Primary hyperparathyroidism (pHPT) in MEN1 is characterized by multiglandular disease and early involvement of parathyroid glands at different times. Persistence and recurrence range from 25% to 35%.
The purpose was: (a) to describe the experience and the treatment of patients with pHPT in MEN1; (b) to analyze the variables related with clinical presentation and recurrence.
MethodA total of 97 patients with MEN1 were diagnosed in a tertiary hospital. A retrospective analysis was made in patients with pHPT (n=71). Study variables: age at diagnosis, mutation, clinical presentation, laboratory tests, surgical technique, and recurrence of HPT.
ResultsMean age was 38 years, and 50 patients were asymptomatic. The surgical technique was: subtotal parathyroidectomy (n=55), resection of three glands (n=7), and resection of less glands (n=9). Transcervical thymectomy was performed in 53 patients. Mean follow-up was 102.9 months. There were 21 recurrences, There were correlations between age at diagnosis and serum calcium levels with the presence of symptoms (P<.0001). There were also correlations between recurrence and surgical technique (P<.03), non-association with thymectomy (P<.0001), and follow-up time (P<.03).
ConclusionPerforming genetic and clinical screening allows us to make a diagnosis in the asymptomatic period and to provide early treatment for HPT in MEN1. The recurrence rate is high, and follow-up time and the surgical technique used are risk factors for recurrence.
El hiperparatiroidismo (HPT) asociado al MEN 1 se caracteriza por ser una afectación multiglandular, no afectándose todas las glándulas en el mismo momento. Suele ser asintomático, aunque la afectación ósea es elevada en los pacientes jóvenes. Las tasa de recidiva y persistencias es de 25-35%.
Los objetivos fueron: a) estudiar HPT-MEN 1; y b) analizar las variables relacionadas con la presencia o no de clínica y con la persitencia.
MétodoDe 97 sujetos con MEN 1 diagnosticados en el HUVA, Murcia, pertenecientes a 16 familias, se han estudiado restrospectivamente 71 pacientes con afectación paratiroidea. Las variables estudiadas son: mutación, edad de diagnóstico, clínica, los valores de calcio, fóforo y PTHi, MIBI, técnica quirúrgica, valores de la PTHi y tasa de recidiva.
ResultadosLa edad media fue de 38 años, y 50 estaban asintomáticos en el momento del diagnóstico. La técnica quirúgica realizada fue: paratiroidectomía subtotal (n=55), paratiroidectomía de 3 glándulas (n=7) y resección de menos de 3 glándulas (n=9). Se asoció timectomía transcervical en 53. El seguimiento medio ha sido de 102,9 meses. Se han encontrado 21 recidivas (10 cirugía incompleta). Encontramos una relación estadísticamente significativa entre: la edad de diagnóstico (p<0,0005) y los valores elevados de calcio (p<0,008) y la presencia de clínica en el momento del diagnóstico, la técnica quirúrgica incompleta (p<0,003), no timectomía (p<0,0001) y seguimiento (p<0,001) y la recidiva tras la cirugía.
ConclusiónLa realización de screening genético y clínico nos permite un diagnóstico en fase asintomática y tratamiento precoz, evitando así complicaciones secundarias a la evolución del HPT. La tasa de recidiva del HPT en el MEN 1 es elevada, siendo los factores de recidiva el tiempo de seguimiento y la técnica quirúrgica realizada.
Primary hyperparathyroidism (pHPT) is the most prevalent endocrine disease in MEN1 syndrome, affecting nearly 100% of patients with this syndrome. It usually appears after the second decade of life, and practically 95% of patients have developed it before the age of 40. Thus, in more than 80% of patients with MEN1, HPT is present at the time of diagnosis. It remains asymptomatic for years, so the diagnosis is made with the detection of calcium and parathyroid hormone (PTH) prospectively in the carrier.1–4 The concept of “asymptomatic” is debatable. On the one hand, it is difficult to properly assess whether certain supposedly nonspecific symptoms are a result of the disease. On the other hand, the bone disease can be severe, yet cause few clinical symptoms. Metabolic bone disease, osteopenia and osteoporosis usually present at an early age.5
Another controversy is determining when the surgical indication should be made in a patient with pHPT-MEN1 and what surgery should be performed. Currently the surgical indication is based on the same criteria used for sporadic pHPT. It is important to bear in mind that the time that is decided for performing parathyroidectomy may be influenced by possible differences in gland size, symmetry of the hyperplasia and technical difficulty, since the histological lesion is a hyperplasia of main cells affecting the 4 glands unequally.6 There is also a consensus that the best initial intervention for patients with pHPT-MEN1 consists of bilateral exploration with subtotal parathyroidectomy, marking the remnant, and bilateral transcervical thymectomy based on the presence of multiglandular disease.5–7 Total parathyroidectomy with autotransplantation has also occasionally been proposed as the treatment of choice for pHPT-MEN1. However, it seems to be associated with a higher rate of permanent hypoparathyroidism, no improved hypercalcemic control8 and possible early recurrence in the area of the autotransplantation. There are authors who defend more selective techniques that are less aggressive, although the associated recurrence rates are higher than 90%.
Both techniques, subtotal and total parathyroidectomy with autotransplantation, have pHPT-MEN1 persistence rates of 20%–25% and recurrence rates of up to 30%. In other words, approximately half of patients will require at least 2 interventions to control their HPT.5–7 This implies that the follow-up of these patients is indefinite.
The high rate of recurrence entails a high number of parathyroid reoperations, which are followed by a number of complications that, even in expert hands, is not negligible. These range from hypoparathyroidism rates from 4% to 16% and permanent recurrent paralysis at around 25%.9
The objective of this study is to determine whether in HPT-MEN1 there are factors that are related with the presence or absence of clinical signs, as well as recurrence after surgery.
MethodsOut of the 97 patients with MEN1 (16 families) diagnosed with genetic studies (mutation in the menin gene), 71 patients with pHPT who were diagnosed and treated at the Virgen de la Arrixaca University Hospital have been included in this study.
The study variables included:
A. General data (demographic and clinical).
- 1.
Age at diagnosis: age of the subject in years at the time HPT was diagnosed;
- 2.
Gender: male or female;
- 3.
Mutation detected in each subject;
- 4.
Clinical characteristics: 2 patient groups were defined according to the diagnostic method of the syndrome: genetic or clinical.
- a)
Patients without disease: subjects without symptoms and diagnosis of HPT,
- b)
Patients with disease: subjects who present symptoms and signs related with HPT (bone pain, recurrent nephritic colic, depression and dyspepsia).
B. Laboratory data and location studies:
- 1.
Calcium and PTH levels at diagnosis.
- 2.
Parathyroid scintigraphy: persistence of radiotracer in imaging studies after 2h was considered pathological. The MIBI results were assessed, determining the number of glands detected.
- 3.
Cervical ultrasound: for the detection of parathyroid and/or thyroid disease.
C. Assessment of bone involvement:
- 1.
Bone densitometry to evaluate bone involvement. The results obtained were classified according to WHO criteria: normal=T-score between +1 and −1 SD; osteopenia=T-score between −1 and −2.5 SD; osteoporosis=T-score>2.5 SD; severe osteoporosis=T-score>2.5 SD+fracture.
D. Surgery:
- 1.
Surgical technique performed in parathyroid glands (parathyroidectomy of one or several glands, subtotal or total parathyroidectomy with autotransplantation) as well as the thymus (thymectomy yes/no). The variation of the technique in each case was due to the evolution in our knowledge of pHPT in patients with MEN1. After 1992, the standard technique was subtotal parathyroidectomy associated with bilateral transcervial thymectomy. Complete surgery was defined as a subtotal parathyroidectomy (after the identification of 4 glands, excision of at least 3, leaving a remnant of approximately 50mg, equivalent to the size of a normal gland).
- 2.
Postoperative complications:
- a.
Definitive hypoparathyroidism when the calcium levels are less than 8.5mg/dL one year after surgery (we did not consider PTH levels).
- b.
Recurrent lesion, defined as the alteration in voice tone, timbre or intensity associated with vocal cord paralysis confirmed by laryngoscopy; considered definitive if persisting 12 months after surgery.
- a.
- 3.
Follow-up:
- -
Mean follow-up time (months),
- -
Cure rate,
- -
Recurrence rate.
- -
- 4.
Recurrence, defined as the presence of hypercalcemia after a period great than or equal to 6 months of normocalcemia.
- -
Mean appearance time,
- -
Descriptive study of cases,
- -
Study of the factors for recurrence.
- -
After carrying out the descriptive study, we evaluated the possible factors related with the presence of clinical symptoms in pHPT-MEN1 and the recurrence rate.
Descriptive statistics were conducted. To test the hypothesis, the Student's t-test was used to compare the quantitative variables, and Pearson's chi-squared test was used for the qualitative variables, with an analysis of adjusted standardized residuals.
A P<.05 was considered significant. Finally, a multivariate logistic regression analysis was performed with calculation of the odds ratio and its 95% confidence interval.
ResultsDescriptive StudyThe mean age of the 71 subjects studied with HPT was 38 (SD: 14.5; range: 17–75), with 41 women (57.7%).
The mutations found in these 71 patients were the following:
- •
c.1546 del C: 61 cases,
- •
c.1546 ins C: 5 cases,
- •
c.1263 C>T: 2 cases,
- •
c.599 del G: 3 cases.
Out of the 71 patients with HPT, 50 (70.4%) had clinical signs related with HPT and 21 (29.6%) did not; 68.1% had bone pain, 60.2% nephritic colic, 30% neurological symptoms and 27.3% epigastralgia.
The mean values of calcium and PTH were 11.5mg/dL (SD: 0.8; range: 10.2–14) and 146.1ng/mL (SD: 99.1; range: 23–610), respectively.
57 patients underwent parathyroid MIBI scintigraphy before the procedure, detecting one gland in 25 subjects, 2 glands in 23, 3 glands in 2 cases and 4 glands in 3 cases; it was negative or uncertain in 4 cases. No ectopic glands were detected. The sensitivity of the MIBI was 45%.
All patients underwent a cervical ultrasound that detected a pathological process in the thyroid in 9.1% of the cases and parathyroid disease in 7%.
Out of the 31 bone densitometry studies performed, 19 (61.3%) were pathological. Nine patients had osteoporosis and 10 osteopenia.
The surgical techniques were as follows: subtotal parathyroidectomy in 55 cases (76.1%), parathyroidectomy of 3 glands in 7 cases (9.9%), parathyroidectomy of 2 glands in 5 cases (7%) and parathyroidectomy of one gland in 4 cases (7%). Bilateral transcervical thymectomy was also performed in 53 cases (74.6%). After surgery, 8 patients (11.3%) presented transient hypocalcemia, with a mean recovery time of 33 days (SD 7.4; range: 20–110), and 3 patients (4.2%) permanent hypocalcemia; in no case was definitive recurrent paralysis detected.
Mean follow-up was 102.9 months (SD: 54.2; range: 12–270). The cure rate after the first surgery was 70.4% (50/71).
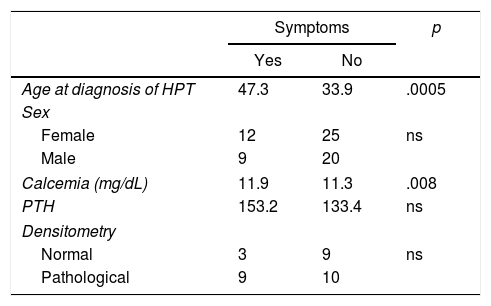
Factors Related With the Presence of Symptoms of Primary MEN1 HyperparathyroidismWhen we compared the groups of patients with and without clinical symptoms (Table 1), we found that the mean age of the subjects without clinical signs was lower than that of the symptomatic patients (33.9 years and 47.3 years, respectively; P<.0005). In addition, the highest calcium levels were found in the group of patients with clinical symptoms (P<.008).
In contrast, we found no relationship between gender, type of genetic mutation, PTH levels, densitometry results and the presence or absence of clinical symptoms.
Factors Related With RecurrenceDuring follow-up, 21 (29.6%) recurrences were diagnosed. The mean age of these patients was 36.5 (SD: 10.7; range: 18–57); 13 were women and 8 men.
In the 21 patients with recurring pHPT, the initial diagnosis of the disease was symptoms-based. Sixteen did not present symptoms, and 5 did. The mean values of calcium and PTH were 11.5mg/dL (SD: 0.52; range: 10.7–12.6) and 156.1ng/mL (SD: 60.6, range: 82–300), respectively.
The initial technique performed in these 21 subjects was subtotal parathyroidectomy in 12 cases, parathyroidectomy of 3 glands in 4 cases, parathyroidectomy of 2 glands in 3 cases and parathyroidectomy of one gland in the remaining 2. Associated thymectomy was done in 8 of the 21 cases.
After the first surgery, the mean time transpired before onset of the recurrence was 41 months (SD: 68.7; range: 24–94), which was diagnosed by the increase in blood PTH and calcium levels.
The localization diagnosis was made by MIBI in 20 cases (in 18 cases one gland was detected, and in 2 cases 2 glands, 4 of which were “ectopic”). Cervical ultrasound and CT were performed in 3 patients, finding recurrence in all patients.
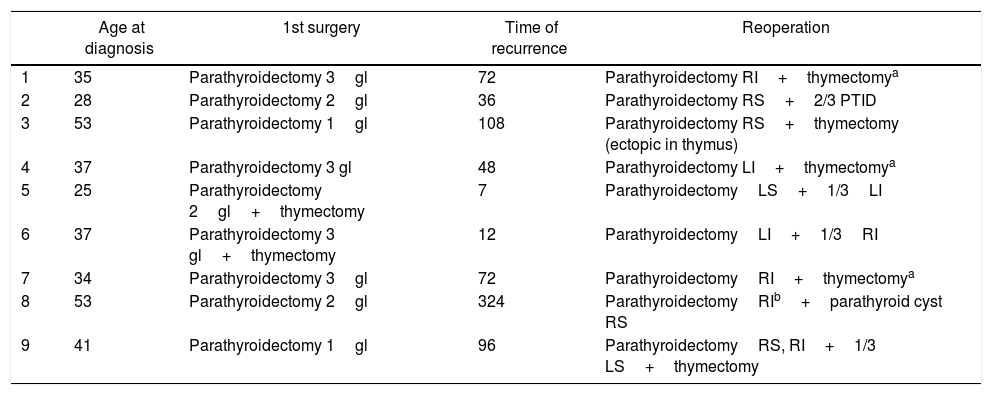
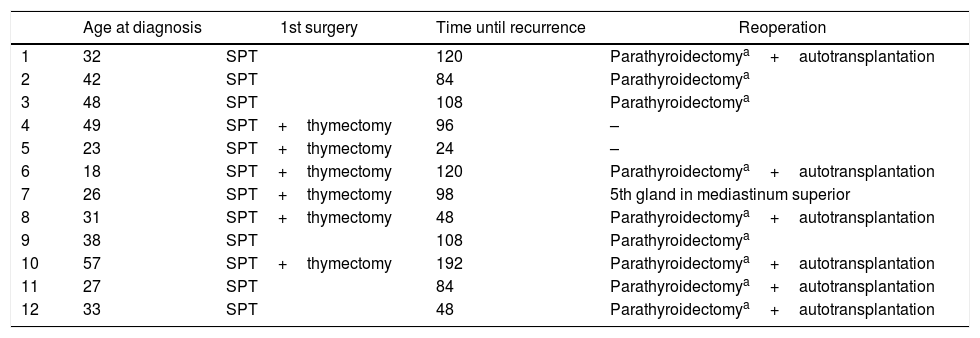
Nineteen patients were reoperated; the surgical technique varied in each case depending on the initial surgery and localization tests. The remaining 2 patients are pending surgery. The results of the initial surgery and of the recurrence are expressed in Tables 2 and 3.
Description of Patients With HPT Recurrence With Initial Incomplete Surgery.
| Age at diagnosis | 1st surgery | Time of recurrence | Reoperation | |
|---|---|---|---|---|
| 1 | 35 | Parathyroidectomy 3gl | 72 | Parathyroidectomy RI+thymectomya |
| 2 | 28 | Parathyroidectomy 2gl | 36 | Parathyroidectomy RS+2/3 PTID |
| 3 | 53 | Parathyroidectomy 1gl | 108 | Parathyroidectomy RS+thymectomy (ectopic in thymus) |
| 4 | 37 | Parathyroidectomy 3 gl | 48 | Parathyroidectomy LI+thymectomya |
| 5 | 25 | Parathyroidectomy 2gl+thymectomy | 7 | ParathyroidectomyLS+1/3LI |
| 6 | 37 | Parathyroidectomy 3 gl+thymectomy | 12 | ParathyroidectomyLI+1/3RI |
| 7 | 34 | Parathyroidectomy 3gl | 72 | ParathyroidectomyRI+thymectomya |
| 8 | 53 | Parathyroidectomy 2gl | 324 | ParathyroidectomyRIb+parathyroid cyst RS |
| 9 | 41 | Parathyroidectomy 1gl | 96 | ParathyroidectomyRS, RI+1/3 LS+thymectomy |
gl: glands; RI: right inferior parathyroid; LI: left inferior parathyroid; RS: right superior parathyroid; LS: left superior parathyroid.
Description of the Patients With HPT Recurrence After Complete Initial Surgery.
| Age at diagnosis | 1st surgery | Time until recurrence | Reoperation | |
|---|---|---|---|---|
| 1 | 32 | SPT | 120 | Parathyroidectomya+autotransplantation |
| 2 | 42 | SPT | 84 | Parathyroidectomya |
| 3 | 48 | SPT | 108 | Parathyroidectomya |
| 4 | 49 | SPT+thymectomy | 96 | – |
| 5 | 23 | SPT+thymectomy | 24 | – |
| 6 | 18 | SPT+thymectomy | 120 | Parathyroidectomya+autotransplantation |
| 7 | 26 | SPT+thymectomy | 98 | 5th gland in mediastinum superior |
| 8 | 31 | SPT+thymectomy | 48 | Parathyroidectomya+autotransplantation |
| 9 | 38 | SPT | 108 | Parathyroidectomya |
| 10 | 57 | SPT+thymectomy | 192 | Parathyroidectomya+autotransplantation |
| 11 | 27 | SPT | 84 | Parathyroidectomya+autotransplantation |
| 12 | 33 | SPT | 48 | Parathyroidectomya+autotransplantation |
The causes of recurrence in the 10 cases treated with complete surgery were due to hyperplasia of the remnant in 8 cases and due to the presence of a fifth gland in one case.
After the second surgery, all patients presented normal calcium and PTH levels, with a follow-up of 124.4 months (SD: 51.6; range: 48–180).
The type of parathyroidectomy, the performance or not of thymectomy and the mean follow-up time were factors that significantly correlated with recurrence (Table 4).
Factors Associated With HPTP-MEN1 Recurrence.
| Recurrence | p | ||
|---|---|---|---|
| Yes | No | ||
| Age at diagnosis of HPT | 36.4 | 39.4 | Ns |
| Sex | |||
| Female | 13 | 28 | Ns |
| Male | 8 | 22 | |
| Calcemia (mg/dL) | 11.6 | 11.6 | Ns |
| PTH | 162.7 | 145 | Ns |
| Symptoms | |||
| Surgical technique | |||
| Subtotal parathyroidectomy subtotal | 12 | 43 | .003 |
| Parathyroidectomy, 3 glands | 4 | 3 | |
| Parathyroidectomy, 2 glands | 3 | 2 | |
| Parathyroidectomy, 1 gland | 2 | 2 | |
| Thymectomy bilateral | |||
| Yes | 8 | 45 | .0001 |
| No | 13 | 5 | |
| Mean follow-up (months) | 109.0 | 39.04 | .001 |
P<.05: statistically significant.
MEN1 syndrome is an autosomal dominant hereditary disorder caused by the presence of a mutation in the MEN1 gene located in the 11q13 region. It is characterized by the appearance of hyperfunction or hyperplasia of 2 or more endocrine glands, mainly affecting the parathyroid, pituitary and duodenum-pancreas.1,10
Hyperparathyroidism (HPT) is the most frequent affectation in MEN1. Unlike primary HPT (pHPT), where single gland involvement is the most frequent, HPT-MEN1 is characterized by a multiglandular involvement, whose morphological substratum appears to be adenomatous type as the lesions are mainly monoclonal.11,12
pHPT-MEN1 is usually asymptomatic, although the meaning of ‘asymptomatic’ is debatable. On one hand, the non-specific symptoms of PTH can go unnoticed, so the number of symptomatic cases increases when performing the anamnesis is thorough. On the other hand, the bone disease can be severe but cause little or no clinical symptoms. Metabolic bone disease, osteopenia and osteoporosis usually present at an early age. Burgess13 showed that there was severe osteopenia in 44% of MEN1 patients who presented HPT with asymptomatic hypercalcemia. Due to the appearance of early bone involvement, there are authors who advocate performing surgery early on (in the asymptomatic HPT phase). An alternative to surgery would be to perform periodic densitometries in patients with normocalcemia, so that the bone disease would be detected in very early stages.13 The different published studies try to detect which factors are related to the presence of symptoms secondary to the HPT, finding that the most significant is the age of diagnosis, as in our series. The influence of calcemia or PTH levels is more controversial.
pHPT-MEN1 is clinically indistinguishable from sporadic pHPT. Left to its own evolution, it causes the same clinical manifestations although, as we have pointed out, patients present the disease at earlier ages. pHPT-MEN1 can be as serious as the sporadic type if it is not diagnosed early.14
Although the diagnosis of HPT is based on biochemical (calcemia and calciuria) and hormonal (PTH) data, the impact of the disease on each subject (renal function, renal ultrasound, bone densitometry) should also be studied.12–15
Unlike sporadic pHPT, where scintigraphy with sestamibi localizes 80%–90% of adenomas, in the case of HPT in MEN1, its sensitivity decreases significantly. Therefore, the use of scintigraphy in primary HPT surgery in MEN1, aimed at locating the affected glands, is not clear.15 It is recommended to perform scintigraphy in order to locate possible ectopic and/or supernumerary glands, since the literature describes that the frequency of supernumerary glands in MEN1 reaches 30%, which is higher than in the normal population (15%).15 The diagnosis in the scintigraphy of possible ectopic or supernumerary glands, in addition to facilitating surgery, also allows us to remove all the parathyroid tissue, thereby avoiding recurrences. In our experience, as in the literature, the sensitivity of sestamibi to detect multiglandular involvement was very low, not locating ectopic or supernumerary glands in any cases. In contrast, it was effective in the case of reoperations and located the recurrence in all cases, both ectopic glands and recurrence of the remnant.
Currently, the criteria for the indication of surgical treatment for HPT in MEN1 should be based on the same criteria as sporadic HPT,16 although the criterion of the severity of bone involvement is arguable. Thus, surgery should be indicated not only in cases of osteoporosis, but also in cases of osteopenia.16
Due to the characteristics of the syndrome (non-synchronous, multiglandular involvement),14 early surgery would imply less glandular involvement, and therefore more difficulties for complete glandular identification, and perhaps increased risk of postoperative hypocalcemia. Furthermore, late surgery provides a greater probability of performing a satisfactory subtotal parathyroidectomy, but the cost is that the patient will have been exposed to the effects of the disease for a longer period. Parathyroidectomy should be indicated on an individual basis, depending on both the severity of pHPT and age.15,16
Surgical treatment in the HPT of MEN1 should follow 3 basic criteria: (1) to reach and maintain normal calcium levels for as long as possible, avoiding the persistence or recurrence of hypercalcemia; (2) to avoid hypocalcemia secondary to surgery, whose consequences in young patients can be worse than the disease itself; and (3) to facilitate reoperations in recurrent disease.15
Although the majority of expert surgeons advocate surgery based on bilateral exploration using subtotal or total parathyroidectomy with autotransplantation, some recent publications advocate parathyroidectomy only in the affected glands.17 These would actually be enlarged parathyroid glands, because they all have histological involvement. This leads to more recurrences and more reoperations, but a lower risk of hypocalcemia.18 In our series, the cases of surgery with less than 3 glands removed present a recurrence rate greater than 60%. Therefore, it is currently not indicated to perform minimally invasive surgery or surgery where less than 3 glands are removed.
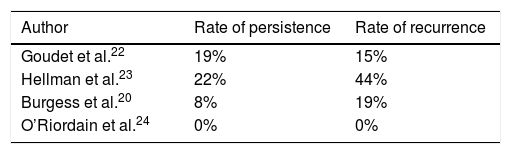
Currently, the most commonly used surgical technique is subtotal parathyroidectomy (SPT); some authors believe that this is an imprecise term that has been used in literature to define various degrees of parathyroid resection.19,20 We would be strictly speaking about SPT when, after the identification of 4 glands, at least 3 of them are removed to leave a remnant of approximately 50mg (equivalent to the size of a normal gland). The size of the remnant can vary from one surgeon to another from 50–60mg to 70–80mg. The results obtained in terms of persistence and recurrence rates varied according to the series, ranging from 0% to 88% and 12% to 33%, respectively19–25 (Table 5). In our experience, the most frequently performed technique has been subtotal parathyroidectomy, with a recurrence rate in these cases of 7.5%, which is comparable to other series. It is expected that this rate will increase when the follow-up of these patients increases. In 16 patients, surgery was incomplete (leaving more than one parathyroid gland). In these cases, the recurrence rate was significantly higher (56.2%; 9/16), which concurs with reports by other authors.26
Similar to recurrence rates, postoperative hypocalcemia rates after SPT vary among the series. While Burgess et al.20 report no hypocalcemia, Hellman et al.22 reported hypoparathyroidism rates of 24% in their series. Hypocalcemia is significantly lower after subtotal parathyroidectomy than after total parathyroidectomy with autotransplantation, since the parathyroid remnant left after a SPT usually has better viability than the autograft.
Another aspect of the surgical technique is related to thymectomy. The purpose of this technique is to eliminate thymic tissue that may harbor supernumerary glands in its interior, which may be the cause of recurring PTH after surgery.
If we analyze the HPT series in MEN1, there are significant differences in the results. They are often not comparable in follow-up time, patient age or surgery conducted.19
Given the high rates of recurrence in HPT associated with MEN1, an attempt has been made to define the factors influencing it. The most important prognostic factor is the follow-up, so that, even after performing the same surgery, those series with longer follow-up times have higher recurrence rates. In our experience, when the mean follow-up was 2.6 years, the recurrence rate was 6.1%; when it was 5.4 years, the recurrences were 5.4%.
The supernumerary glands, the proliferation capacity of the parathyroid cells and the type of surgery have also been related to recurrence.27–31
We can conclude that age at diagnosis and calcium levels are related with the presence or absence of clinical symptoms. Early diagnosis and younger age make it possible to diagnose HPT-MEN1 before bone disease appears. Factors related with the recurrence of PTH are the surgical technique (adequate parathyroid surgery and thymectomy) and follow-up time.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Balsalobre Salmeron M, Rodriguez Gonzalez JM, Ríos A, Febrero B, Parrilla Paricio P. Hiperparatiroidismo primario asociado a neoplasia endocrina múltiple tipo 1 (MEN 1). Experiencia en 71 casos. Cir Esp. 2018;96:627–633.