Major ambulatory surgery (MAS) has been shown to be cost-effective while maintaining quality of care and patient safety1. The complications associated with thyroid and parathyroid surgery, such as asphyctic haematoma, recurrent injury, and hypocalcaemia, are controversial2.
The importance should be highlighted of specialisation in endocrine surgery3 and outpatient surgery, where morbidity should be minimal. The main obstacle to undertaking ambulatory procedures is postoperative bleeding, which has an incidence of between .5% and 3%, and is more frequent in the first 6 h and exceptional after 24 h4.
The use of new technologies in coagulation and sealing of vascular pedicles has made it possible to reduce surgical time and increase safety levels with respect to postoperative bleeding5.
We present a retrospective observational study of patients scheduled for ambulatory hemithyroidectomy or parathyroidectomy between 2019 and 2020.
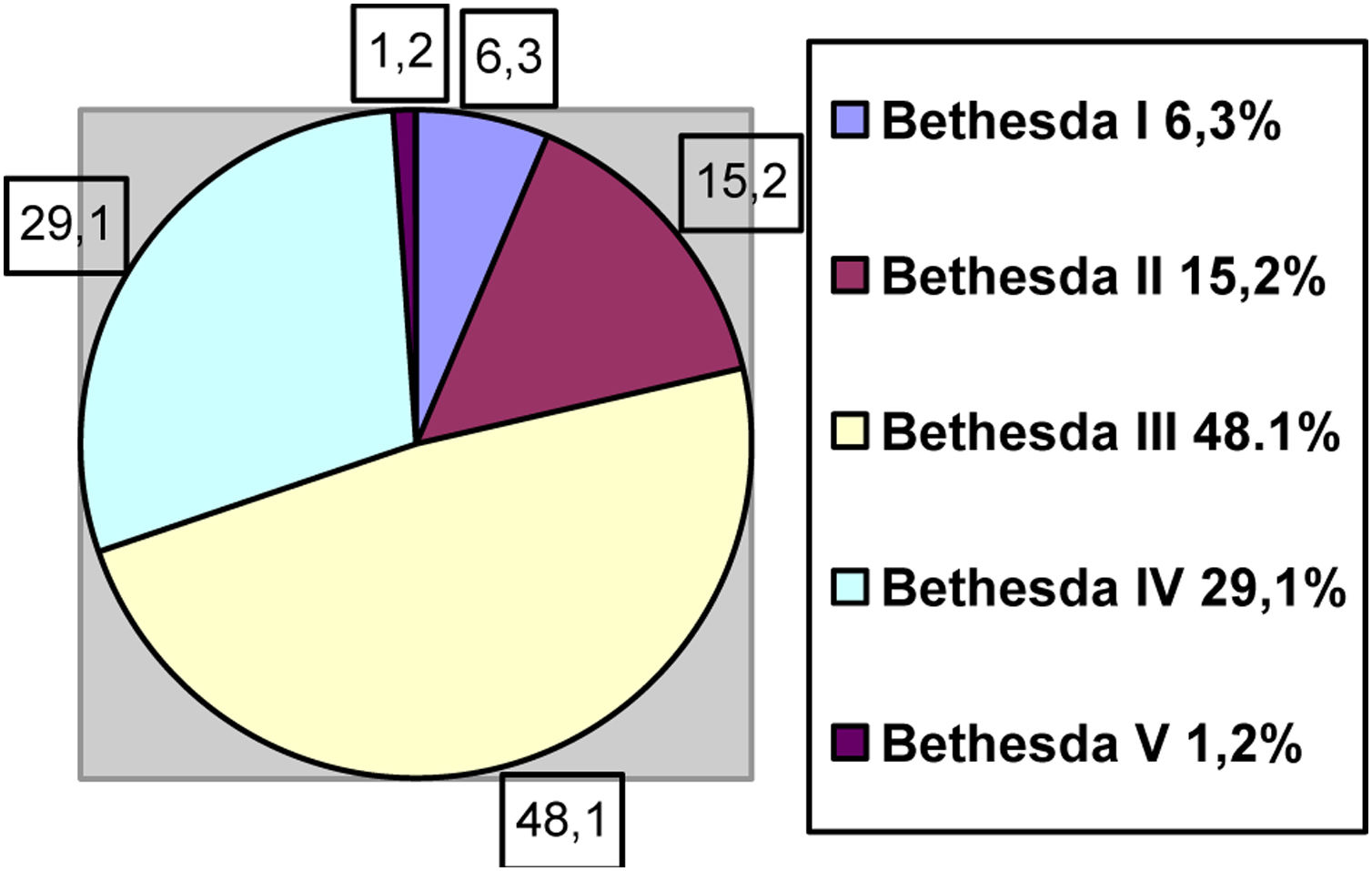
Patients scheduled for hemithyroidectomy, or parathyroidectomy (decision taken in a multidisciplinary committee) are scheduled from for ambulatory surgery from the clinic. The selection criteria are as follows: older patient, anaesthetic risk ASA I-III, adequate social or family support, regardless of Bethesda (Fig. 1) or nodule size (mean size recorded is 27.7 cm, with a range between 7 and 57 cm).
All patients are operated by surgeons dedicated exclusively to endocrine surgery, with the support of the MAS infrastructure.
The patients come to the hospital one hour before surgery, and are kept for 6 h for observation. They are then discharged home if they meet the following criteria: stable vital signs; no ecchymosis, bruising or cervical swelling; no dysphonia, dyspnoea or dysphagia, good oral tolerance, adequate pain control, ambulation, understanding of instructions, adequate home support, and possibility of telephone monitoring.
In parathyroidectomies, parathyroid hormone (PTH) is measured prior to surgery and 10 min after removal of the gland, requiring levels within the normal range for discharge.
In hemithyroidectomies, ultrasonic scalpel and motorisation of the recurrent laryngeal nerve (RLN) are used for vascular sealing.
At 24 h, the MAS nurse makes a phone call to monitor patients early and to assess level of satisfaction, using a questionnaire.
A follow-up visit is then made to the endocrinology clinic 4 weeks after the intervention. On the surgery side, assessment is “non-face-to-face” with a form designed to assess postoperative progress, possible complications related to the wound and nerve damage. Patients with symptoms suggestive of nerve damage are referred to ENT for evaluation.
Over the period described, 82 hemithyroidectomies and 13 parathyroidectomies were performed. Three patients scheduled for hemithyroidectomy and one for parathyroidectomy did not meet the criteria for MAS, and therefore were scheduled for inpatient surgery (they were not included in the study).
In the 79 ambulatory hemithyroidectomies, 77.2% were discharged 6 h after surgery (pure MAS), 21.5% required a hospital stay of less than 12 h (short-stay MAS). Only one patient (1.3%) required admission for cardiology assessment due to electrocardiogram abnormalities.
In the short-stay MAS patients, the reason for prolonged stay was because the surgery was performed in the afternoon in 64.7% (Table 1).
Reasons for a night of admission.
| Parathyroidectomy 12 patients | Reasons |
|---|---|
| Pure MAS (83.3%) | – |
| Short stay MAS (16.7%) | 1 operation during evening shift |
| 1 RLN injury |
| Hemithyroidectomy 79 patients | Reasons |
|---|---|
| Pure MAS (77.2%) | – |
| Short-stay MAS (21.5%) | 64.7% operations in evening shift |
| Other: vomiting, syncope, requested by patient |
MAS: major ambulatory surgery; RLN: recurrent laryngeal nerve.
With 6-h surveillance, there were no early complications. Of the 17 patients in short-stay MAS, 29.4% presented mild seroma (reported by the patient, which had already resolved on examination) and dysphonia in 17.6%, with fibrolaryngoscopy without paralysis on examination by ENT (Table 2). Of the 61 patients with pure MAS, 19.6% had mild seroma, one patient (1.6%) had a wound infection that required treatment at their health centre, 1.6% had upper laryngeal nerve symptoms, and 6.3% had RLN symptoms (no lesion detected by ENT).
Postoperative complications according to surgical technique and type of MAS.
| Hemithyroidectomy 79 patients | Complications |
|---|---|
| Pure MAS (73%) | 19.6% seroma |
| 1.6% wound infection | |
| 1.6% superior laryngeal nerve symptoms | |
| 6.3% RLN symptoms (without injury) | |
| Short stay MAS (26%) | 29.4% seroma |
| 17.6% dysphonia without VF injury |
| Parathyroidectomy 12 patients | Complications |
|---|---|
| 8.3% RLN injury noted (1 patient) |
VF: Vocal folds; MAS: Major ambulatory surgery; RLN: Recurrent laryngeal nerve.
Complications were not statistically significant (P > .05) in the pure MAS patients versus short-stay MAS patients.
In the 12 parathyroidectomies included in the study, the outpatient rate was 83.3% for pure MAS and 16.7% for short-stay MAS. The reasons for admission were because the surgery was performed in the afternoon in one case and RLN injury noted during the operation in another (Table 1).
No wound-related complications were reported (Table 2). There is also no record of readmissions or visits to the emergency department due to hypocalcaemia in the patients studied.
Therefore, based on the data obtained, the ambulatory rate for hemithyroidectomies and parathyroidectomies is close to 80% and the rate of unwanted admissions (understanding unwanted as short stay) is 16.7% for parathyroidectomy and 21.5% for hemithyroidectomy. No patient presented major complications at home and the level of satisfaction was high or very high according to the nursing surveys and the hospital's Net-Promotor-Score. The major limitation of the study is the small number of patients included.
Ambulatory surgery does not increase the number of complications related to wound, bleeding or nerve damage, and the results are comparable to those found in the literature6.
We can conclude that parathyroidectomy with selective approach and hemithyroidectomy performed by expert surgeons on an ambulatory basis meet the objectives of outpatient surgery: they reduce the cost of the process, are safe, effective, and well accepted by patients7. To achieve this, it is important to select patients correctly (which minimises potential risks8) and provide them with detailed information from the clinic.
Please cite this article as: de la Fuente Bartolomé M, Sánchez de Molina Rampérez ML, García Vasquez C, Vieiro Medina MV, Jiménez de los Galanes Marchan SF. Manejo de la cirugía tiroidea y paratiroidea en régimen ambulatorio. Cir Esp. 2022;100:600–602.