The Karydakis technique for the treatment of pilonidal sinus is a widely accepted procedure by the scientific community.1,2 It involves asymmetric resection to flatten the natal cleft and lateralize the surgical suture,3 creating a flap from the medial edge to cover the defect and close the wound, avoiding the intergluteal cleft.
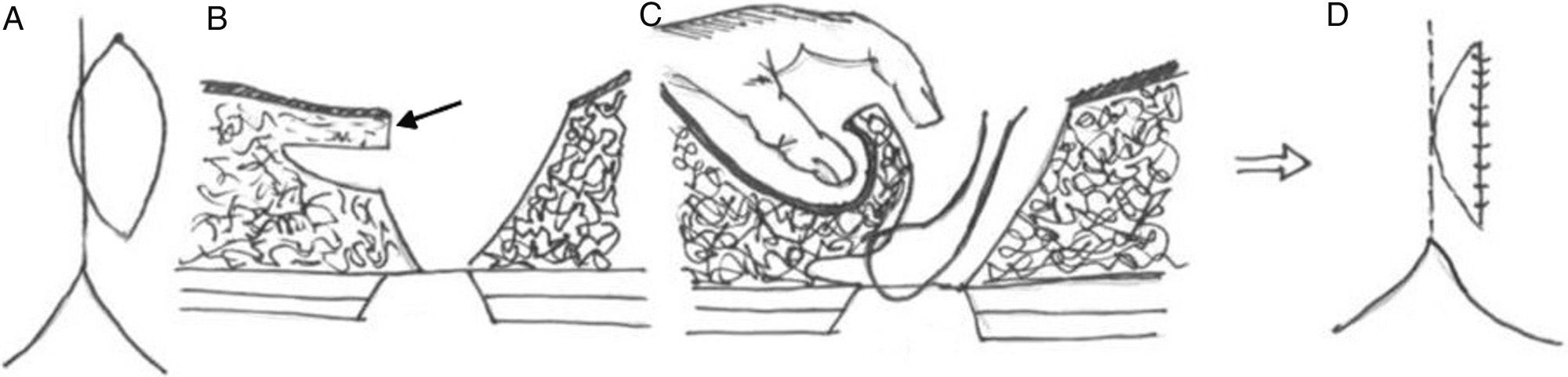
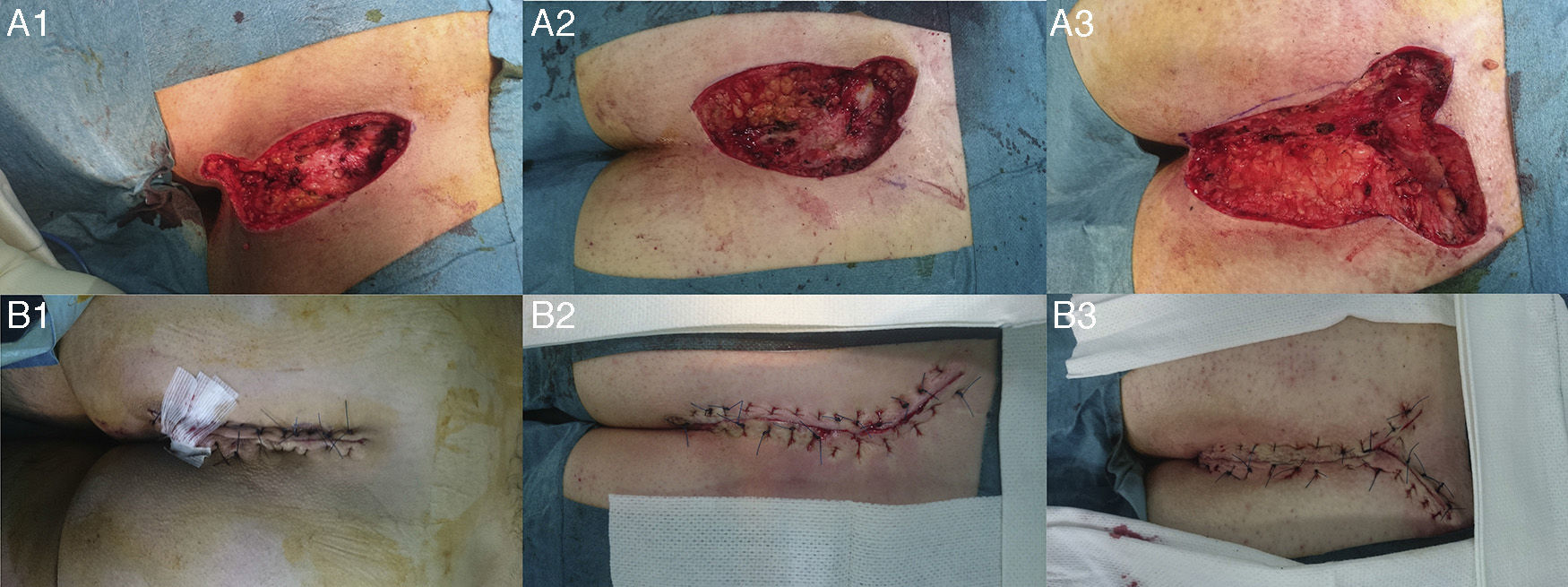
We present the cases of 3 patients with pilonidal sinus larger than 12cm, with lateral/bilateral projections of the pseudocyst (Table 1). In all cases, reconstruction was performed with the Karydakis technique (Figs. 1 and 2). In doing so, a paramedian line was drawn 2cm from the median line (becoming the new medial axis) displaced towards the side of the secondary orifice or where an induration was palpated, caused by the pilonidal sinus; the caudal end of the incision was displaced 1cm more to the side in order to distance the wound from the anus. The medial edge of the incision followed a curved path that crossed the midline, including the primary orifice(s), and the lateral edge was symmetrical with the medial edge to avoid the scar resting on the midline.3,4 All the affected tissue was resected until the sacrococcygeal fascia was reached. In the subcutaneous fatty tissue of the medial edge of the wound, 1cm underneath the skin, a flap was created from the fatty tissue some 2cm along the length of the wound. The lower lip of the flap was sutured to the rectosacral fascia on the midline with interrupted sutures, which caused lateral displacement of the flap. Another layer of interrupted sutures was used to deal with the raw surface, reducing dead space. However, our patients presented bilateral projections that required extending the excision. Therefore, in keeping with the principles of the Karydakis technique at all times, the fatty flaps were modified and fabricated along the medial edge, including the extensions of the excision.
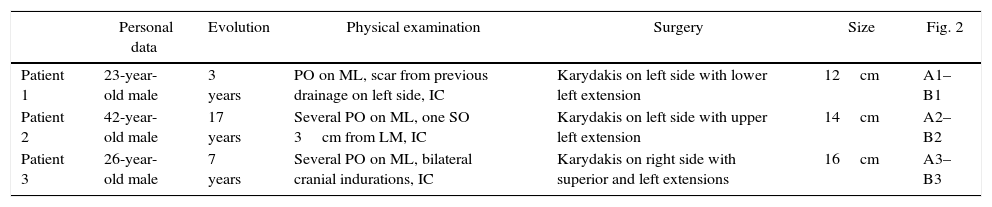
Clinical and Surgical Data of the Patients.
| Personal data | Evolution | Physical examination | Surgery | Size | Fig. 2 | |
|---|---|---|---|---|---|---|
| Patient 1 | 23-year-old male | 3 years | PO on ML, scar from previous drainage on left side, IC | Karydakis on left side with lower left extension | 12cm | A1–B1 |
| Patient 2 | 42-year-old male | 17 years | Several PO on ML, one SO 3cm from LM, IC | Karydakis on left side with upper left extension | 14cm | A2–B2 |
| Patient 3 | 26-year-old male | 7 years | Several PO on ML, bilateral cranial indurations, IC | Karydakis on right side with superior and left extensions | 16cm | A3–B3 |
ML, midline; PO, primary orifice; SO, secondary orifice; IC, intergluteal cleft.
Diagrams of the technique used: (A1) the skin is marked with an eccentric ellipse 2cm from the midline; (B1) the arrow indicates how a flap is created at the medial edge that is 1cm thick and 2cm long; (C1) suture of the lower and inside edges of the flap to the presacral fascia to cover the defect; (D1) final result, with sutures.
The patients presented good progress, and there were no early postoperative complications, such as infection of the surgical site, subcutaneous collections or suture dehiscence within the first 30 days after surgery. The patients have presented no disease recurrence after 12 months of follow-up.
Pilonidal disease is a very frequent disorder in our setting that affects young men in particular. It is an important socioeconomic and medical problem as it impacts the core of the active working population, resulting in sick leaves, and also due to its chronicity and recurrence.5 Currently, there is no gold standard surgical technique for this disease. The ideal treatment should provide a rapid cure, be minimally invasive, shorten sick leaves, and reduce hospitalization time, morbidity and recurrence.
En bloc resection and primary closure on the midline, which has been the most frequently used technique in our country to date, can generate excessive tension in the surgical wound, especially in large pilonidal sinuses, with high postoperative complication rates, including wound dehiscence, appearance of seromas, surgical site infections and mid/long-term recurrences.
According to the meta-analyses by Brasel et al. and McCallum et al.,1,2 closed resection techniques, in general, have not been shown to be superior to open techniques, and, although they reduce healing time and patients return to daily activities more quickly, the rate of recurrences is higher. These same meta-analyses, as well as the Cochrane review by Al-Khamis et al.,6 state that if a closed technique is chosen, this should be done outside the midline like the Karydakis technique,7 which is considered the surgery of choice for this disease by many authors.
The morbidity described for the Karydakis technique varies greatly in the literature reviewed, with rates ranging from 3.6% to 26%.3,8–10 Although different authors have confirmed the benefits of this procedure, its use has not been generalized, probably because it is technically more difficult than the classical technique and because the incision and the size of the defect can be larger than with other procedures, as published by la Portilla et al.11 in a regional survey in Andalusia in which only 11.5% of those surveyed had ever utilized a flap for the repair of a pilonidal sinus, which was the most often used technique.
We have not found a standardized pilonidal sinus classification according to size or any studies that recommend a specific procedure for larger lesions. Further research is needed in this context. In these cases, given the heterogeneity in the extension and severity of the pilonidal sinus, extensions of the Karydakis technique could be a good method to definitively resolve this disease.
FundingNo funding was received for the completion of this study.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Martinez Sanz N, Peña Ros E, Sánchez Cifuentes A, Benavides Buleje JA, Albarracín Marín-Blazquez A. Técnica de Karydakis modificada para el tratamiento del sinus pilonidal gigante. Cir Esp. 2016;94:609–611.