Primary leiomyosarcoma (LMS) of vascular origin is a rare tumor (1/100 000 malignant tumors) most frequently located in the inferior vena cava (60%).1–4 Primary LMS of the gonadal vein is a very rare entity, and only a dozen cases have been reported in the literature.2,5,6
A 72-year-old woman consulted for pain in the right flank, accompanied by early satiety and weight loss. Physical examination revealed a palpable mass in the right hemiabdomen that was painful to pressure.
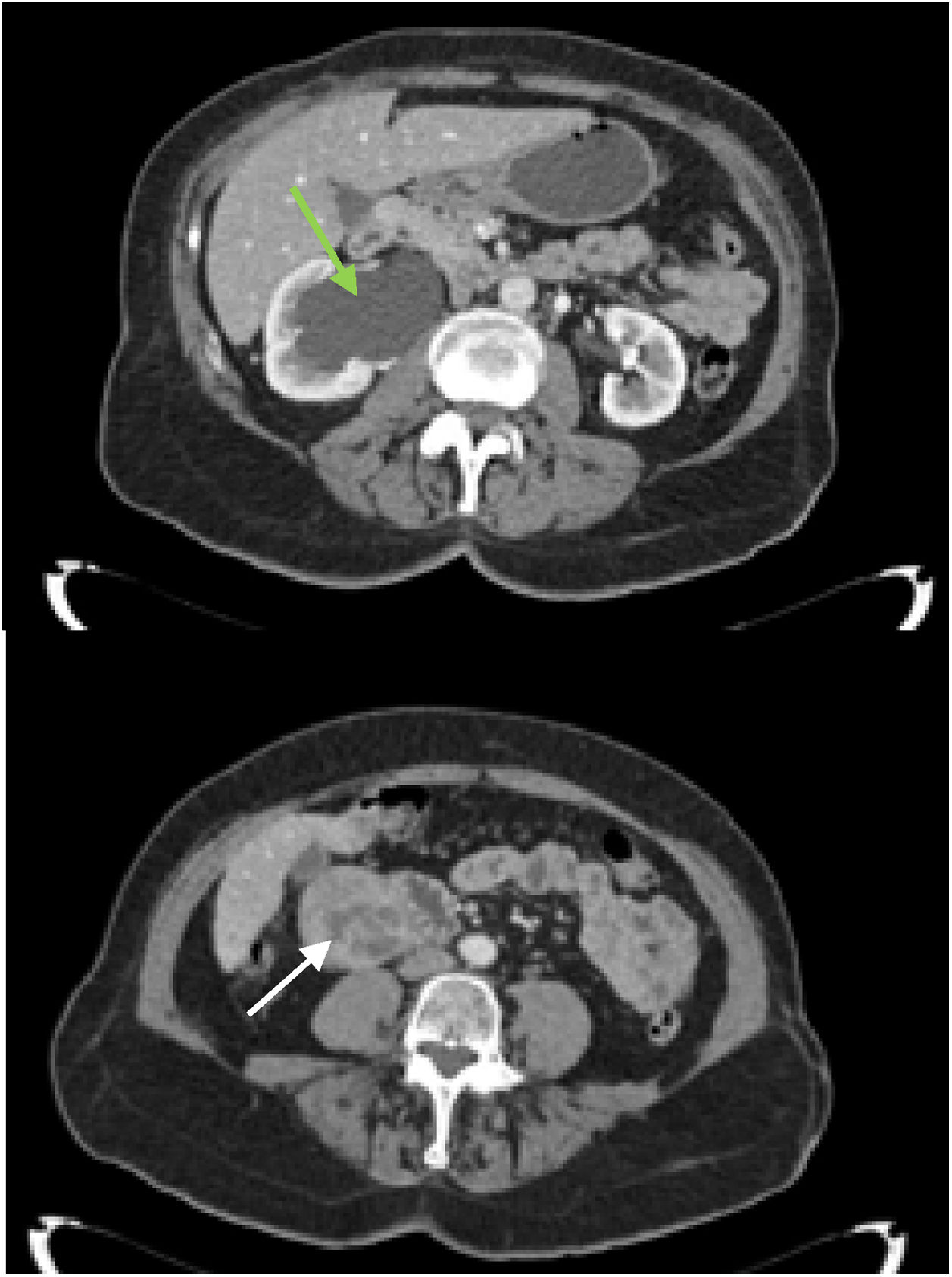
Abdominal ultrasound detected a heterogeneous retroperitoneal mass measuring 6 × 5 cm and the presence of calcifications adjacent to the right renal pelvis, causing ipsilateral hydronephrosis. On computed tomography (CT) scan, this mass appeared to be in contact with the 2nd part of the duodenum and the inferior vena cava, with no clear signs of invasion (Fig. 1). In addition, grade III right hydronephrosis was observed due to compression versus invasion of the middle ureter, along with calcifications and foci of intratumoral necrosis that could have been related to a GIST. Endoscopic ultrasound ruled out duodenal wall dependence/invasion. The results of ultrasound-guided CNB identified a malignant mesenchymal neoplasm with smooth muscle differentiation, indicative of LMS, although without being able to rule out WT-GIST. No secondary pulmonary deposits were found on extension chest CT.
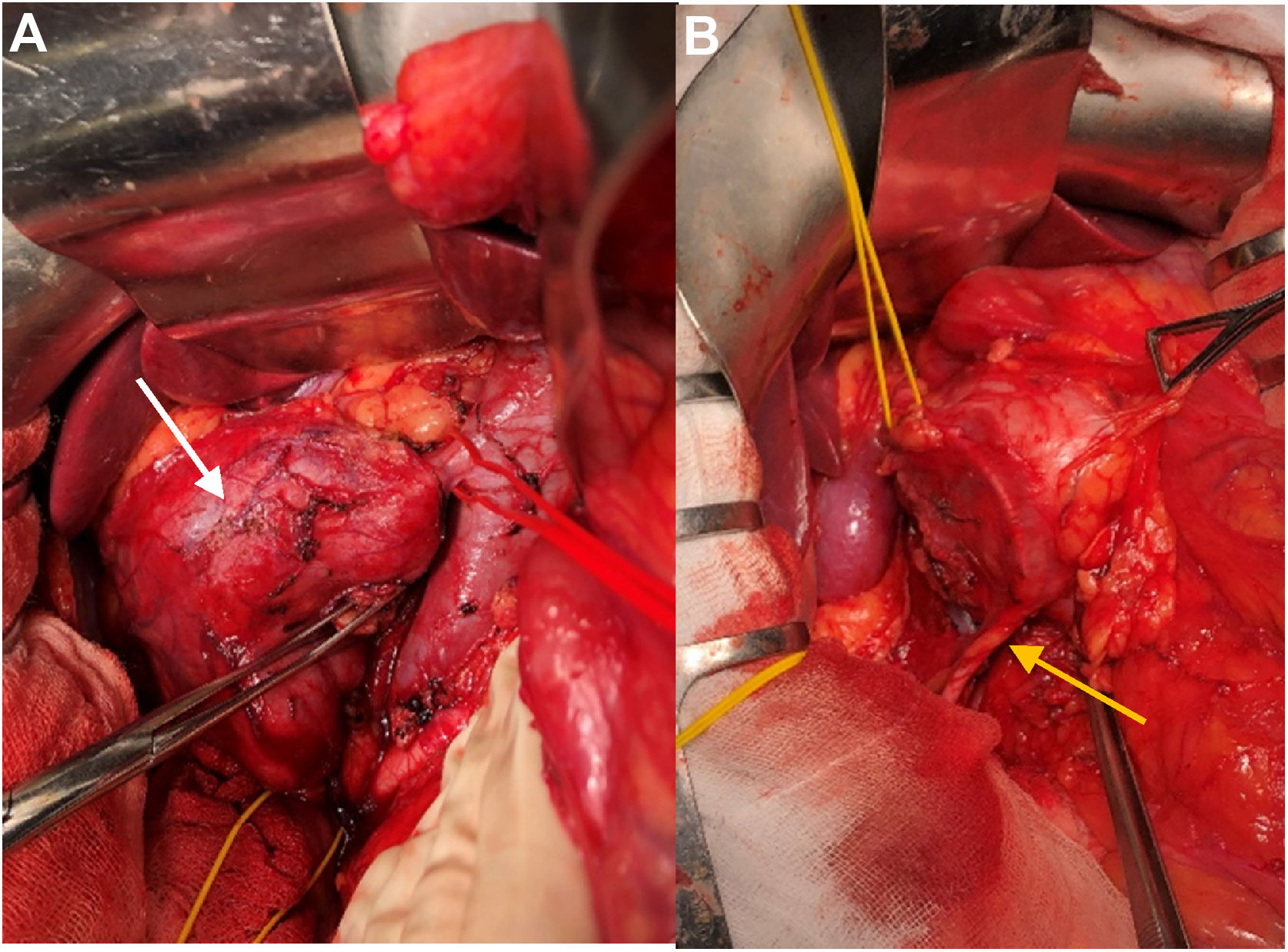
With a diagnosis of retroperitoneal mesenchymal tumor, and with the uncertainty of being able to guarantee en bloc resection with negative margins via laparoscopy due to possible invasion of surrounding structures, an open approach was chosen. Using midline laparotomy, we found a mass measuring 10 cm in diameter adjacent to the lower pole of the right kidney and the inferior vena cava, dependent on the right gonadal vein. The right ureter was in close contact but ultimately showed no evidence of invasion. Tumor excision involved ligation and resection of the right gonadal vein, after vascular control in the supra and infrarenal cava and liberation of the right ureter, previously stented with a JJ catheter (Fig. 2).
The patient had no postoperative incidents and was discharged 72 h after surgery. The definitive pathological examination reported grade III LMS with free resection margins, 10% tumor necrosis and a mitotic index of 35 mitoses/10 cmga (pT2NxMx). The patient received no adjuvant treatment. After 12 months of follow-up, there have been no signs of local or distant tumor recurrence.
LMS are neoplasms originating from the smooth muscle fibers of the tunica media of the vessels. They are more frequent in women (2:1) between the ages of 60 and 69.4 Generally, they present an extravascular (60%) and slow growth pattern. LMS are usually asymptomatic until they reach large sizes, and the most common symptoms in the cases reported are the appearance of abdominal pain or a palpable mass.6
The absence of initial symptoms together with their low incidence and, therefore, low diagnostic suspicion generally mean that LMS are diagnosed late, leading to a worse prognosis.
Tumor size, depth of invasion, histological grade, and vascular origin have been described as prognostic factors.1,6
LMS of vascular origin has been associated with a worse prognosis than those of other locations, given to their high potential for hematogenous dissemination.1,5
Published series report some 12% of LMS in a location other than the vena cava with metastases at diagnosis (most frequently pulmonary); however, none of the cases is an LMS with a gonadal location.3,4
To date, there is no clear evidence on the role of chemo or radiation therapy in terms of survival or lower local recurrence rates, so the cornerstone of treatment continues to be surgery.
Complete tumor resection with free margins, including en bloc resections of neighboring structures in case of invasion, is essential. R0 resection is the main objective as it is the most important prognostic factor6–8 and associates the highest survival rates (5-year survival: 33%–68%).9,10 For this reason, given the uncertain invasion of the right middle ureter in the case of our patient, we decided (together with the Urology Service) to opt for an open approach in order to guarantee complete tumor removal (R0).
The laparoscopic approach in this type of tumor must be evaluated with caution. De la Fuente et al9 describe the case of an LMS of the right gonadal vein where, in the absence of a preoperative histological diagnosis, they decided to carry out a minimally invasive approach. The definitive histopathological analysis of the surgical specimen revealed a high-grade LMS with resection margin involvement (R1), with the prognostic implications that this entails, as previously described.
Given the limited number of cases described in the literature of LMS of the gonadal vein, it is important to report each case. This provides visibility in order to progress in the knowledge of this disease, thereby increasing the diagnostic suspicion for earlier diagnosis and early treatment, with the probable positive impact in prognostic terms.
Please cite this article as: Puerta Vicente A, Sanjuanbenito A, Lobo E. Leiomiosarcoma de vena gonadal derecha. Cir Esp. 2021;99:764–766.