Neurological diseases are not uncommon, exhibiting a lifetime prevalence of 6% in the general population being even higher among elderly. The trend of the most common neurological disorders (cerebrovascular disease, Parkinson, dementia, epilepsy) for presentation at older ages, the increasing need of elderly for surgery (of any type) and the demographic aging of the population result in higher rates of neurological cases among patients undergoing surgery, especially the elderly.1–3
Perioperative management of neurological patients is a clinical challenge, demanding the active participation of several medical experts for better handling of the multiple specific and complex medical issues accompanying surgery in patients with known neurological disease. The appropriate adjustment of the neurological treatment (before, during and after surgery), the selection of the optimal anesthetic technique and regimens, the need for additional or specific preoperative tests, consultations or interventions, are only some of those issues.2–4 Moreover, the frequent presence of various comorbidities and the multisystem and multiorgan involvement characterizing particular neurological disorders such as Parkinson and neuromuscular diseases, necessitate a multidisciplinary approach in their handling.5–8
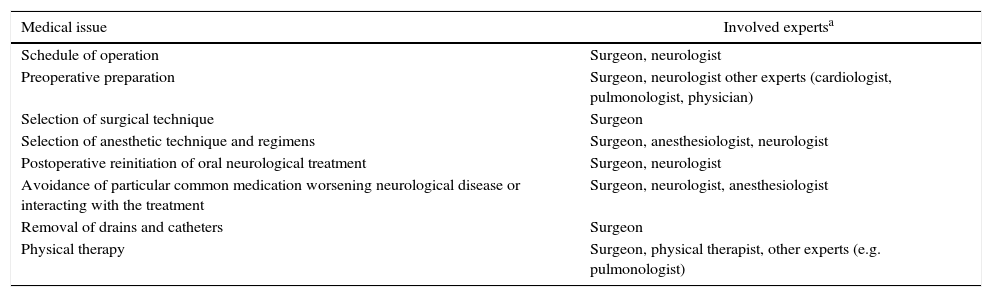
Literature publications on the issue have mostly focused on the role of anesthesiologist and neurologist in the perioperative management of neurological patients, frequently overlooking the role of surgeon.1–3,6,7,9 However, surgeon has a central and crucial position in this process, not limited to the performance of the operation and the handling of particular surgical complications (e.g. bleeding, wound infections). The main medical issues requiring surgeon's participation are listed in Table 1 and analyzed in the following paragraphs.
Surgeon's Participation in the Multidisciplinary Perioperative Management of Neurological Patients.
| Medical issue | Involved expertsa |
|---|---|
| Schedule of operation | Surgeon, neurologist |
| Preoperative preparation | Surgeon, neurologist other experts (cardiologist, pulmonologist, physician) |
| Selection of surgical technique | Surgeon |
| Selection of anesthetic technique and regimens | Surgeon, anesthesiologist, neurologist |
| Postoperative reinitiation of oral neurological treatment | Surgeon, neurologist |
| Avoidance of particular common medication worsening neurological disease or interacting with the treatment | Surgeon, neurologist, anesthesiologist |
| Removal of drains and catheters | Surgeon |
| Physical therapy | Surgeon, physical therapist, other experts (e.g. pulmonologist) |
Preoperatively, for elected surgery, surgeon determines the optimal time of operation in cooperation with the neurologist and the other experts involved in the preoperative assessment of the patient, providing the necessary time interval for stabilization and improvement (if feasible) of the neurological disorder, or the completion of neurological assessment and investigation (for recently diagnosed cases). Other medical issues attributable either to the surgical problem or to existing comorbidities should be revealed and appropriately regulated before surgery: Anemia, malnutrition, fluid and electrolyte or metabolic abnormalities, hypertension, presence of active or subclinical infections (respiratory, urinary, etc.) not only increase the general perioperative risk and the rate of complications, but may also worsen, rekindle or even predispose to particular neurological conditions (neuromuscular disease, epilepsy, stroke). Also, prophylactic antibiotics (if required) should be compatible with the administered neurological medications.1–3,6,7
The critical decision for continuation or withdrawal of the antiplatelet or anticoagulant agents in stroke patients undergoing surgery should be based on a multidisciplinary patient evaluation (surgical, neurological, cardiological), considering both the risk of bleeding and that of perioperative stroke. The former is limited for minor procedures (dental, ophthalmologic, colonoscopies), whereas the latter is associated with advanced age, cardiac and cerebrovascular disease and cardiac and major vascular surgery. Therefore, decision should be individualized.2–4,9
Another important issue is the selection of minimally invading surgical techniques (laparoscopic, robotic, thoracoscopic, etc.) which is clearly a surgeon's decision – based on the existing indication for the particular case. The subsequent reduction of surgical stress, inflammatory reaction, pain, blood loss and transfusion need and other risk factors related to the extent of the operation may prevent the exacerbation of neurological disorders, such as multiple sclerosis and myasthenia Gravis, which is potentially triggered by the aforementioned factors.1,2,6,7 It may also minimize the risk of perioperative cognitive dysfunction which is strongly associated with the extent of surgery, patient age and preexisting mental disturbances (i.e. dementia).1–3,10 A combination of separate less invading techniques is preferable in some cases, e.g. choledocholithiasis, treated with endoscopic sphincterotomy followed (at second time) by laparoscopic cholecystectomy.
Moreover, surgeon interferes in the selection of the method of anesthesia (general, local, regional), in cooperation with the anesthesiologist and the neurologist. Apparently, the existence of respiratory and cardiovascular disorders (due to the neurological disease or to comorbidities) renders preferable regional or local anesthesia (especially for minor surgery). However, certain local anesthetics or upper extremity blockade could worsen myasthenia Gravis, whereas the presence of neurological motor symptoms (tremor and dyskinesia) in Parkinson may hamper the execution of surgery.3,7,8
Postoperatively, the surgeon determines the appropriate time of reinitiation of oral intake of neurological medications (depending on the type of surgery), which is an essential component of patient management. In addition, the decision for removal of drains and folley catheters (facilitating patient mobilization and recovery) belongs to the surgeon. However, handling of these issues could be hampered by the presence of dysphagia, paralytic ileus and urinary retention–not uncommon complications in particular neurological disorders (Parkinson, multiple sclerosis). Surgeon, should also order physical therapy (for respiratory and/or motor problems) to prevent complications and assist recovery.2,3,6–8
Close cooperation between surgeon, anesthesiologist and neurologist is required regarding the administration of common analgesics (i.e. opioids), antiemetic agents (e.g. metoclopramide), benzodiazepines and barbiturates potentially presenting serious interactions with the neurological medications (e.g. the interaction between meperidine and monoaminoxidase inhibitors in Parkinson) or worsening neurological symptoms. Therefore, all these common agents should be avoided or cautiously used.2,3,7,8,10
In conclusion, surgeon has a key role in the perioperative management of neurological patients, actively and essentially participating in the most critical treatment decisions and coordinating the other experts involved in this process.
Please cite this article as: Papagiorgis P. El papel del cirujano en el manejo perioperatorio de enfermedades neurológicas. Cir Esp. 2017;95:408–410.