Postoperative lung lobe torsion is a rare condition, with an incidence between 0.09 and 0.3%.1 It occurs more frequently after upper lobectomies (74.4%), and the middle lobe is most vulnerable to torsion (29.4%).2 Rotation of the lobe pedicle causes venous occlusion, resulting in thrombosis and hemorrhagic infarction. Therefore, early diagnosis is of vital importance.3 We present the case of a patient with left upper lobe torsion after left lower lobectomy requiring urgent thoracotomy and lobectomy.
The patient is a 72-year-old woman with high blood pressure and no toxic habits, diagnosed with breast cancer that had been treated with left mastectomy 25 years earlier. Preoperative computed tomography (CT) scan showed a lung mass measuring 5.5×3.8cm in the upper and posterolateral segments of the lower left lobe (LLL). Bronchoscopy revealed a tumor-like lesion at the entrance of the bronchus of the upper segment of the LLL. Transbronchial biopsy was compatible with primary lung adenocarcinoma. After a PET/CT extension study, the tumor was staged as cT2bN0M0.
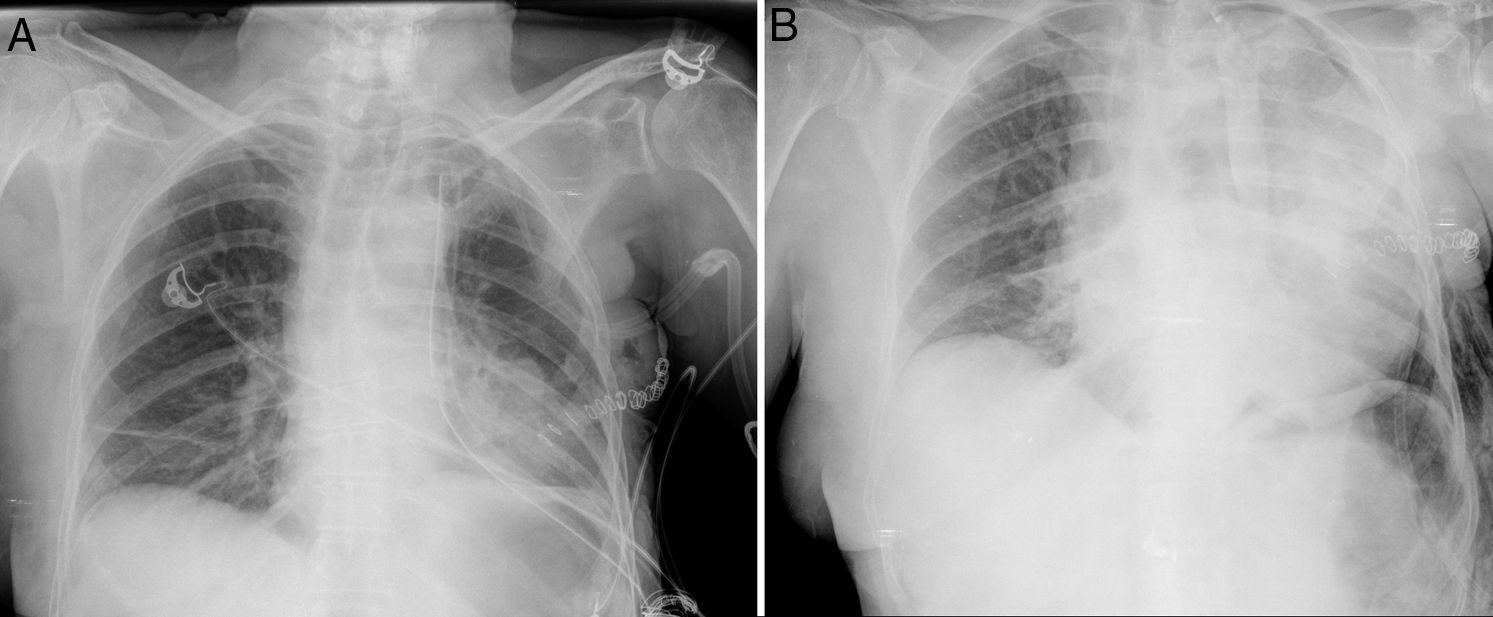
Left lower lobectomy was performed, and systematic lymphadenectomy was done by video-assisted thoracic surgery (VATS) using 2 ports. The immediate postoperative period was satisfactory. A simple chest X-ray 24h later showed no notable findings (Fig. 1A). On the second day post-op, the patient developed general malaise and hemoptysis. There were no clinical or laboratory data showing respiratory failure or infectious process. Serosanguineous pleural fluid was drained at a rate of 500ml/24h for the first 2 postoperative days. Progressive anemia was detected during this timeframe, requiring the transfusion of 2 units of packed red blood cells. Simple chest radiograph 48h after the intervention demonstrated a condensation in the left upper lobe (LUL) and re-expansion defect (Fig. 1B).
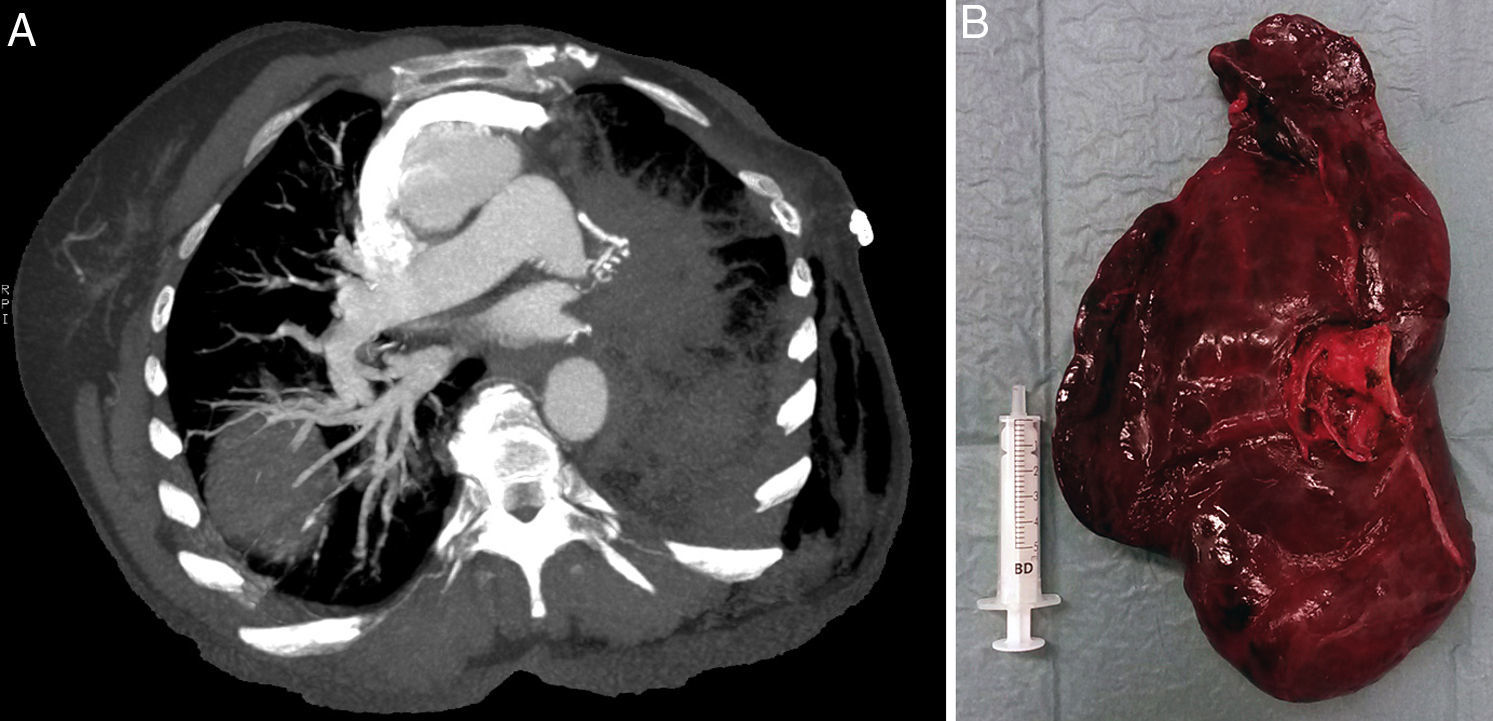
Given the suspicion of lobe torsion, a CT scan was ordered, which showed extensive diffuse left lung involvement comprised of areas of consolidation, ground glass and septal thickening related with pulmonary hemorrhage or edema. This was accompanied by absence of filling of the venous/arterial tree of the left lung, suggestive of devascularization. Sharp tapering was also observed with complete occlusion of the left pulmonary artery and ipsilateral superior pulmonary vein, proximal to the left bronchus, with delayed enhancement of the pulmonary vasculature in inverted position, which suggested probable LUL torsion (Fig. 2A).
With this clinical-radiological diagnosis, axillary thoracotomy was performed, which confirmed a 180° counterclockwise lobe torsion (lingula toward the vertex and apex turned back and downwards). The lobe was twisted, hepatized and nonviable, so pneumonectomy was completed and bronchoplasty of the bronchial stump was performed with pericardial fat (Fig. 2B). In the immediate postoperative period, the patient presented an episode of paroxysmal atrial fibrillation with good response after pharmacological reversion. He was discharged on the ninth postoperative day after re-operation.
Lobe torsion is an uncommon condition that occurs in 70% of cases after right upper lobectomy.3 In a study of 7889 patients who underwent elective lung resection, only 2 cases of left upper lobe torsion were diagnosed.4
In lobe torsion, the most frequent rotation is 180° clockwise. Rotation of more than 180° or angulation of the pedicle causes acute obstruction of the bronchus, pulmonary artery and vein, inducing atelectasis, infarction, and pulmonary necrosis.4,5
Previously described predisposing factors3,4,6 include the presence of complete interlobe fissure, narrow lobe hilum, absence of adhesions with other structures, atelectasis or insufficient pulmonary re-expansion, presence of pneumothorax or pleural effusion, and dissection of the inferior pulmonary ligament. In the case presented, we believe that laxity of the pedicle and a small lung lobe were causes that led to torsion.
Clinical findings vary from asymptomatic patients in early stages, to progressive and fatal decline with sudden dyspnea, acute respiratory failure, hemoptysis and chest pain.3,4,7 Simple chest X-ray within the first few post-operative days identifies signs like lobe opacification or air trapping.3 CT studies provide accurate diagnosis of left upper lobe torsion at the start of this condition. Bronchoscopy shows extrinsic stenosis or bronchial obstruction.3,4
In general, the treatment of choice for lobe torsion is lobectomy by thoracotomy.1 In cases of torsions of less than 180° with incomplete obstruction of the pedicle, detorsion and lobe preservation are controversial.5 There have been reports of cerebrovascular accident following detorsion of the affected pulmonary lobe. Therefore, some authors recommend lobe resection to prevent possible embolism.6,8
Early diagnosis of pulmonary torsion is of vital importance. It is necessary to have a high index of suspicion, and to evaluate the usefulness of systematic chest X-rays within the first few days post-op.
Please cite this article as: Moreno Asencio MT, Rivo Vázquez E, Quiroga Martínez J, Moldes Rodriguez M, García Prim JM. Torsión lobar superior izquierda tras una lobectomía inferior videoasistida. Cir Esp. 2017;95:406–408.