Different hormones and peptides involved in lipid and carbohydrate metabolism have been studied in relation to morbid obesity and its variation after bariatric surgery. The aim of this study is to evaluate variations in different molecules related to gluco-lipidic metabolism during the first year after sleeve gastrectomy in morbidly obese patients.
Materials and methodsThis is a prospective study in patients undergoing sleeve gastrectomy between November 2009 and January 2011. We analysed changes in different clinical, anthropometric and analytic parameters related with gluco-lipidic metabolism in all patients in the preoperative period, first postoperative day, fifth day, one month, 6 months and one year after surgery. Statistical analysis was performed using SPSS 20.0.
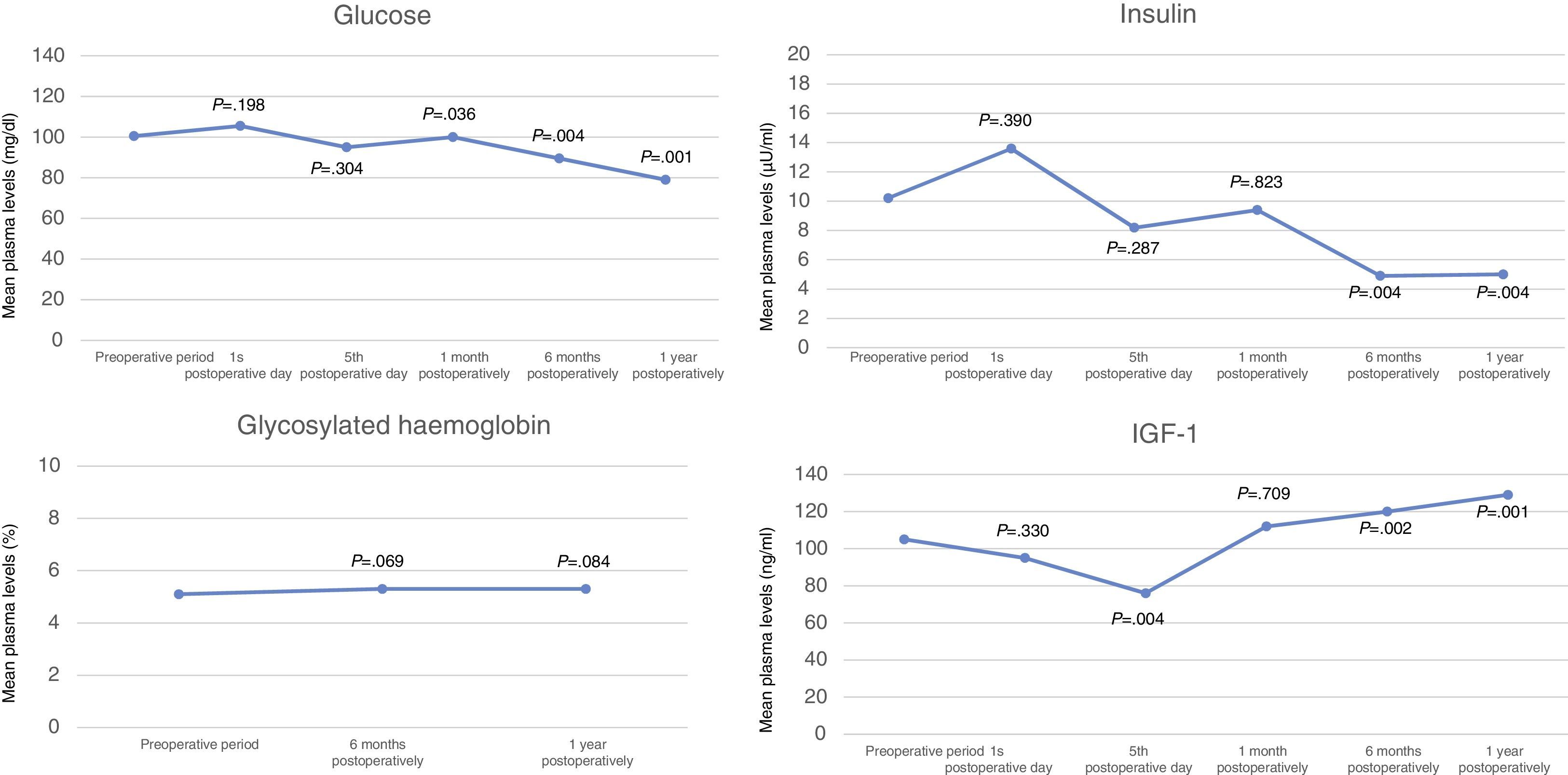
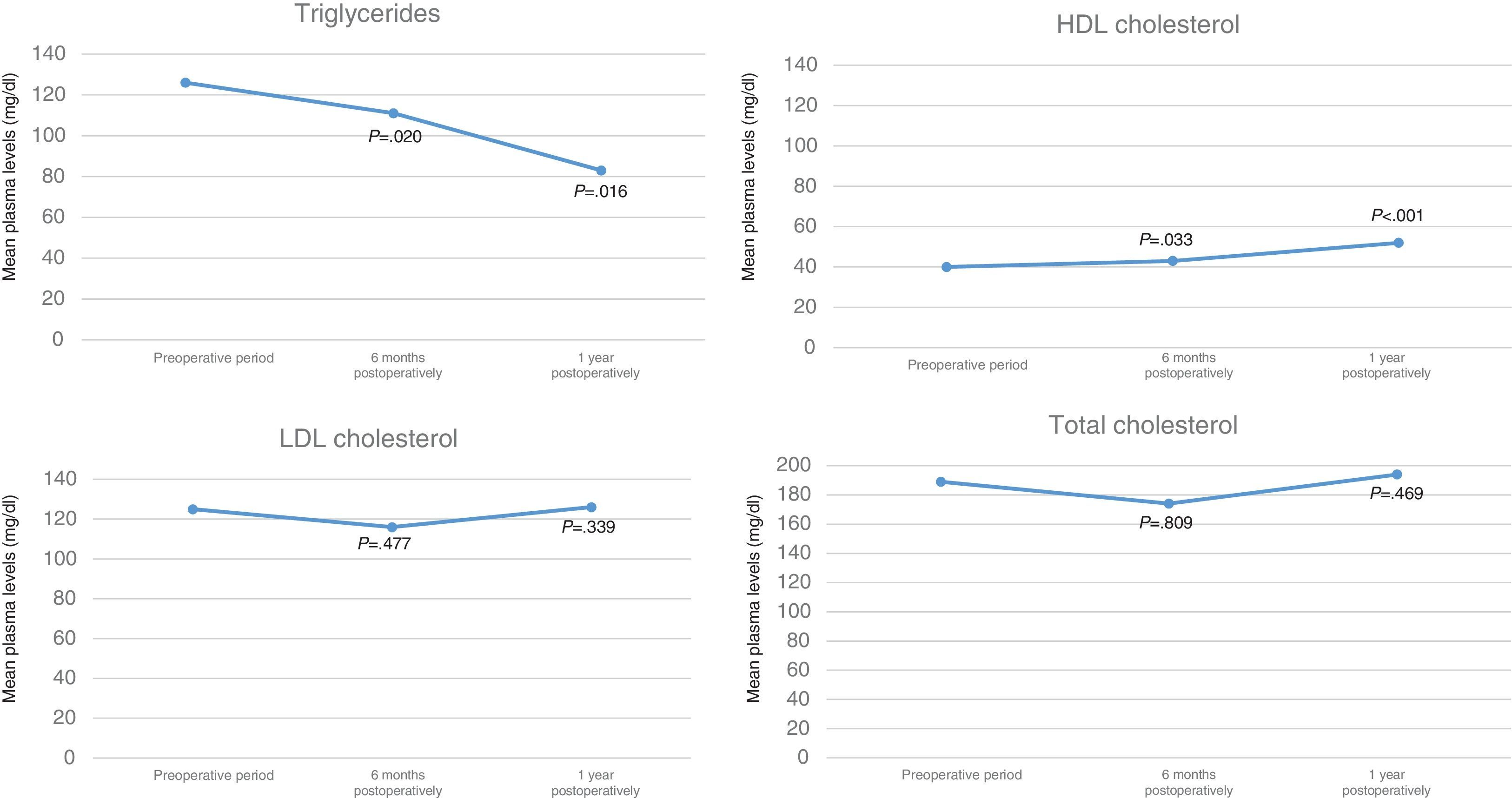
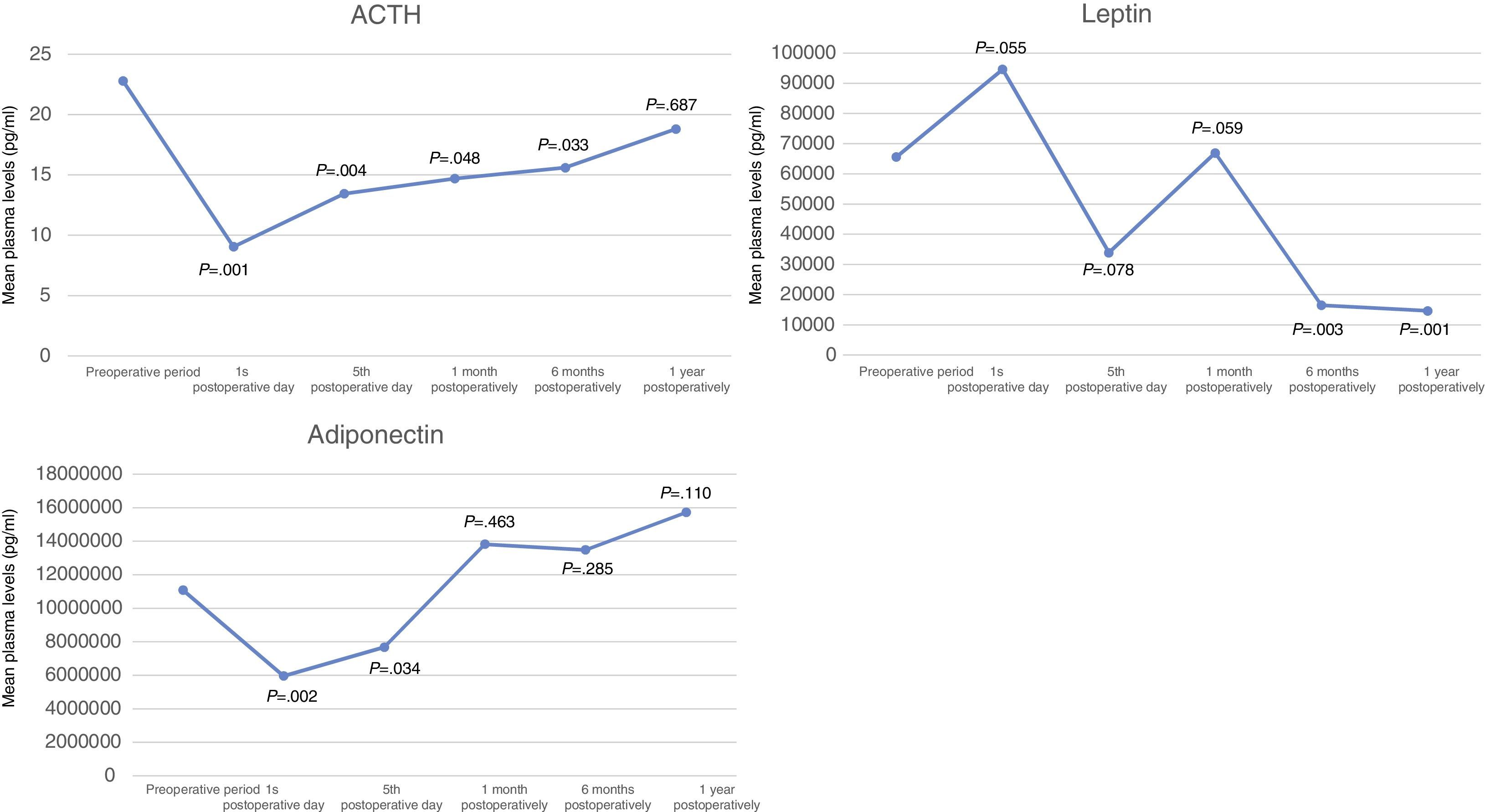
ResultsWe included 20 patients, 60% were women with a median age of 45 years and the median of body mass index (IMC) was 48.5kg/m2, 70% had obstructive sleep apnea syndrome (SAOS), 65% arterial hypertension (HTA), 45% dyslipidemia and 40% diabetes mellitus. One year after surgery, the percentage of excess of BMI loss was 72% and the rate of cure or improvement of dyslipidemia was 100%, diabetes 87.5%, HTA 84.6% and SAOS 57.1%. At this time, glycemia levels decreased significantly (P<.001), and levels of IGF-1 and HDL-cholesterol increased significantly. Levels of adiponectine increased and those of leptine (P=.003), insulin (P=.004) and triglycerides (P=.016) decreased significantly one year after the surgery. ACTH levels (that decreased during first 6 months after surgery), glycosylated haemoglobin, total cholesterol and LDL-cholesterol had no changes one year after surgery.
ConclusionsSleeve gastrectomy is a surgical technique with good results of weight loss and cure of comorbidities. This procedure induces significant modifications in blood levels of gluco-lipidic metabolism related peptides and hormones, such as glucose, IGF-1, insulin, leptin, triglycerides and HDL-cholesterol.
Diferentes hormonas y péptidos implicados en el apetito y el metabolismo lipídico e hidrocarbonado se han estudiado en relación con la obesidad mórbida y su variación tras cirugía bariátrica. El objetivo de nuestro trabajo es evaluar las variaciones de diferentes moléculas relacionadas con el metabolismo glucolipídico durante el primer año tras una gastrectomía vertical en pacientes obesos mórbidos.
Material y métodoEstudio prospectivo en pacientes operados mediante gastrectomía vertical entre noviembre de 2009 y enero de 2011. Se determinaron y analizaron las variaciones en diferentes parámetros clínicos, antropométricos y analíticos relacionados con el metabolismo glucolipídico en todos los pacientes en el preoperatorio, al primer y quinto días, al mes, a los 6 meses y al año postoperatorio, realizando el estudio estadístico con ayuda del programa SPSS 20.0.
ResultadosDe los 20 pacientes estudiados, el 60% eran mujeres con una mediana de edad de 45 años. La mediana del índice de masa corporal (IMC) preoperatorio fue de 48,5kg/m2 y el 70% padecían síndrome de apnea obstructiva del sueño (SAOS), el 65% hipertensión arterial (HTA), el 45% dislipidemia y el 40% diabetes mellitus. Al año de la cirugía, el porcentaje de exceso de IMC perdido fue del 72% y la tasa de curación o mejoría de la dislipidemia fue del 100%, de diabetes el 87,5%, de HTA el 84,6% y de SAOS el 57,1%. En ese período los niveles de glucemia en ayunas disminuyeron de forma significativa (p<0,001), mostrando los niveles de IGF-1 y colesterol HDL un aumento significativo. Los niveles de adiponectina aumentaron y los de leptina (p=0,003), insulina (p=0,004) y triglicéridos (p=0,016) disminuyeron de forma significativa al año de la intervención. Los valores de ACTH (que disminuyeron durante los 6 primeros meses), hemoglobina glucosilada, colesterol total y LDL no experimentaron cambios significativos al año de la intervención.
ConclusiónLa gastrectomía vertical es una técnica que presenta buenos resultados ponderales y de curación de comorbilidades, produciendo modificaciones significativas durante el primer año postoperatorio en los niveles sanguíneos de diferentes parámetros relacionados con el metabolismo glucolipídico como la glucosa, IGF-1, insulina, leptina, triglicéridos y colesterol HDL.
Genetic, environmental and educational factors have been implicated in the development of morbid obesity. There are various alternative approaches to finding a cure, and bariatric surgery has shown the best long-term results. Sleeve gastrectomy has boomed over the past decade and is currently one of the most frequently-used bariatric techniques,1 as it has demonstrated weight-loss outcomes and a cure of comorbidities over and above required standards.
Several studies on morbid obesity have demonstrated how there are many peptides and hormones influencing appetite regulation and lipid and hydrocarbon metabolism and how they change in patients who have undergone bariatric surgery.2
The objective of our study is to determine possible hormone and peptide changes related to glycolipid metabolism in morbidly obese patients who have undergone sleeve gastrectomy.
Materials and MethodsWe performed a prospective, descriptive and analytical study on a total of 20 morbidly obese patients who underwent laparoscopic sleeve gastrectomy in our centre between November 2009 and January 2011.
All the patients fulfilled the indication criteria for bariatric surgery with a body mass index (BMI) above 40kg/m2 or above 35 if associated with other comorbidities. All were informed about the characteristics of the study and signed a specific consent form in order to participate in it.
The surgical technique was performed by the same surgical team, which included 4 surgeons with expertise in bariatric surgery. The surgical approach was laparoscopic using 5 trocars. After releasing the greater gastric curvature, the gastrectomy was performed from 4.5cm in the region proximal to the pylorus up to the angle of His on a 36 Fr intragastric catheter. The integrity of the section line was tested intraoperatively, instilling methylene blue through a nasogastric probe. The specimen was extracted through the incision of one of the trocars situated in the left hypochondrium. A suction drain was placed in all patients, which was removed 3 days after surgery after checking that there were no complications in the oesophagogastric tract.
Different epidemiological variables were collected from the patients: age, gender, BMI, prior medical history, operation details, pre and post-operative laboratory results, assessing weight outcomes, quality-of-life scales (BAROS, Deitel and Reinhold) and data on comorbidities one year after surgery.
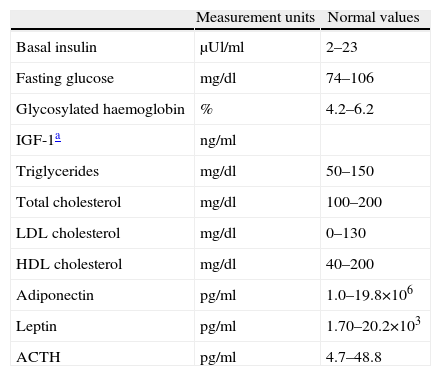
In order to study the specific biochemical parameters of our study (Table 1), 20ml of fasting peripheral blood was taken from all the patients in the morning. Blood samples were taken in gelose tubes and EDTA aprotinin tubes which were sent immediately to be centrifuged at 4°C. The blood and plasma aliquots were stored at −80°C until definitive analysis. The Human Obesity Base, Fluorokine®MAP (R & D Systems) kit, was used to determine adiponectin and leptin levels, and the Luminex analyser to read it.
List of Blood Test Parameters Studied, Measurement Units and Normal Values.
| Measurement units | Normal values | |
| Basal insulin | μUl/ml | 2–23 |
| Fasting glucose | mg/dl | 74–106 |
| Glycosylated haemoglobin | % | 4.2–6.2 |
| IGF-1a | ng/ml | |
| Triglycerides | mg/dl | 50–150 |
| Total cholesterol | mg/dl | 100–200 |
| LDL cholesterol | mg/dl | 0–130 |
| HDL cholesterol | mg/dl | 40–200 |
| Adiponectin | pg/ml | 1.0–19.8×106 |
| Leptin | pg/ml | 1.70–20.2×103 |
| ACTH | pg/ml | 4.7–48.8 |
ACTH: adrenocorticotropic hormone; HDL: high-density lipoprotein; IGF: insulin-like growth factor; LDL: low density lipoprotein.
The blood samples were taken at each of the following times:
- -
Preoperatively.
- -
First postoperative day.
- -
Fifth postoperative day.
- -
First month post-surgery.
- -
Six months after surgery.
- -
One year after surgery.
Triglyceride, total cholesterol, HDL cholesterol, LDL cholesterol and glycosylated haemoglobin levels were analysed preoperatively, after six months and one year after surgery.
The statistical study was performed using the computer programme SPSS 20.0 for Windows®, assessing the evolution of the parameters studied and comparing the preoperative values with those obtained in the other postoperative samples. P values lower than .55 were considered statistically significant.
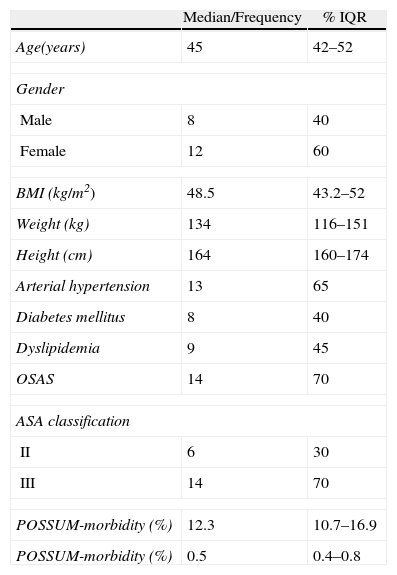
OutcomesTwelve of the 20 (60%) patients included in the study were women, the median age of the series was 45 (IQR: 42–52). The median preoperative BMI was 48.5kg/m2 (IQR: 43.2–52). 70% of the patients had obstructive sleep apnoea syndrome (OSAS), 65% had hypertension, 45% had dyslipidemia, 40% had diabetes mellitus (DM) and 10% were smokers. 70% of them had an anaesthesia risk score of ASA III (Table 2).
Descriptive Study of the Characteristics of the Patients in Our Series.
| Median/Frequency | % IQR | |
| Age(years) | 45 | 42–52 |
| Gender | ||
| Male | 8 | 40 |
| Female | 12 | 60 |
| BMI (kg/m2) | 48.5 | 43.2–52 |
| Weight (kg) | 134 | 116–151 |
| Height (cm) | 164 | 160–174 |
| Arterial hypertension | 13 | 65 |
| Diabetes mellitus | 8 | 40 |
| Dyslipidemia | 9 | 45 |
| OSAS | 14 | 70 |
| ASA classification | ||
| II | 6 | 30 |
| III | 14 | 70 |
| POSSUM-morbidity (%) | 12.3 | 10.7–16.9 |
| POSSUM-morbidity (%) | 0.5 | 0.4–0.8 |
ASA: American Society of Anesthesiologists; BMI: body mass index; IQR: interquartile range; OSAS: obstructive sleep apnoea syndrome.
The median surgery time was 172min (IQR: 150–184). One patient was converted to open surgery due to a haemoperitoneum secondary to an injury to the superior mesenteric vein that occurred as one of the trocars was inserted. There were no other intraoperative complications.
During the post-operative period there were 2 infections of the surgical wound through which the specimen was extracted, one haematoma and one seroma at the same site. One patient was reoperated on due to a suspected fistula of the angle of His; lavage and drainage were performed of the subcardial area, where a small purulent collection was observed but with no evidence of intraoperative leakage, the patient's subsequent progress was satisfactory. There was no mortality associated with the procedure.
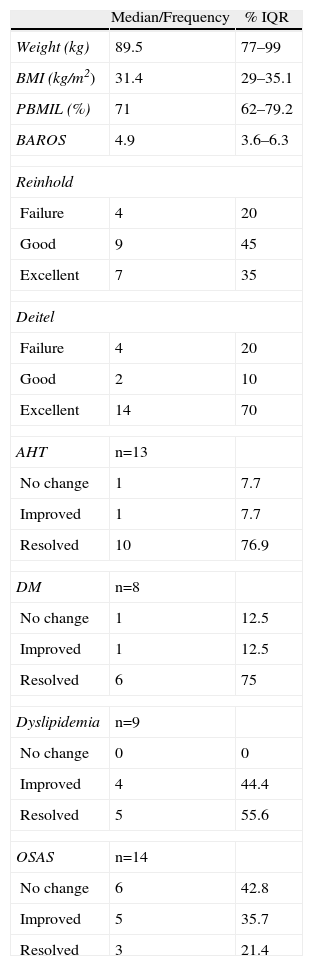
The outcomes in terms of weight, quality of life and cure of comorbidities are shown in Table 3. The median percentage of excess BMI loss (PBMIL) one year after surgery was 71% (IQR: 62–79.2), the BAROS score was 4.9 at this time. One year after surgery, according to Reinhold and Deitel's classifications, the outcome was good or excellent in 80% of the cases (Table 3). The rate of cure or improvement of dyslipidemia one year after surgery was 100%, of diabetes 87.5%, AHT 84% and OSAS 57.1% (Table 3).
Weight Outcomes, Quality of Life and Cure of Comorbidities One Year After Surgery.
| Median/Frequency | % IQR | |
| Weight (kg) | 89.5 | 77–99 |
| BMI (kg/m2) | 31.4 | 29–35.1 |
| PBMIL (%) | 71 | 62–79.2 |
| BAROS | 4.9 | 3.6–6.3 |
| Reinhold | ||
| Failure | 4 | 20 |
| Good | 9 | 45 |
| Excellent | 7 | 35 |
| Deitel | ||
| Failure | 4 | 20 |
| Good | 2 | 10 |
| Excellent | 14 | 70 |
| AHT | n=13 | |
| No change | 1 | 7.7 |
| Improved | 1 | 7.7 |
| Resolved | 10 | 76.9 |
| DM | n=8 | |
| No change | 1 | 12.5 |
| Improved | 1 | 12.5 |
| Resolved | 6 | 75 |
| Dyslipidemia | n=9 | |
| No change | 0 | 0 |
| Improved | 4 | 44.4 |
| Resolved | 5 | 55.6 |
| OSAS | n=14 | |
| No change | 6 | 42.8 |
| Improved | 5 | 35.7 |
| Resolved | 3 | 21.4 |
DM: diabetes mellitus; AHTA: arterial hypertension; BMI: body mass index; PBMIL: percentage of BMI loss; OSAS: obstructive sleep apnoea syndrome.
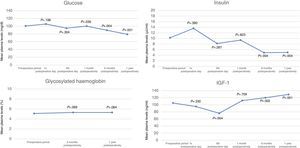
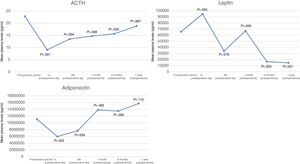
A significant reduction in fasting glycaemia levels was seen on blood analysis six months after surgery (median of 89mg/dl and P=.004) and one year after surgery (median of 79mg/dl and P=.001) with no changes in glycosylated haemoglobin count (Fig. 1). Levels of insulin-like growth factor 1 (IGF-1), after slightly dropping during the first postoperative days, increased significantly with a median of 129ng/dl, one year after surgery (Fig. 1). Median insulinaemia values dropped significantly from six months post surgery (Fig. 1).
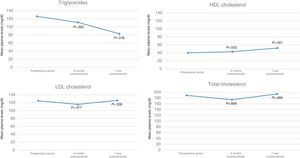
Levels of HDL cholesterol increased significantly, with a median of 52mg/dl (Fig. 2) one year after surgery. Blood triglyceride values went from 126mg/dl preoperatively to 83mg/dl one year later (P=.016), whereas there was no significant change in total and LDL cholesterol levels during this period of follow-up (Fig. 2).
Leptin levels increased on the first postoperative day and subsequently dropped significantly 6 months and 1 year after surgery compared to preoperative levels (Fig. 3). A significant reduction in adiponectin and adrenocorticotropic hormone (ACTH) levels was observed during the first postoperative day which then gradually increased in the remaining tests up to one year after surgery (Fig. 3).
DiscussionMorbid obesity is an increasingly prevalent disease in our society and its aetiology has been related to many socioeconomic, genetic, hormonal and behavioural factors. There is a wide field of research attempting to find new therapeutic targets to achieve optimal weight loss and a cure for the weight-associated diseases which present in these patients.
Bariatric surgery is a therapeutic option which has been demonstrated to achieve the best outcomes in terms of medium and long term weight loss and cure of comorbidities in morbidly obese patients and its cost-effectiveness is favourable.3 Amongst the different techniques which are currently used, sleeve gastrectomy has been experiencing a boom over the past decade. This procedure has gone from representing 5.3% of the total number of bariatric operations performed worldwide during 2008 and is now in second place after gastric by-pass, representing 27.8% of all bariatric operations in 2011,1 partly because it is less technically complex and achieves good outcomes in terms of weight loss and cure of comorbidities, with a PBMIL above 65% and resolution of diabetes and arterial hypertension in more than 80% of the cases,4 as in our series.
The effect of sleeve gastrectomy on hydrocarbate and lipid metabolism has been demonstrated in many studies, since glycaemia, glycosylated haemoglobin levels and lipid fractions normalise,5 as shown by our outcomes. In addition, these good results are achieved early, even before a suitable weight loss, and this supports the fact that many other factors, which are seen to change after gastrectomy, are involved in regulating this complex metabolism.6 It has been demonstrated that levels of ghrelin, a peptide produced in the gastric fundus which causes an increase in appetite as it stimulates the production of different neuropeptides in the arcuate nucleus, reduce after gastric resection in obese patients.7
Leptin is a hormone derived from the adipocytes, levels of which decrease with weight loss; and this occurs early in obese patients who have undergone gastric by-pass.8 It has been demonstrated that physiological increases in its plasma levels are linked to insulin resistance and inhibition of insulin secretion.9 In our results, leptin increases initially, probably in relation to the inflammatory process induced by surgery and subsequently they gradually decrease, which could help to improve our patients’ hydrocarbon metabolism.
A significant, sustained rise in ACTH levels has been demonstrated in gastric by-pass patients during the postoperative period. There have been attempts to explain this as the decrease in leptin levels would reduce the inhibitory effect of this hormone on the hypothalamic–pituitary–adrenal axis.2 In our study, after a very significant drop on the first day after surgery, ACTH levels increased during subsequent follow-up, although they did not exceed preoperative values.
IGF-1 is a polypeptide hormone which is principally secreted by the liver through the effect of the growth hormone. It has a hypoglycaemic action in increasing glucose usage, stimulating its peripheral absorption and inhibiting its production in the liver. This hormone has been linked to the regulation of energy metabolism and, more recently, some of its genetic variations have been associated with longevity, dementia, metabolic diseases and cancer.10 Unlike some studies performed on gastric by-pass2 patients, in whom IGF-1 levels significantly decrease after surgery, our outcomes show that IGF-1 levels increase significantly and in positive relation to adiponectin levels in patients who have undergone sleeve gastrectomy 6 months after surgery.11
Adiponectin is an adiposin which plays a protective role in cardiovascular risk as it inhibits inflammation and atherogenesis,12 its blood concentrations relating negatively with C-reactive protein and triglyceride levels and positively with HDL cholesterol levels.13 Significant increases in its values have been demonstrated in studies of obese gastric by-pass patients from the first day following surgery.14 In line with this, we have shown in our study that adiponectin levels, after a drop during the immediate postoperative period, tend to increase, just as HDL levels, and there is a significant decrease in blood levels of triglycerides 6 months and one year after surgery.
A prospective randomised study published by Woelnerhanssen in 2011 demonstrated no significant differences in the results of gastric by-pass and sleeve gastrectomy on the evolution of postoperative values of the parameters connected with glycolipid metabolism such as insulin, glucose, lipids, leptin and adiponectin.15
Therefore, we can conclude that sleeve gastrectomy is a bariatric surgery technique which presents good weight outcomes and cure of comorbidities from the first postoperative months, producing significant changes in the levels of peptides and hormones related with glycolipid metabolism such as glucose, insulin, IGF-1, leptin, adiponectin, triglycerides and HDL cholesterol.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bruna M, Gumbau V, Guaita M, Canelles E, Mulas C, Basés C, et al. Estudio prospectivo de los valores de hormonas y péptidos relacionados con el metabolismo glucolipídico en pacientes obesos mórbidos sometidos a una gastrectomía vertical. Cir Esp. 2014;92:175–181.