Any surgery in morbidly obese patients is associated with a higher incidence of complications, such as deep vein thrombosis, pulmonary thromboembolism, pneumonia, fat necrosis, and wound dehiscence1. For these reasons, these patients undergo post-bariatric panniculus resection after their body mass index (BMI) normalizes. But when the abdominal apron is so large that it limits daily activity, abdominal panniculectomy is proposed. Although the patients are explained how this procedure entails a high incidence of complications and even death, most patients choose to assume the risk. The operation must be carefully planned, and a device must be prepared in the operating room to raise the abdominal apron and suspend it in order to dissect the fat without it continuously obstructing the surgical field.
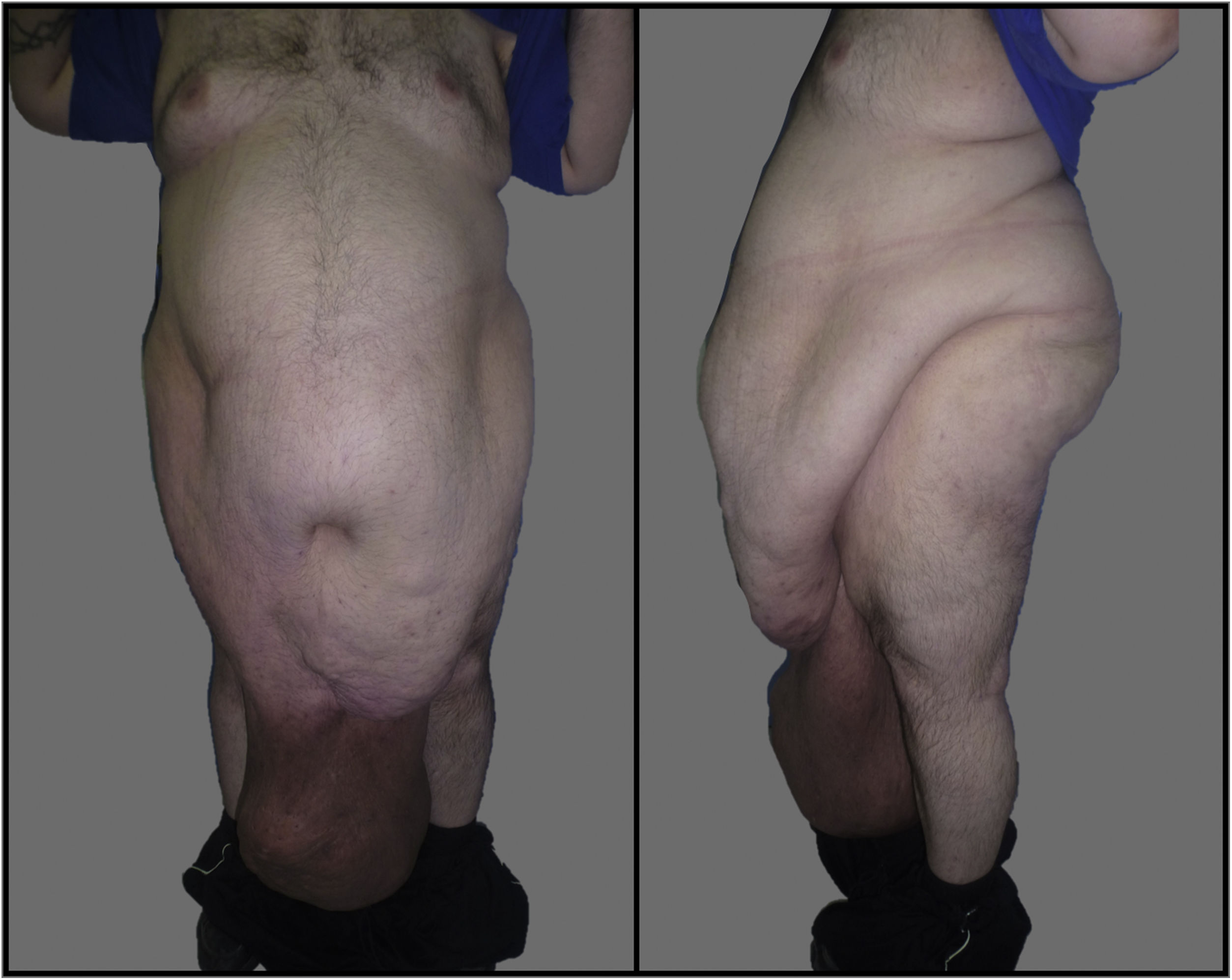
We present the case of a morbidly obese 40-year-old male with a massive abdominal panniculus (BMI: 61.73 kg/m2) that reached his ankles (Fig. 1).
In July 2017, he came to the Emergency Department for a fever of 38 °C, associated with foul-smelling suppuration from a wound secondary to distal necrosis of the abdominal apron. Lab work showed: 46.04 thousand/mm3 leukocytes, 86.2% neutrophilia, coagulopathy and lactic acid 4.9 mmoL/L. Because it was technically impossible to perform an urgent standard computed tomography (CT) scan due to grade IV morbid obesity, the imaging test was performed in the inverted position (feet first) in order to visualize the content of the apron. He presented extensive cellulitis and an abscess measuring 25 × 13 cm in the most distal part; the presence of an inguinoscrotal hernia was ruled out. The patient underwent emergency surgery under general anesthesia to drain the abscess. Due to the state of septic shock caused by cellulitis of the apron, 48 h later we performed urgent abdominal dermolipectomy. To facilitate the surgical technique, a crane was used to suspend the panniculus by means of a 4-suture Ventrofil® (BRAUN) system, with 2 sutures through the skin at each end of the apron that were attached to both arms of the crane (Fig. 2).
The surgical specimen weighed 24 kg, and the patient required admission to the Resuscitation Unit for a week. After being discharges to the ward, he presented good evolution with targeted antibiotic therapy for Actinomyces turicensis, Phorfyomonas somarae and Pseudomona aeruginosa, which had been identified in cultures. PREVENA™ KCI negative pressure therapy was placed over the surgical wound for 10 days to promote healing. Drain tubes were removed on the 7th and 11th days after surgery, and the patient was discharged one month after admission.
In November 2018, the patient returned to the Emergency Department for incarcerated umbilical hernia with no signs of intestinal obstruction, requiring urgent umbilical hernia repair. The patient had gained weight and once again presented a massive panniculus. On the 7th seventh postoperative day, he started a low-grade fever associated with cellulitis in the most distal region of the abdominal apron. Imaging tests ruled out associated abscess and, after the failure of conservative treatment using broad-spectrum antibiotic therapy, we decided to perform another dermolipectomy, with the same suspension technique described; this time, the surgical specimen weighed 20.6 kg.
Several methods have been described to retract the abdominal apron during scheduled surgery. Ollapallil et al.2 describe a technique with 2 Kuntcher nails that pierce the adipose pad and suspend it from a crane with chains. Gabilondo et al.3 use a ‘stirrup-nail’ system suspended from pulleys previously installed from the ceiling of the operating room. Graf et al.4 use a specific retractor: the Rultract Skyhook Surgical Retractor System (Rultract Inc, Cleveland, Ohio). Meanwhile, Fadel et al.5 use forceps that are connected to the abdomen with a bar that is lifted by a crane.
In our case, the panniculectomy was carried out urgently, and we had to use the resources available at that time, specifically the crane for obese patients and the Ventrofil® sutures through the skin on both sides of the panniculus, which were fastened to the crane arms to lift and move it. We believe that the suspension method we describe can be used in any hospital. It is effective because it holds the weight well, without tearing the skin, and provides good mobilization of the abdominal apron.
Please cite this article as: Pérez de la Fuente T, Blanco Terés L, Viamontes Ugalde F, Gimeno A. Recurso técnico inusual en una paniculectomía abdominal urgente en paciente superobeso. Cir Esp. 2021;99:763–764.