Diverticulosis of the appendix is an uncommon disease with an incidence in appendectomy specimens that ranges between 0.004% and 2.1%.1,2 Diverticula may cause the inflammatory process, although occasionally they are findings that are not directly related with the acute appendiceal symptoms. Symptoms of appendiceal diverticulitis are difficult to distinguish from acute appendicitis.3 It is usually diagnosed as an incidental finding in the surgical specimens from interventions due to acute abdomen and associated with the finding of appendicitis.
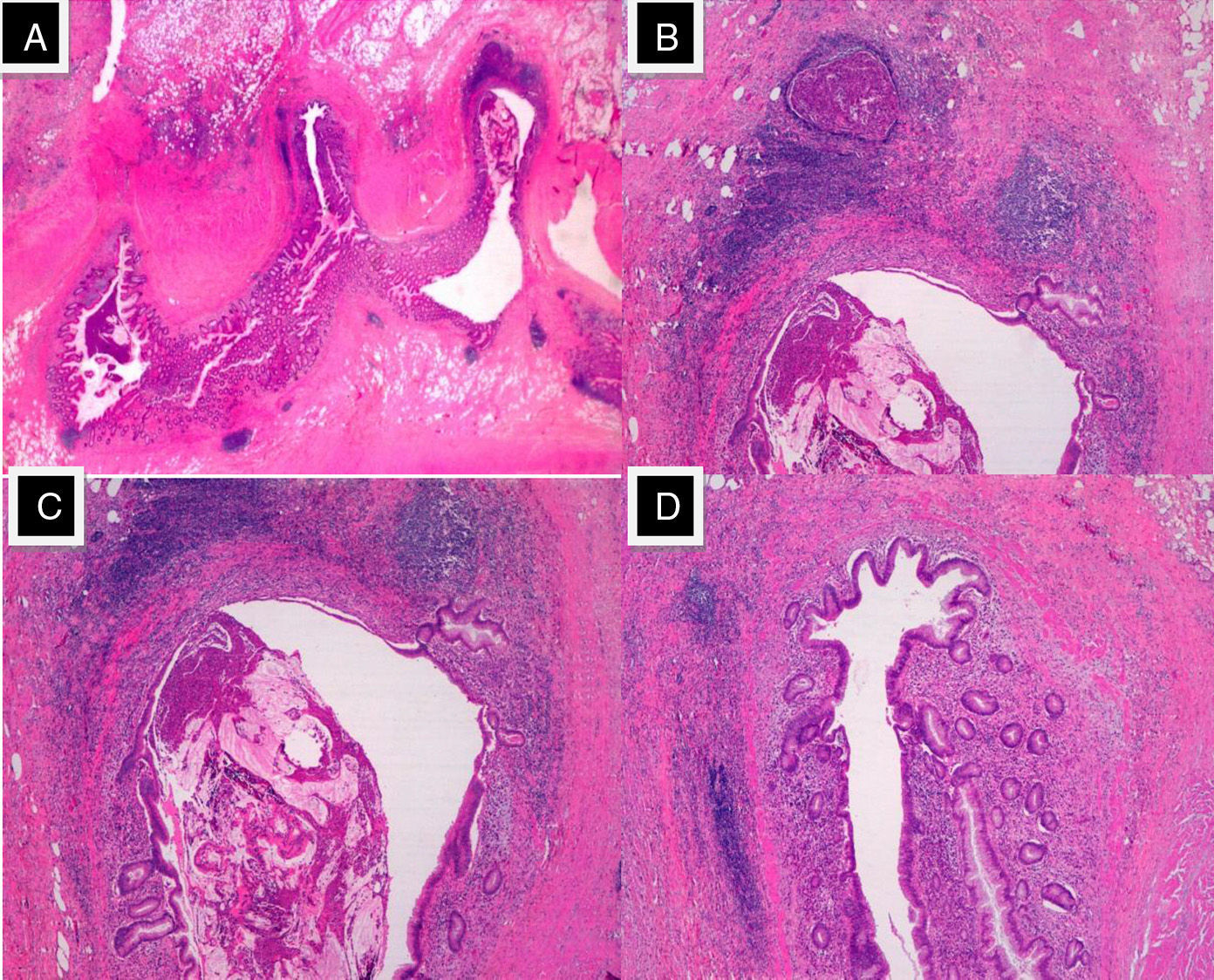
We present a case of diverticulosis in a 54-year-old woman who complained of abdominal pain over the course of the previous 3 days, which was initially located in the right iliac fossa (RIF) and accompanied by fever. Examination detected abdominal pain and guarding in the RIF with positive Blumberg sign. No acute phase reactants were observed in the blood sample. Abdominal ultrasound of the RIF showed a tubular structure with a sac-like end measuring 8mm in thickness, with an adjacent hypoechoic area and increased echogenicity of the adjacent mesentery with a small formation of free fluid (Fig. 1). With the diagnosis of an acute appendiceal condition, we operated by means of a McBurney incision and observed the cecal appendix with diverticula along its entire length. Those that were situated at the more distal end presented signs of inflammation, with important mesenteric thickening. Appendectomy was performed. The postoperative recovery was uneventful and the patient was discharged on the third postoperative day. The pathology study of the specimen reported diverticulosis of the vermiform appendix, accompanied by mucocele and abscesses rich in eosinophils. No appendicular parasites were identified (Fig. 2).
(A) Multiple “false” diverticula on the mesenteric edge of the distal end of the appendix (HE, 4×); (B and C) diverticular wall made up of mucosa and muscularis mucosae, pushing the muscularis propria and forming eosinophil abscesses. (HE, 20×); (D) diverticula occupied by mucus (mucocele) and a large eosinophil content (HE, 40×).
The presence of diverticula in the cecal appendix was described for the first time by Kelynak in 1893. The appearance of diverticulosis of the appendix is exceptional, with a mean incidence of around 1%.1 Diagnosis is usually incidental, generally during the pathology study of the appendix. Appendiceal diverticulitis is an inflammatory clinicopathological disease that is different from acute appendicitis; it is more common in men around the fifth decade of life and presents a higher mortality rate.3 Morphologically, there are 2 main subtypes of diverticula: true and false. True or congenital diverticula are caused by abnormal intestinal permeability in the solid phase. Meanwhile, pseudodiverticula, false diverticula or acquired diverticula (mean incidence 1%) are caused by increased pressure on the least resistant points of the appendix wall; they are generated by high pressure and made up of the mucosa.1,2 Our case presented diverticulosis with several false diverticula caused by pressure that were located distally.
According to the pathological changes of the diverticulum and the appendix, various main forms of presentation can be differentiated2,4: acute diverticulitis without appendiceal inflammation; diverticulitis and acute appendicitis; uncomplicated diverticular disease and acute appendicitis; and, last of all, uncomplicated appendiceal diverticulitis with normal appendix. Of these, our case fits with the second scenario of associated appendicitis and diverticulitis. Since the symptoms secondary to complicated appendiceal diverticulosis (inflammation and perforation) are usually indistinguishable from the abdominal pain caused by inflammation of the appendix, the findings are usually incidental after appendectomy.5 Appendicular diverticulosis is usually asymptomatic.3,6 It tends to progress with subacute inflammation with the appearance of abscesses and perforation, causing abdominal pain similar to that of acute appendicitis.2,3 Less frequently, there are other complications of diverticulosis of the appendix, including acute hemorrhage due to rupture of the appendiceal artery, edema of the mouth of the diverticulum, pseudotumor formations (appendiceal pseudomyxoma), luminal obstruction by foreign bodies or fecalomas, appendiceal fibrosis and appendico-ileo-vesical fistula.7
With regards to preoperative diagnosis, there are authors1 that affirm that the ultrasound findings in appendiceal diverticulitis, such as thickened and echogenic appendix wall, are due to the presence of air. Multidetector CT can be very useful as it has detected acute appendiceal diverticulitis in 86% of cases with pathologically confirmed appendiceal diverticulitis.8,9 According to other authors,6,10 preoperative imaging tests do not contribute to the definitive diagnosis because diagnosis is mainly determined by the histology study. As for treatment, complicated diverticulosis is treated with appendectomy.3 In asymptomatic cases diagnosed incidentally, prophylactic appendectomy is recommended due to the higher risk of perforated appendix and mortality that is associated with the complicated form of this condition.1,10
Please cite this article as: Motos Micó J, Ferrer Márquez M, Berenguel Ibáñez MM, Belda Lozano R, Moreno Serrano A. Diverticulitis apendicular: un diagnóstico a tener en cuenta en el abdomen agudo. Cir Esp. 2015;93:e49–e51.