the afferent loop after pancreaticoduodenectomy. These depend on the general state of the patient, type of reconstruction (Child's loop or Roux-en-Y) and the location of the obstruction regarding the pancreaticojejunostomy and hepaticojejunostomy.
If the general state of the patient is poor with a short life expectancy, due to tumour progression as well as associated comorbidity, less invasive treatments are preferred, such as the placement of a stent by means of endoscopy or interventionist radiology. If the patient's general state is good with a long life expectancy, the first therapeutic option is surgery.
The endoscopic or radiological therapeutic options are varied. In the case of Child's loop reconstruction, due to the proximity between the gastrojejunostomy and obstruction, a stent could be inserted by endoscopy.3 If this is not possible, the afferent loop is drained with the transhepatic placement of a stent4 or with direct needle aspiration of the obstructed loop.5 However, due to the risk for bile leakage and peritonitis at the puncture site, it may be necessary to attach the afferent loop to the anterior abdominal wall. In cases of Roux-en-Y reconstruction, as the endoscopic approach is impossible, transhepatic placement of a stent is possible if the obstruction is close to the hepaticojejunostomy; percutaneous needle aspiration should be reserved for when the obstruction is close to the base of the loop.6
Different descriptions of surgical techniques include: side-to-side jejunojejunostomy of the dilated afferent loop with a jejunal loop4 or with the lesser curvature of the stomach,7 proximal resection of the afferent loop and Roux-en-Y reconstruction8 or bypass of the afferent loop in Roux-en-Y.9 In the obstruction of the afferent loop in Roux-en-Y, there are descriptions of pancreaticojejuno-jejunostomy, which is a technique that avoids revision of the pancreaticojejunal anastomosis.10 In our case, a side-to-side anastomosis was done between the distended and collapsed segments of the afferent loop (Fig. 1C), which is a different surgical alternative that could be effective in the treatment of cholangitis and would avoid intestinal resection.
Conflict of InterestsThe authors declare that there are no funding or other aspects that could lead to a conflict of interests.
Please cite this article as: Ruiz Pardo J, Llàcer-Millán E, Jimeno Griñó P, Fernández Hernández JÁ, Parrilla Paricio P. Colangitis por obstrucción de asa aferente tras duodenopancreatectomía cefálica. Cir Esp. 2016;94:106–108.