Urethroplasty is the surgical treatment of choice for urethral stenosis. Lichen sclerosus is one of the most common causes of anterior urethral stenosis and can entail extensive involvement, sometimes extending from the fossa navicularis to the verumontanum. This type of stenosis is called panurethral stenosis and its treatment poses a surgical challenge1. In these cases, urethroplasty with free grafting of oral mucosa according to the Kulkarni technique achieves good results and avoids multiple surgeries with cosmetic and functional compromise of the penis2,3. It is based on urethral enlargement through dorsolateral placement of the grafts, preserving contralateral urethral vascularisation.
Obtaining long grafts generally requires the use of mucosa from both cheeks as a donor site and even additional mucosal grafts from the tongue or lip, which significantly increases the morbidity associated with the procedure4. This is complicated in patients with previous graft harvesting due to failed urethroplasty, radiotherapy to the donor site, poor oral hygiene, or heavy smokers5. Pedicled skin grafts and flaps are also contraindicated in the treatment of lichen sclerosus due to its high recurrence1.
We present 2 patients with panurethral stenosis due to lichen sclerosus who were operated by a multidisciplinary team composed of urologists and general surgeons at the Hospital Universitario de Getafe, using urethroplasty with a single graft of rectal mucosa extracted by transanal surgery. Table 1 presents these patients’ main operative data.
Main preoperative, operative, and postoperative data of both patients.
| Case 1 | Case 2 | |
|---|---|---|
| Platform | TEO | TAMIS: GelPOINT® |
| Instruments | Forceps and harmonic scalpel | Bipolar |
| Mechanical bowel preparationa | Yes | Yes |
| Preoperative colonoscopy | Yes | Yes |
| Antibiotic prophylaxis | Yes | Yes |
| Operation time, hours | 6 | 5.5 |
| Hospital stay, days | 2 | 4 |
| ERAS protocol | Yes | Yes |
| Antibiotherapy at dischargeb | Yes | Yes |
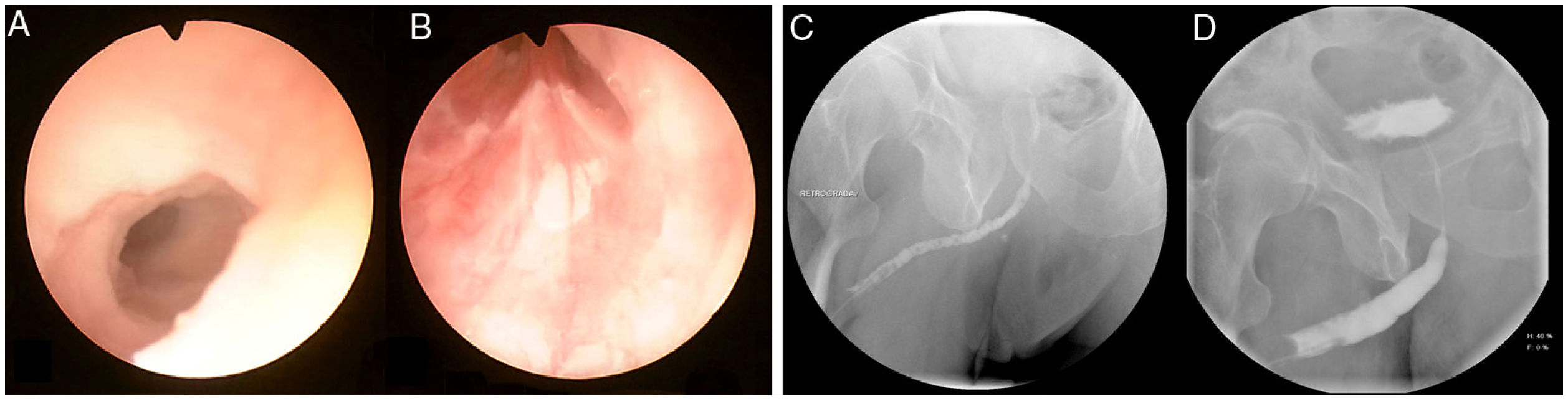
The first patient was a 72-year-old circumcised male with a history of diabetes, dyslipidaemia, arterial hypertension, bladder urothelial carcinoma undergoing transurethral resection on 4 occasions and dilatation of the anterior urethra on 6 occasions in the last year. Both combined urethrography and cystoscopy with integrated 14Ch cystoscope after urethral dilatation confirmed the diagnosis of panurethral stenosis of approximately 19 cm in length (Fig. 1A and B). The second was a 78-year-old male with a similar history of circumcision, dilatations, diabetes, dyslipidaemia, and hypertension. Combined urethrography confirmed panurethral stenosis of approximately 20 cm in length (Fig. 1C). Cystoscopy could not be performed.
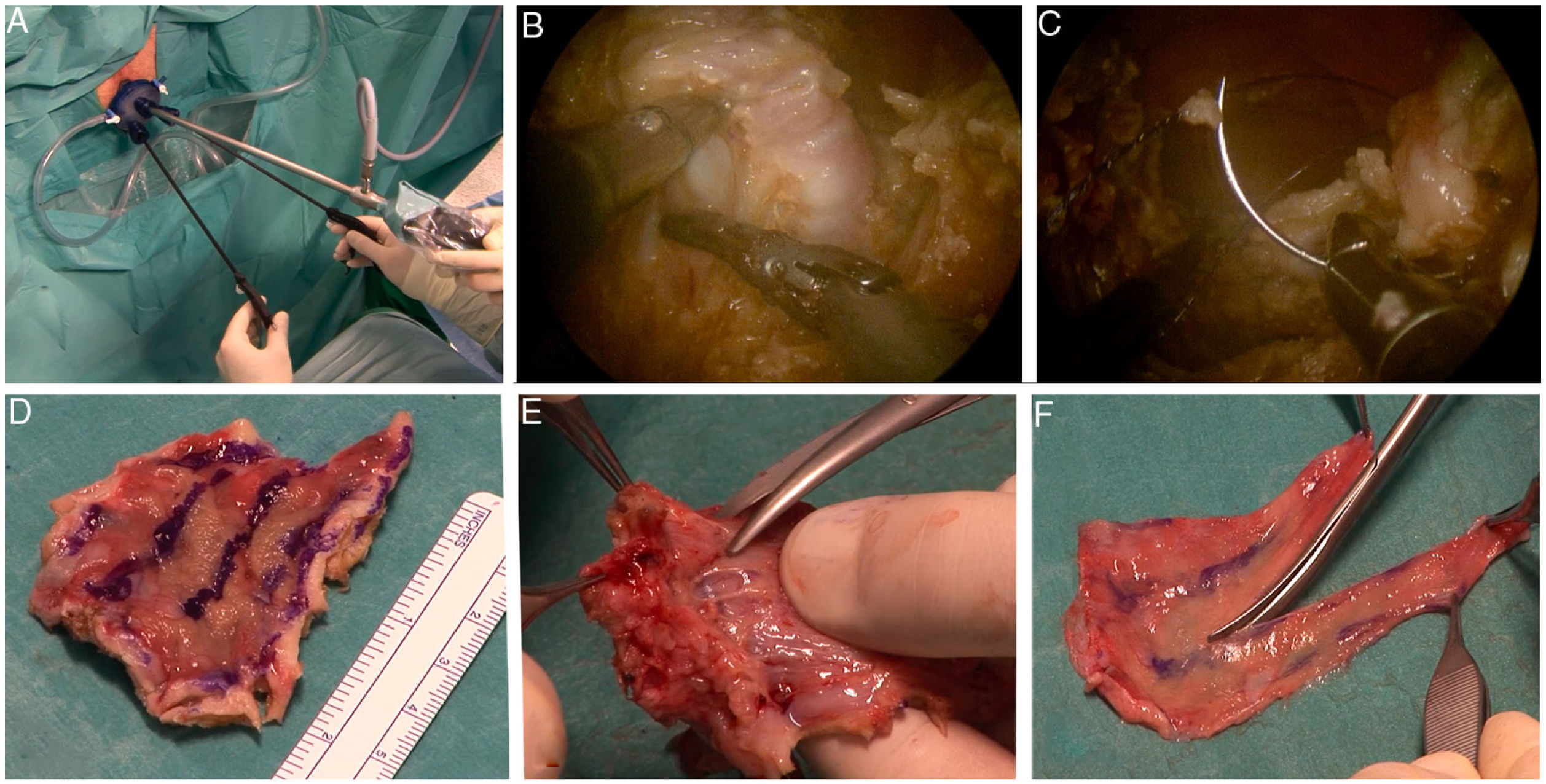
In both cases, underlying tumour or inflammatory bowel disease was ruled out by colonoscopy and abdominal CT before undertaking this surgical technique. In the second patient, a polyp was detected 20 cm from the anal margin corresponding to tubular adenoma, a disease that did not contraindicate removal of the rectal graft. In the first case we used a specific platform for endoscopic transanal surgery, and in the second case we performed minimally invasive transanal surgery with a GelPOINT® platform and conventional laparoscopic instruments (Fig. 2A–C).
Removal of rectal mucosal graft by transanal minimally invasive surgery (TAMIS) with GelPOINT® platform (A). Dissection down to the circular stratum of the tunica muscularis (B) and closure with V-Loc™ 3-0 longitudinal barbed suture (C). Rectal patch removed (D), separation of the rectal mucosa (E) and carving of the rectal mucosa in an “N” shape resulting in a free longitudinal graft of 22 × 1.5 cm (F).
A single free graft of rectal wall (rectal mucosa and muscle) in the form of a patch of approximately 6 × 5 cm was obtained in both patients. Dissection was carried out on the posterior rectal wall, avoiding opening the peritoneal cavity, with forceps and harmonic scalpel in the first case and bipolar in the second. The incision was started 2 cm from the dentate line, from distal to proximal. The dissection plane was the circular stratum of the tunica muscularis. Once the rectal patch was removed, the defect was closed with V-Loc™ 3-0 longitudinal barbed suture. We preferred to close the donor site and avoid second intention healing to promote early recovery and avoid possible stensoses6. There is no consensus on the closure of the rectal defect, although there tend to be fewer complications (bleeding and infection) closing the gap7,8. The mucosa was carved on the bench and trimmed in an “N” shape to convert it into a longitudinal graft of approximately 22 × 1.5 cm (Fig. 2D–F). These grafts allowed a single dorsolateral graft urethroplasty (supplementary material).
The 16 Ch urethral catheter was maintained for 3 weeks. Neither patient presented haematoma, pain or fistula, the most frequent complications of this surgery. There was also no rectal morbidity. One of the patients required readmission due to transient cognitive impairment, although a thromboembolic process associated with the procedure was ruled out. Retrograde urethrography at 3 months confirmed urethral patency and absence of postvoid residue and urethral diverticula (Fig. 1D). Both patients had an excellent clinical outcome 2 years after the procedure, with no recurrence of stenosis and good maximum flow rate (16.2 and 18.1 mL/s, respectively), and were very satisfied with the result, with no cosmetic impact or scarring, with normal erection without diversion and with preserved ejaculation.
In our experience, the rectal mucosa graft obtained by transanal surgery is an interesting resource that allows long segments of rectal mucosa to be obtained, making it possible to effectively reconstruct long anterior urethral stenoses. This technique avoids oral pain and limitations in speech and mastication, which are the sequelae of obtaining oral mucosa grafts9. We believe that it could be considered, even as a first choice, in patients with very long stenoses due to lichen sclerosus. Furthermore, this harvesting strategy is particularly indicated in patients with contraindications to oral cavity graft harvesting, such as multi-operated patients in whom oral mucosal grafts have been used previously.
A disadvantage of this technique is the increased surgical time that it entails, as it prevents 2 surgical teams from working simultaneously in 2 fields, as is usually done in oral extraction and simultaneous preparation of the perineal field for urethroplasty. In addition, this technique requires multidisciplinary teams with rectal surgeons experienced in transanal surgery and urologists experienced in urethroplasty techniques.
The use of minimally invasive transanal surgery to extract rectal mucosa to be used as graft material in urethroplasty is a new opportunity for this type of technique in rectal surgery. At present, and especially considering the novelty of this approach, there are no data for us to compare the morbidity of obtaining rectal or buccal mucosa grafts, or the effectiveness of either. On the other hand, the different techniques of urethroplasty with grafts also make this comparison difficult. Nevertheless, panurethral stenosis associated with lichen sclerosus seems an optimal scenario to study the feasibility and convenience of obtaining rectal mucosa by minimally invasive techniques and thus avoiding repeated oral graft beds.
The authors would like to thank José Domínguez for his iconographic work.
Please cite this article as: Ruiz-Graña S, Ramos JL, Arance I, Angulo JC. Cirugía transanal mínimamente invasiva para extracción de mucosa rectal en el tratamiento de la estenosis panuretral asociada a liquen escleroso mediante uretroplastia de Kulkarni. Cir Esp. 2022;100:597–600.