Cystic echinococcosis (CE) is a zoonosis caused by Echinococcus granulosus larva.1–8 The most frequently affected organ is the liver (70%–80% of patients).1–3,5,9 As there are no randomized trials, it is not clear which is the best treatment for hepatic hydatid cysts (HHC): surgery, percutaneous drainage, medication (albendazole) or observation.1–7
In 1985, a published report proposed puncture as a therapeutic option for HHC. Since then, PAIR therapy (HHC puncture, aspiration of the intracystic content, injection of scolicidal solution and reaspiration) has become consolidated as a valid treatment.1–5,8,9
We present our experience with PAIR in three complex cases of HHC.
Material and MethodsFrom May 2007 to December 2012, the Hepatobiliopancreatic Surgery unit at our hospital treated 107 patients with HHC: 60 were treated; 44 were under periodic observation since they were asymptomatic and presented inactive cysts, refused surgery, or were at high risk for surgery; 3 symptomatic patients were treated with PAIR.
Technique: after 7 days of treatment with albendazole (400mg orally/12h), we performed the PAIR technique. Patients were monitored and under conscious sedation with local anesthesia. An initial CT-guided puncture was done with a 22 G needle, using the Seldinger technique with a 0.018 guide, attempting to pass through part of the liver tissue. After puncture, a dilator system with a 6F sheath was inserted, through which a small quantity of liquid was suctioned (10–20cc) to decompress the cyst. The liquid was analyzed immediately with laboratory diagnostic strips in order to rule out traces of bilirubin and connection with the bile duct; if there was still any doubt, cystography was done. Other samples were sent for microbiology and cytology studies. Using the same Seldinger technique, a 12–14F catheter was inserted with a 0.035″ guide. Through this catheter, 90% of the intracystic liquid was aspirated and 2/3 of the extracted liquid was replaced with a mix of 50% absolute alcohol with hypertonic saline solution (20%), which remained in the cavity for 1h. The catheter was left in for 48h, during which time the patient was monitored in order to assess any possible complications. After radiology follow-up with a CT scan, the catheter was withdrawn.
Patients were prescribed albendazole for 1 month after the PAIR procedure (400mg orally/12h). Follow-up studies at 1, 3 and 6 months included ultrasound and/or CT scan, which were repeated every 6 months thereafter. If we observed that the cyst increased in size or caused symptoms, the procedure was repeated.
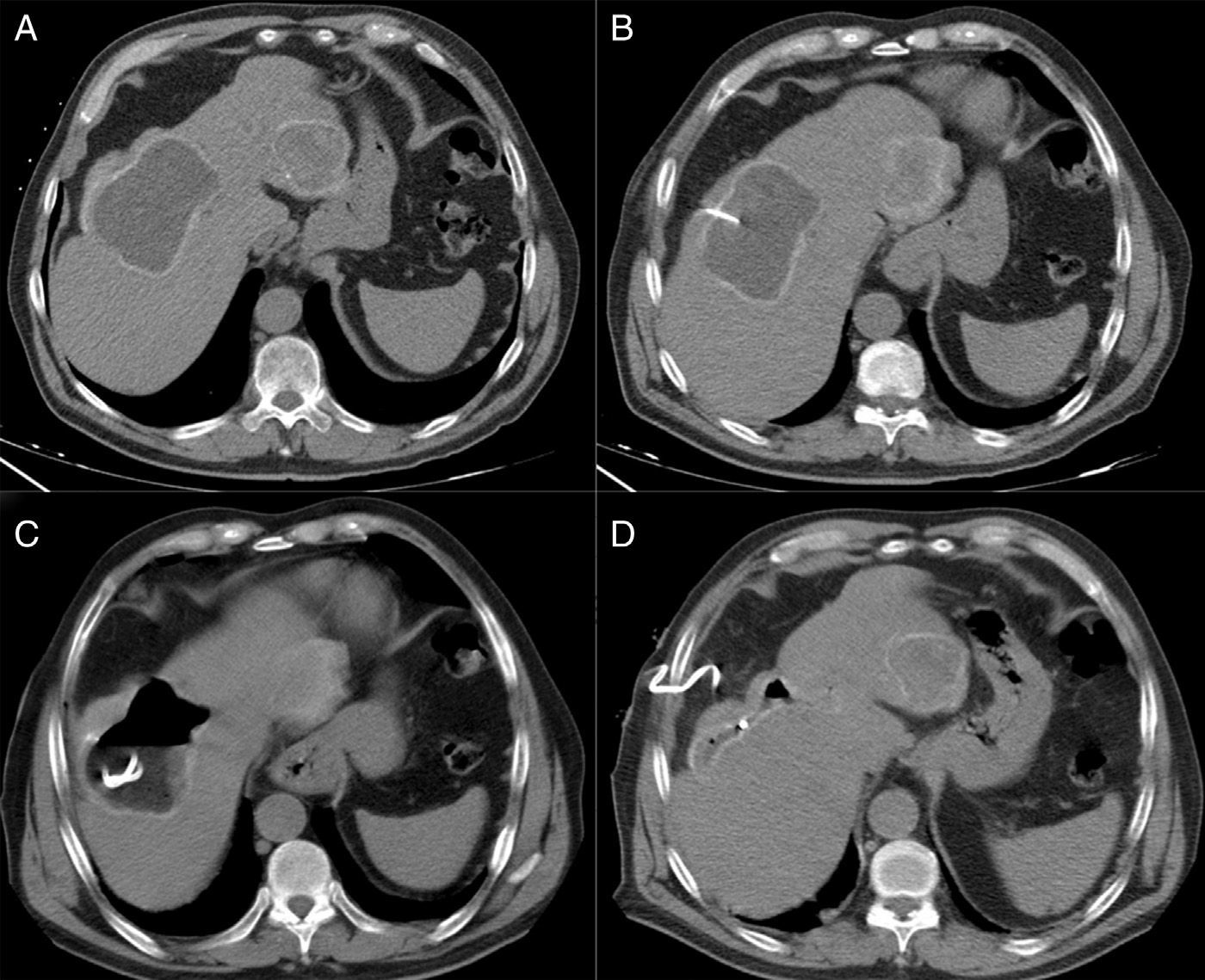
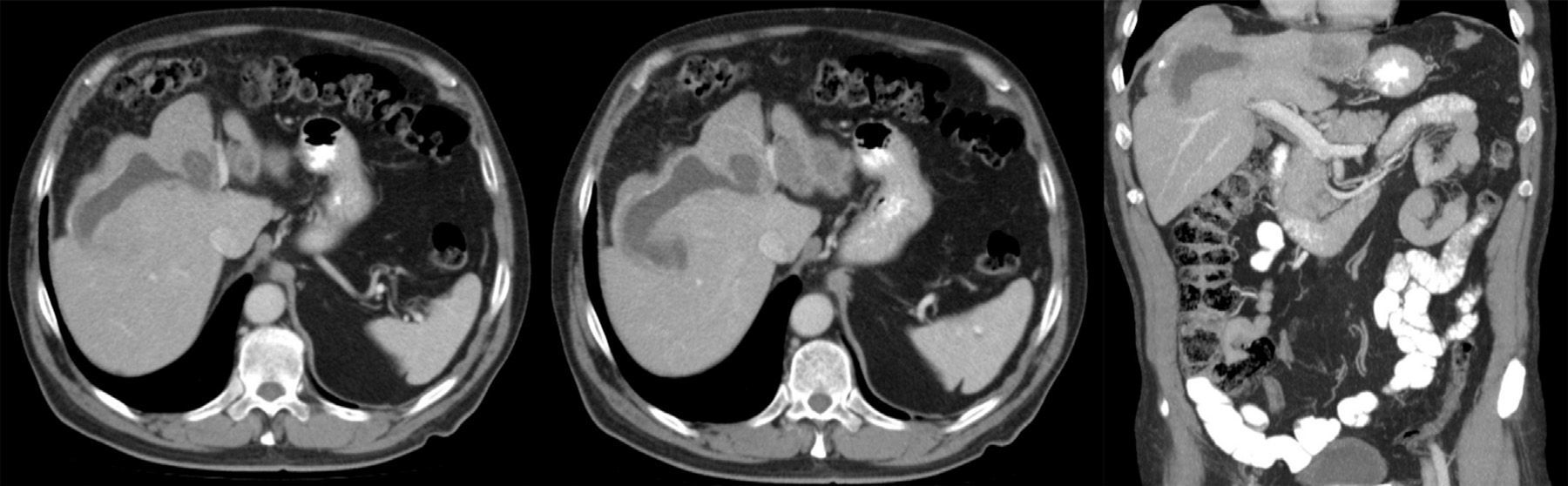
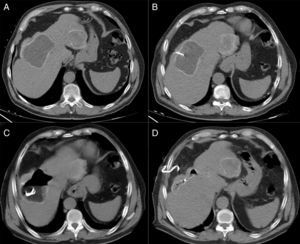
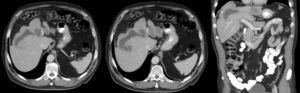
ResultsClinical characteristics are shown in Table 1. One patient presented with obstructive jaundice, and a biliary fistula was ruled out by ERCP and fistulography during PAIR (Fig. 1). The jaundice was probably a result of the compression by the large HHC. Nine months later, this patient had an increased cyst size, so a second PAIR procedure was done (Fig. 2). The second patient presented disseminated hydatidosis with a symptomatic cyst that was punctured. The third patient presented a symptomatic HHC in a small liver remnant after previous surgeries. PAIR was able to resolve the symptoms of these three patients.
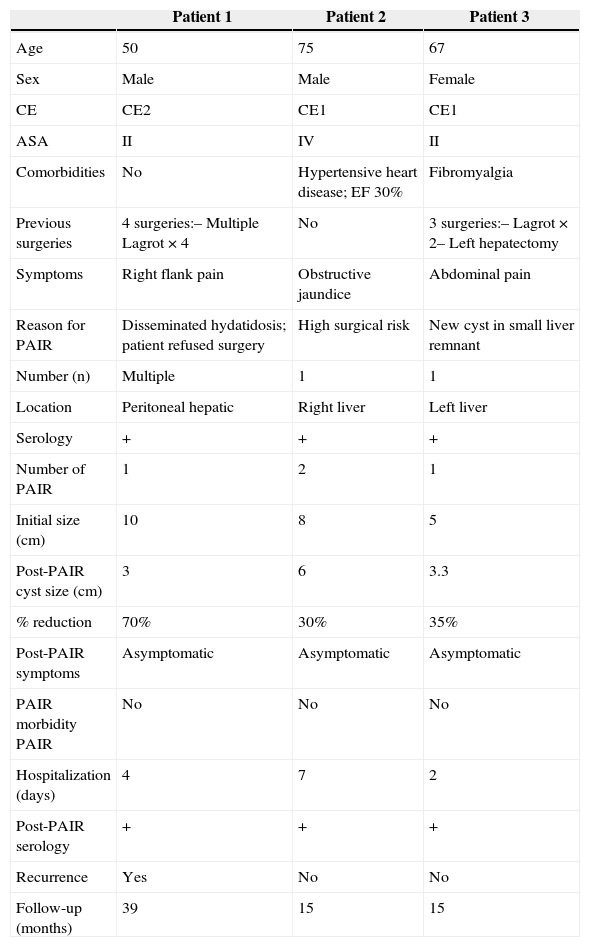
Patient Characteristics.
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age | 50 | 75 | 67 |
| Sex | Male | Male | Female |
| CE | CE2 | CE1 | CE1 |
| ASA | II | IV | II |
| Comorbidities | No | Hypertensive heart disease; EF 30% | Fibromyalgia |
| Previous surgeries | 4 surgeries:– Multiple Lagrot×4 | No | 3 surgeries:– Lagrot×2– Left hepatectomy |
| Symptoms | Right flank pain | Obstructive jaundice | Abdominal pain |
| Reason for PAIR | Disseminated hydatidosis; patient refused surgery | High surgical risk | New cyst in small liver remnant |
| Number (n) | Multiple | 1 | 1 |
| Location | Peritoneal hepatic | Right liver | Left liver |
| Serology | + | + | + |
| Number of PAIR | 1 | 2 | 1 |
| Initial size (cm) | 10 | 8 | 5 |
| Post-PAIR cyst size (cm) | 3 | 6 | 3.3 |
| % reduction | 70% | 30% | 35% |
| Post-PAIR symptoms | Asymptomatic | Asymptomatic | Asymptomatic |
| PAIR morbidity PAIR | No | No | No |
| Hospitalization (days) | 4 | 7 | 2 |
| Post-PAIR serology | + | + | + |
| Recurrence | Yes | No | No |
| Follow-up (months) | 39 | 15 | 15 |
EF: ejection fraction; PAIR: puncture, aspiration, injection, reaspiration.
Patient from Fig. 1, 12 months after the PAIR technique.
Surgery is the only technique that is able to cure this pathology and the only option for patients with complicated HHC.1–9 Percutaneous treatment of HHC, usually combined with albendazole, has grown in popularity, and it is considered the best therapeutic option in many underdeveloped countries.1–6,8,9
The most widely recognized indications for PAIR are: CE1 and CE3a HHC, infected cysts, pregnancy, failed treatment with albendazole, inoperable patients or those who refuse surgery, and HHC recurrence after surgery.4,5 This technique has a recurrence rate of 0%–15%; the results are related with the type of HHC, which are poorer in multivesicular cysts and better in CE1 HHC larger than 5cm and CE3a.3–5 Contraindications include: CE4 and CE5 HHC, HHC that are inaccessible by puncture or high-risk, and HHC connected to the bile duct.5,6 The use of PAIR in CE2 and CE3b HHC is controversial.5
The benefits of PAIR include: diagnostic confirmation, elimination of parasitic material, low morbidity and almost no mortality, shorter hospitalization and lower cost than surgical techiques.3,5,8,9 The complications described are typical of any liver puncture (bleeding), while others are specific to PAIR: biliary fistula after cystic decompression, sclerosing cholangitis if there is passage of scolicidal solution to the bile duct, cyst infection, parasitic dissemination, systemic toxicity from the injected liquid and anaphylactic reactions.5,9 In cysts larger than 10cm, it is recommended to always leave in a drain tube for 48h.5
One of the disadvantages of PAIR is the follow-up evaluation, since a residual lesion remains and its degree of activity remains unknown.3,4 Kabaaalioglu et al. have created a classification in order to quantify the results after PAIR based on the volume lost and post-puncture radiological characteristics.4
Unlike other countries with endemic areas of hydatidosis, in Spain the use of PAIR is anecdotal, and surgery continues to be the main treatment.7 Asymptomatic patients or those who refuse surgery or in whom surgery is contraindicated due to comorbidities, treatment usually includes albendazole, but not PAIR. The problem arises in symptomatic patients who cannot be treated by surgery and when albendazole therapy has not provided good results or cannot be used due to intolerance or allergy. In this short series, we present patients with uncommon indications, since PAIR is usually used in other countries in patients with univesicular cysts that are uncomplicated and less complex.3,5
In conclusion, PAIR can be useful in patients with complex, symptomatic HHC that cannot be treated surgically, thereby avoiding interventions with high surgical risk. Although the short follow-up does not provide for long-term conclusions, we were able to resolve extreme situations with zero morbidity.
Please cite this article as: Ramia JM, del Cerro J, de la Plaza R, Adel F, García-Parreño J. Punción, aspiración, instilación y re-aspiración en casos complejos de hidatidosis hepática. Cir Esp. 2015;93:e45–e47.