The main objective was the description and analysis of suspended surgeries and their causes for suspension at our hospital from the year 2010 to the present. As a secondary objective, we evaluated the effectiveness of a series of measures for improvement.
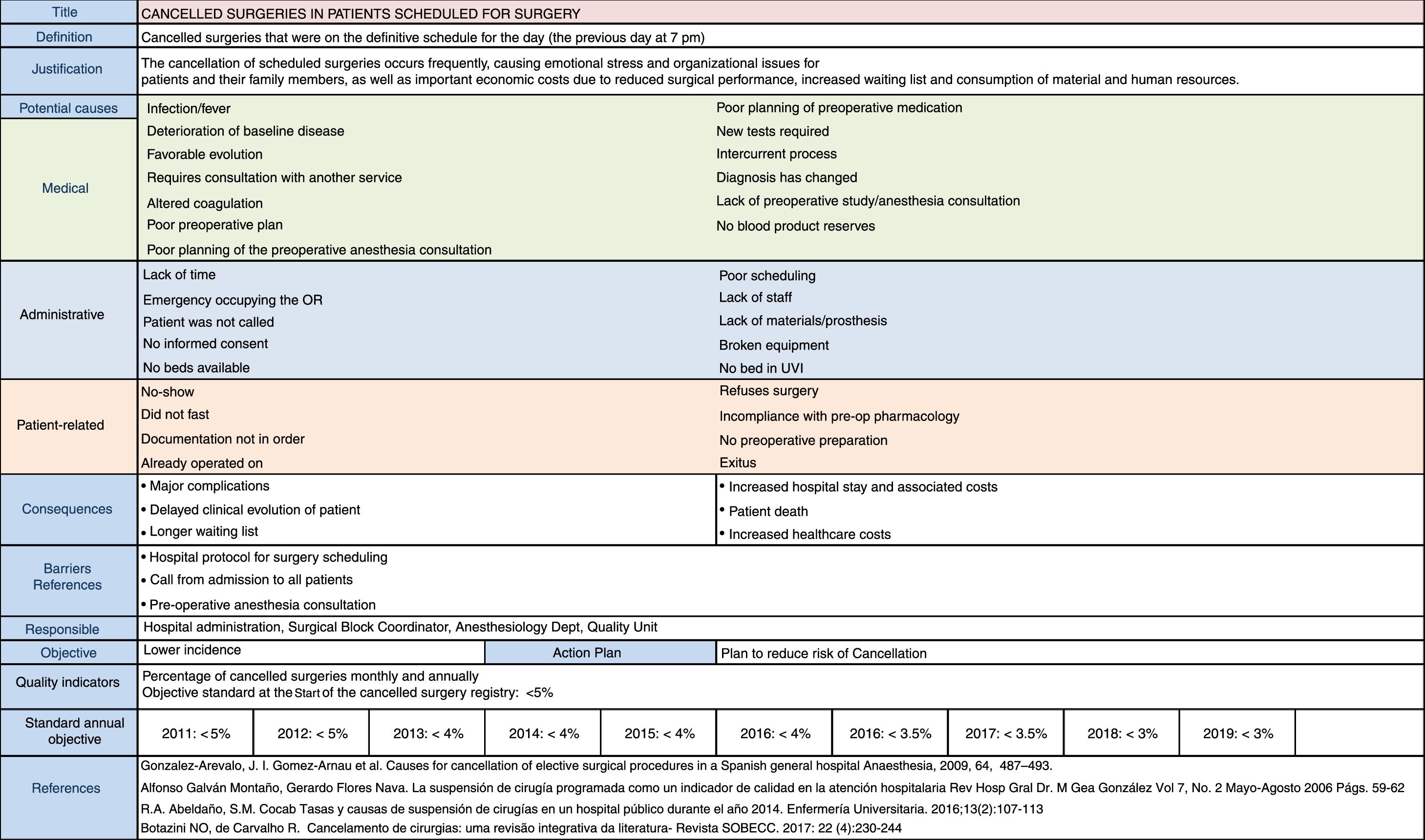
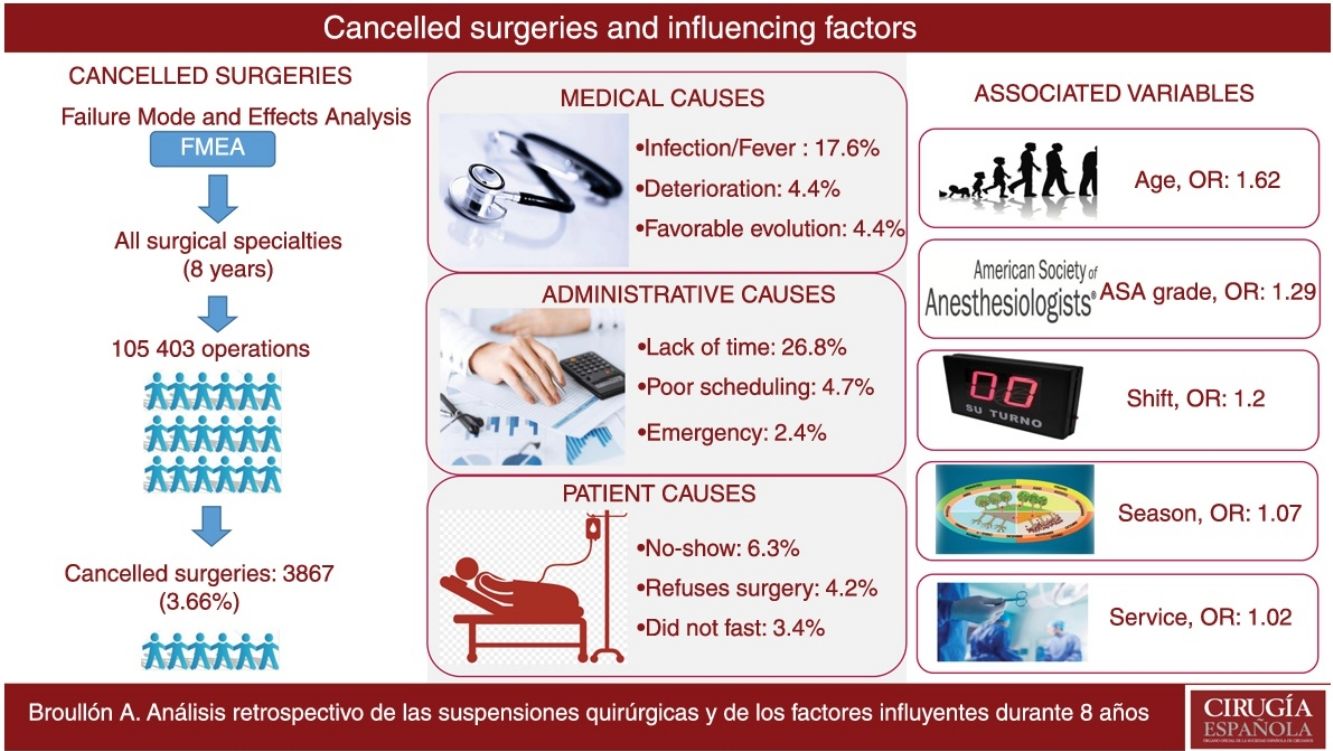
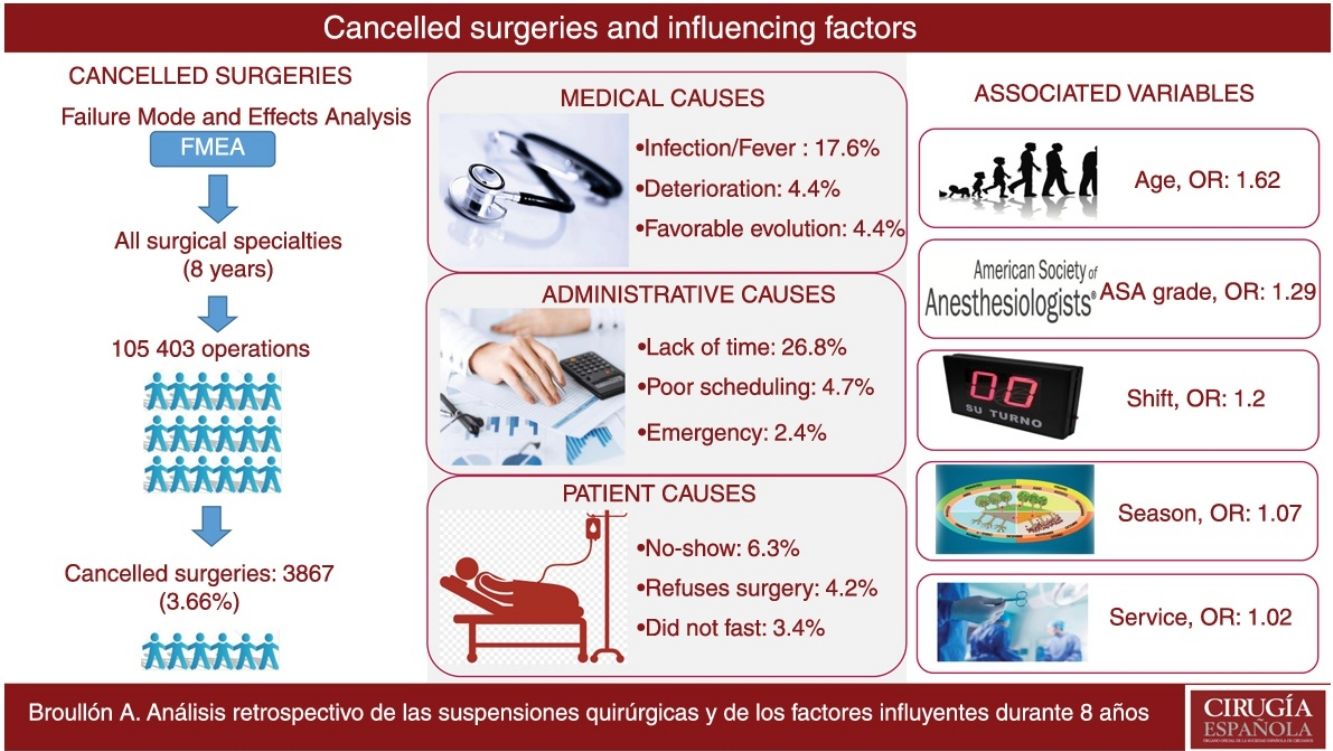
MethodsA retrospective study was conducted to analyze patients who were scheduled to undergo surgery that was finally suspended. A Failure Mode and Effects Analysis (FMEA) was carried out to analyze the causes of the suspensions and their consequences, any existing barriers and possible measures that have been implemented over time. The causes were classified as attributable to the patient, administrative causes and medical causes.
Results105403 surgeries were scheduled, 3867 of which were suspended (3.66%). Factors that influenced the suspensions included: surgical specialty, ASA 4 patients, elderly patients, ambulatory patients and surgeries scheduled during the winter. The most frequent medical cause was infection or fever (17.6%), while the most frequent administrative and patient causes were lack of time (26.8%) and no-show (6.3%), respectively. The avoidable causes were 64.8% versus 35.2% unavoidable causes. In the multivariate analysis, risk factors included age, shift, season and surgical service.
ConclusionsSurgical cancellations have repercussions on the consumption of material and human resources. Any means to reduce their incidence should be our future priority in order improve the quality of care.
El objetivo principal es la descripción y análisis de las suspensiones quirúrgicas y sus causas de nuestro hospital desde el año 2010 hasta la actualidad. Como objetivo secundario evaluamos la efectividad de una serie de medidas de mejora.
MétodosSe realizó un estudio retrospectivo analizando pacientes que estaban programados para ser intervenidos y que finalmente se suspendieron. Se realizó un análisis modal de fallos y efectos (AMFE) para analizar las causas de las suspensiones y sus consecuencias, las barreras existentes y las posibles medidas que se han implantado con el paso del tiempo. Las causas se clasificaron en atribuibles al paciente, causas administrativas y causas médicas.
ResultadosSe programaron 105.403 intervenciones, en las que se originaron 3.867 suspensiones (3,66%). Entre los factores que influyen en las suspensiones describimos la especialidad quirúrgica, los pacientes ASA 4, los pacientes ancianos, los pacientes ambulatorios y los intervenidos durante el invierno. Las causas más frecuentes fueron la infección o fiebre (17,6%) dentro de las causas médicas, la falta de tiempo (26,8%) en cuanto a las administrativas, y la no comparecencia dentro de las causas del paciente (6,3%). Las causas evitables fueron el 64,8% frente al 35,2% de causas inevitables. En el análisis multivariante encontramos como factores de riesgo la edad, el turno, la estación y el servicio quirúrgico.
ConclusionesLas cancelaciones quirúrgicas tienen repercusiones a nivel de consumo de recursos materiales y humanos. Cualquier actuación para intentar reducirlas deberá ser nuestra prioridad futura para disminuir la incidencia de las mismas y mejorar la calidad asistencial.
The cancellation of surgical procedures is a problem that directly impacts the quality of care and, more specifically, related factors (less efficiency, lower degree of patient satisfaction, etc.), creating emotional and organizational turmoil for patients and their families. In addition, human and structural resources are wasted, which increases the costs associated with surgical care. This suggests that suspended or cancelled surgeries should not be considered an inherent problem of the hospital system, but rather an anomalous situation that needs to be controlled to maintain a standard of quality.1
The incidence of cancellations is high and reaches 14% in elective surgeries.2 In this context, we must also consider that these suspension rates vary not only among different hospital sizes and types, but they also depend significantly on the surgical specialty.3 Determining the cancellation rate at each hospital institution should be a priority in order to guarantee patients timely, efficient and high-quality care.4 In addition, it is also necessary to identify the reasons why these cancellations occur in order to take actions to lower their incidence.
After analyzing the different causes for suspended surgery and their incidence, some authors have analyzed the impact of specific measures to reduce cancellation rates. For example, Lee et al. have studied the impact of preoperative phone calls, which have been effective to reduce cancellation rates in pediatric surgery.5 Other authors describe the implementation of preoperative planning and preparation protocols for elective surgery, including measures such as early clinical evaluation of patients, better planning and documentation systems, and greater patient participation in surgery scheduling, which have achieved a significant reduction in the rate of surgery cancellations.6
The implementation of different measures will depend on the individualized analysis of each hospital, as the results cannot usually be extrapolated from hospital to hospital.7 It will also be necessary to analyze long periods of time to demonstrate the sustainability of the results obtained after the changes implemented.8
The objective of this study was to describe and analyze cancelled surgeries and their causes at our hospital from 2010 until today. As a secondary objective, we evaluated the effectiveness of a series of measures for improvement.
MethodsThis is a retrospective observational study analyzing all the reasons for suspension in patients scheduled for surgery at the Hospital Povisa in Vigo between June 2010 and May 2018. The hospital has 550 beds and offers all surgical specialties (except cardiac surgery), serving a healthcare region of some 150000 patients, including private care. This study has been accepted by the Research and Ethics Committee of Galicia, Registration Code: 2018/332.
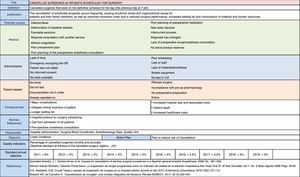
To assess the problem of suspended surgical procedures, during the first semester of 2010 a failure mode and effects analysis (FMEA) was conducted (Fig. 1) in order to analyze the causes of cancellations and their consequences, any existing barriers and possible measures that have been implemented over time.
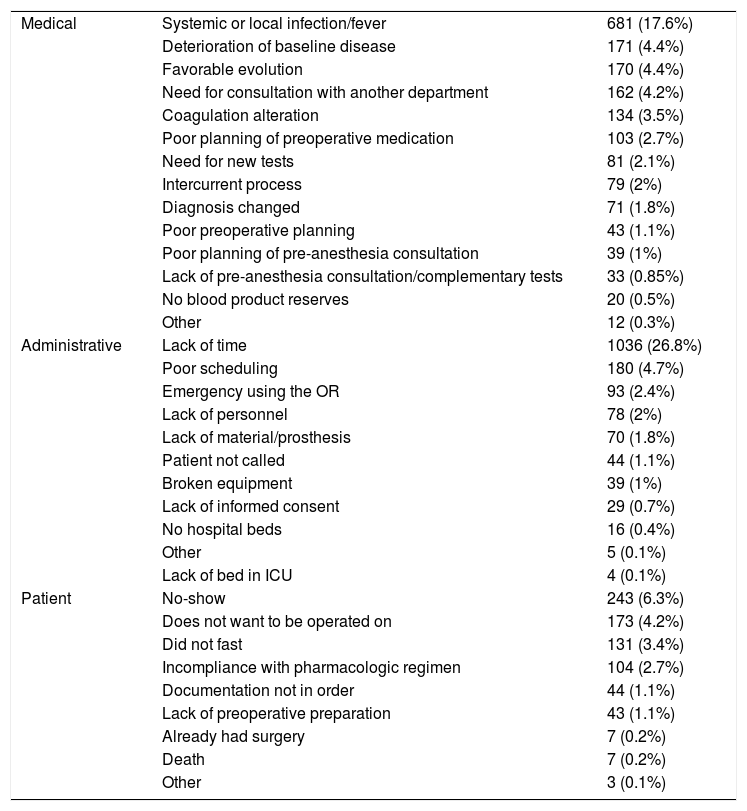
Inclusion criteria. The study included all the patients who were going to be operated on in both major ambulatory surgery (MAS) and traditional admitted surgery regimens, and who were already on the definitive surgery schedule (at our hospital, the schedule is published the previous day at 7pm) but did not undergo surgery due to different reasons. These were classified as patient-related or as a result of either administrative or medical causes (Table 1).
Classification of the Causes for Suspension.
| Medical | Systemic or local infection/fever | 681 (17.6%) |
| Deterioration of baseline disease | 171 (4.4%) | |
| Favorable evolution | 170 (4.4%) | |
| Need for consultation with another department | 162 (4.2%) | |
| Coagulation alteration | 134 (3.5%) | |
| Poor planning of preoperative medication | 103 (2.7%) | |
| Need for new tests | 81 (2.1%) | |
| Intercurrent process | 79 (2%) | |
| Diagnosis changed | 71 (1.8%) | |
| Poor preoperative planning | 43 (1.1%) | |
| Poor planning of pre-anesthesia consultation | 39 (1%) | |
| Lack of pre-anesthesia consultation/complementary tests | 33 (0.85%) | |
| No blood product reserves | 20 (0.5%) | |
| Other | 12 (0.3%) | |
| Administrative | Lack of time | 1036 (26.8%) |
| Poor scheduling | 180 (4.7%) | |
| Emergency using the OR | 93 (2.4%) | |
| Lack of personnel | 78 (2%) | |
| Lack of material/prosthesis | 70 (1.8%) | |
| Patient not called | 44 (1.1%) | |
| Broken equipment | 39 (1%) | |
| Lack of informed consent | 29 (0.7%) | |
| No hospital beds | 16 (0.4%) | |
| Other | 5 (0.1%) | |
| Lack of bed in ICU | 4 (0.1%) | |
| Patient | No-show | 243 (6.3%) |
| Does not want to be operated on | 173 (4.2%) | |
| Did not fast | 131 (3.4%) | |
| Incompliance with pharmacologic regimen | 104 (2.7%) | |
| Documentation not in order | 44 (1.1%) | |
| Lack of preoperative preparation | 43 (1.1%) | |
| Already had surgery | 7 (0.2%) | |
| Death | 7 (0.2%) | |
| Other | 3 (0.1%) |
In order to analyze the possible preventability of the causes, we have divided these into 2 groups: avoidable and unavoidable. Avoidable causes were defined as those that could have been detected before the day of surgery. Unavoidable causes could not have been previously identified and therefore could not be prevented. We have also determined that there was an important group of avoidable causes that ceased to be avoidable when they occurred without sufficient time to correct this issue or to schedule another patient. Therefore, and to further define the classification, the anesthesiologist was responsible for determining whether the cause was either avoidable or unavoidable for each of the cancelled surgeries, based on his/her own criteria. To minimize variability, specific training was given about the precise definitions of the causes for cancellation.
In the analysis of the factors, we have included patient age (younger than 45, 45–75, and over 75), ASA grade, season of the year, operating shift (morning or afternoon), the administrative regimen (admitted or ambulatory) and the surgery department.
Exclusion criteria. Patients were excluded when their surgery was cancelled after the anesthesia procedure had initiated and did not undergo surgery due to clinical complications after induction (allergic reactions, impossible airway, technical difficulties, etc.).
To register the cancelled surgeries for subsequent study, a specific software program was developed for use within the Anesthesia Department system (AnesReaDol®), in which all surgical cancellations were recorded. This software established a monthly monitoring indicator and another for the annual monitoring of cancelled patients. The software recorded all suspended surgeries, their preventability, classification of the causes, explanation of the cancellation and parameters such as who cancelled, which surgical specialty was involved and the place of the cancellation. A report of the event was saved in the electronic patient medical file.
Statistical AnalysisThe qualitative variables are expressed in frequencies followed by the percentage in parentheses. In the comparison of proportions among qualitative variables, the Chi-squared test with Yates correction or Fisher's exact test was used when indicated.
The quantitative variables are expressed as median±interquartile range (IQR) because the distribution is not normal (Kolmogorov–Smirnov test). The comparison of quantitative variables with non-normal distribution was done with a nonparametric test: the Mann–Whitney U for 2 groups.
The multivariate analysis for the study of risk factors associated with cancelled surgeries was performed by multivariate logistic regression in stages.
A P value <.05 was considered significant.
The statistical analysis was carried out using SPSS v.15 software for Windows (SPSS Inc., Chicago, IL, USA.) or R v.3.0.1 (R Development Core Team, 2013, Vienna, Austria).
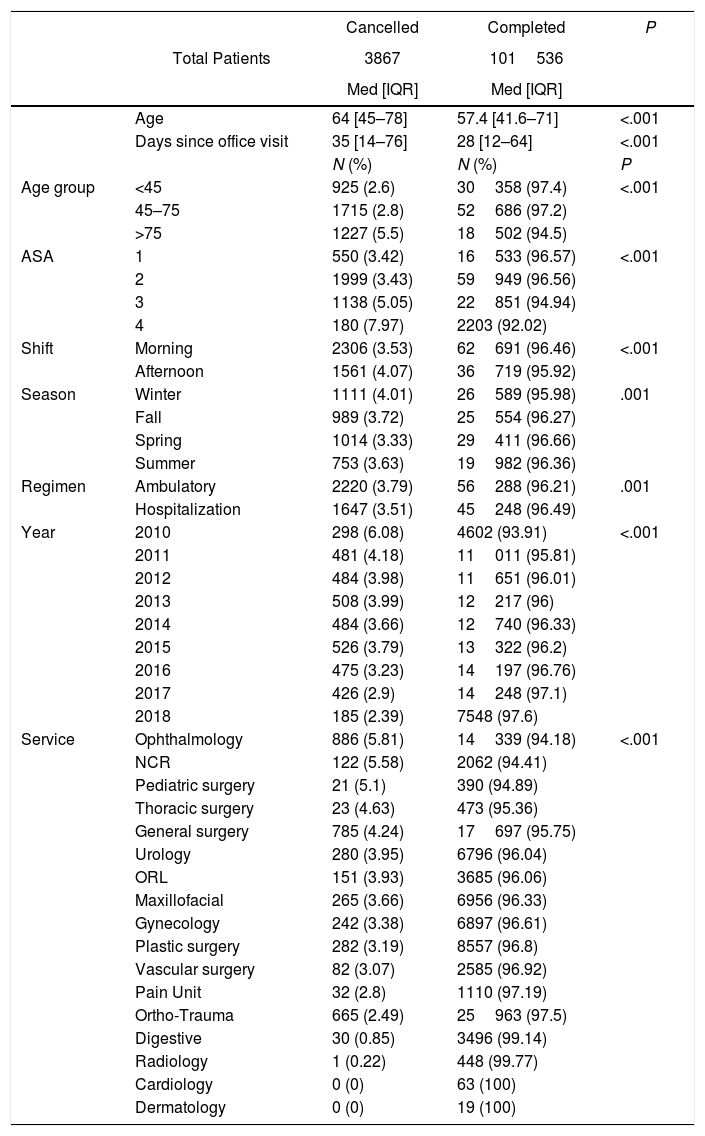
ResultsDuring the 8 years of the study, 105403 surgeries were scheduled, 3867 of which were cancelled, resulting in an overall incidence of 3.66% (Table 2).
Variables Related With the Series of Patients With Completed or Cancelled Surgeries.
| Cancelled | Completed | P | ||
|---|---|---|---|---|
| Total Patients | 3867 | 101536 | ||
| Med [IQR] | Med [IQR] | |||
| Age | 64 [45–78] | 57.4 [41.6–71] | <.001 | |
| Days since office visit | 35 [14–76] | 28 [12–64] | <.001 | |
| N (%) | N (%) | P | ||
| Age group | <45 | 925 (2.6) | 30358 (97.4) | <.001 |
| 45–75 | 1715 (2.8) | 52686 (97.2) | ||
| >75 | 1227 (5.5) | 18502 (94.5) | ||
| ASA | 1 | 550 (3.42) | 16533 (96.57) | <.001 |
| 2 | 1999 (3.43) | 59949 (96.56) | ||
| 3 | 1138 (5.05) | 22851 (94.94) | ||
| 4 | 180 (7.97) | 2203 (92.02) | ||
| Shift | Morning | 2306 (3.53) | 62691 (96.46) | <.001 |
| Afternoon | 1561 (4.07) | 36719 (95.92) | ||
| Season | Winter | 1111 (4.01) | 26589 (95.98) | .001 |
| Fall | 989 (3.72) | 25554 (96.27) | ||
| Spring | 1014 (3.33) | 29411 (96.66) | ||
| Summer | 753 (3.63) | 19982 (96.36) | ||
| Regimen | Ambulatory | 2220 (3.79) | 56288 (96.21) | .001 |
| Hospitalization | 1647 (3.51) | 45248 (96.49) | ||
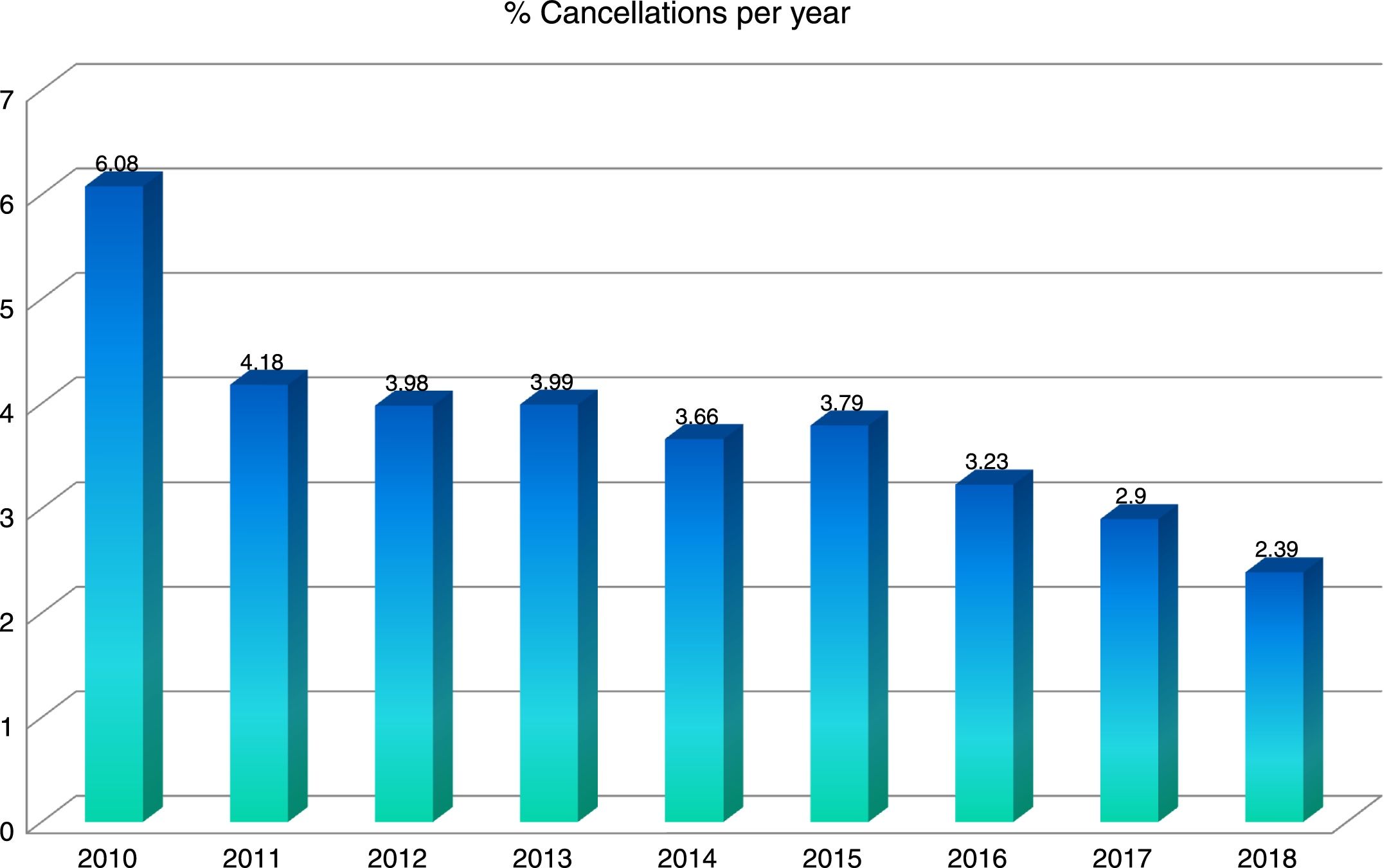
| Year | 2010 | 298 (6.08) | 4602 (93.91) | <.001 |
| 2011 | 481 (4.18) | 11011 (95.81) | ||
| 2012 | 484 (3.98) | 11651 (96.01) | ||
| 2013 | 508 (3.99) | 12217 (96) | ||
| 2014 | 484 (3.66) | 12740 (96.33) | ||
| 2015 | 526 (3.79) | 13322 (96.2) | ||
| 2016 | 475 (3.23) | 14197 (96.76) | ||
| 2017 | 426 (2.9) | 14248 (97.1) | ||
| 2018 | 185 (2.39) | 7548 (97.6) | ||
| Service | Ophthalmology | 886 (5.81) | 14339 (94.18) | <.001 |
| NCR | 122 (5.58) | 2062 (94.41) | ||
| Pediatric surgery | 21 (5.1) | 390 (94.89) | ||
| Thoracic surgery | 23 (4.63) | 473 (95.36) | ||
| General surgery | 785 (4.24) | 17697 (95.75) | ||
| Urology | 280 (3.95) | 6796 (96.04) | ||
| ORL | 151 (3.93) | 3685 (96.06) | ||
| Maxillofacial | 265 (3.66) | 6956 (96.33) | ||
| Gynecology | 242 (3.38) | 6897 (96.61) | ||
| Plastic surgery | 282 (3.19) | 8557 (96.8) | ||
| Vascular surgery | 82 (3.07) | 2585 (96.92) | ||
| Pain Unit | 32 (2.8) | 1110 (97.19) | ||
| Ortho-Trauma | 665 (2.49) | 25963 (97.5) | ||
| Digestive | 30 (0.85) | 3496 (99.14) | ||
| Radiology | 1 (0.22) | 448 (99.77) | ||
| Cardiology | 0 (0) | 63 (100) | ||
| Dermatology | 0 (0) | 19 (100) |
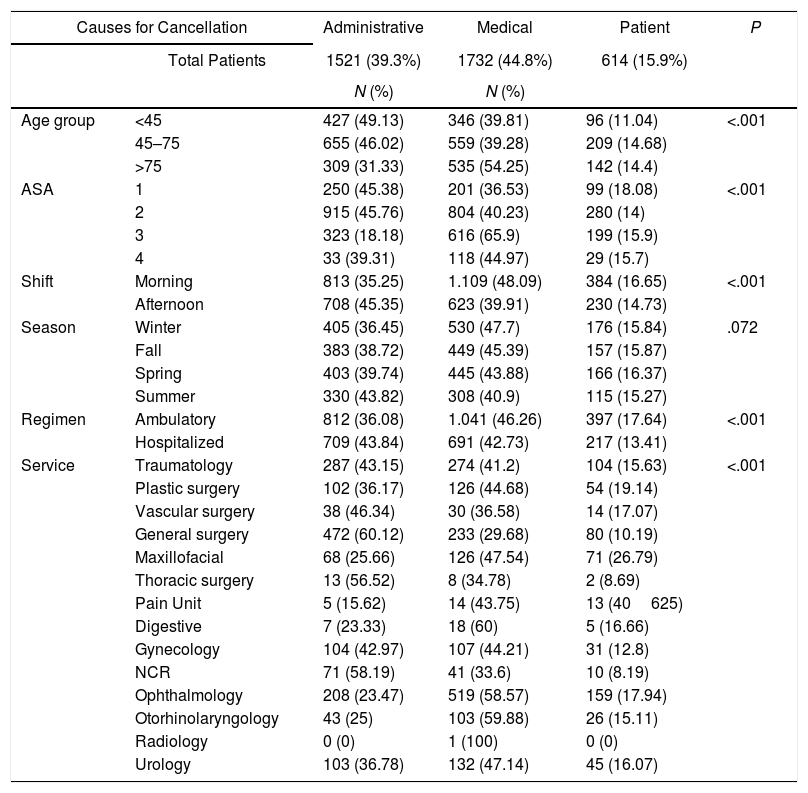
Table 3 demonstrates the influence of different factors on cancellations. Statistically significant differences were found according to the surgical service; those that registered the highest cancellation rates were Ophthalmology (5.81%), Neurosurgery (5.58%) and General Surgery (4.24%).
Influence of Different Factors on the Causes for Cancellation.
| Causes for Cancellation | Administrative | Medical | Patient | P | |
|---|---|---|---|---|---|
| Total Patients | 1521 (39.3%) | 1732 (44.8%) | 614 (15.9%) | ||
| N (%) | N (%) | ||||
| Age group | <45 | 427 (49.13) | 346 (39.81) | 96 (11.04) | <.001 |
| 45–75 | 655 (46.02) | 559 (39.28) | 209 (14.68) | ||
| >75 | 309 (31.33) | 535 (54.25) | 142 (14.4) | ||
| ASA | 1 | 250 (45.38) | 201 (36.53) | 99 (18.08) | <.001 |
| 2 | 915 (45.76) | 804 (40.23) | 280 (14) | ||
| 3 | 323 (18.18) | 616 (65.9) | 199 (15.9) | ||
| 4 | 33 (39.31) | 118 (44.97) | 29 (15.7) | ||
| Shift | Morning | 813 (35.25) | 1.109 (48.09) | 384 (16.65) | <.001 |
| Afternoon | 708 (45.35) | 623 (39.91) | 230 (14.73) | ||
| Season | Winter | 405 (36.45) | 530 (47.7) | 176 (15.84) | .072 |
| Fall | 383 (38.72) | 449 (45.39) | 157 (15.87) | ||
| Spring | 403 (39.74) | 445 (43.88) | 166 (16.37) | ||
| Summer | 330 (43.82) | 308 (40.9) | 115 (15.27) | ||
| Regimen | Ambulatory | 812 (36.08) | 1.041 (46.26) | 397 (17.64) | <.001 |
| Hospitalized | 709 (43.84) | 691 (42.73) | 217 (13.41) | ||
| Service | Traumatology | 287 (43.15) | 274 (41.2) | 104 (15.63) | <.001 |
| Plastic surgery | 102 (36.17) | 126 (44.68) | 54 (19.14) | ||
| Vascular surgery | 38 (46.34) | 30 (36.58) | 14 (17.07) | ||
| General surgery | 472 (60.12) | 233 (29.68) | 80 (10.19) | ||
| Maxillofacial | 68 (25.66) | 126 (47.54) | 71 (26.79) | ||
| Thoracic surgery | 13 (56.52) | 8 (34.78) | 2 (8.69) | ||
| Pain Unit | 5 (15.62) | 14 (43.75) | 13 (40625) | ||
| Digestive | 7 (23.33) | 18 (60) | 5 (16.66) | ||
| Gynecology | 104 (42.97) | 107 (44.21) | 31 (12.8) | ||
| NCR | 71 (58.19) | 41 (33.6) | 10 (8.19) | ||
| Ophthalmology | 208 (23.47) | 519 (58.57) | 159 (17.94) | ||
| Otorhinolaryngology | 43 (25) | 103 (59.88) | 26 (15.11) | ||
| Radiology | 0 (0) | 1 (100) | 0 (0) | ||
| Urology | 103 (36.78) | 132 (47.14) | 45 (16.07) | ||
The median age of the patients studied was 64 years (45–78) in the group of patients with suspended surgery versus 57.4 (41.6–71) in the group of patients who underwent surgery (P<.001).
The days that had elapsed between the pre-anesthesia consultation and the day of scheduled surgery were 35 (14–76) in the group of surgical suspensions versus 28 (12–64) in the group of patients with completed surgeries.
Regarding age, the group that had a higher rate of cancellations (5.5%) was group 3 (elderly patients) (P<.001). According to the ASA classification, ASA 4 patients had the most cancellations (7.97%), (P<.001).
As for the variation between the seasons of the year, the lowest cancellation rate was observed in the spring (3.33%) and the highest in the winter (4.01%) (P=.001).
In terms of the MAS regimen or elective surgery with hospitalization, statistically significant differences were also observed, and MAS had the highest suspension rate (3.79%) compared to admitted patients (3.51%) (P=.001).
When recording the causes for cancellation, there were classified into 3 large groups: medical causes, administrative causes and patient-related causes.
Table 1 shows the causes for cancellation. Within each group, the most frequent causes were, respectively, infection or fever (17.6%) among the medical causes, lack of time (26.8%) among the administrative causes, and patient no-show (6.3%) among the patient-related causes. In turn, the causes were classified according to their possible prevention into 2 groups: avoidable causes (64.8%), and unavoidable causes (35.2%).
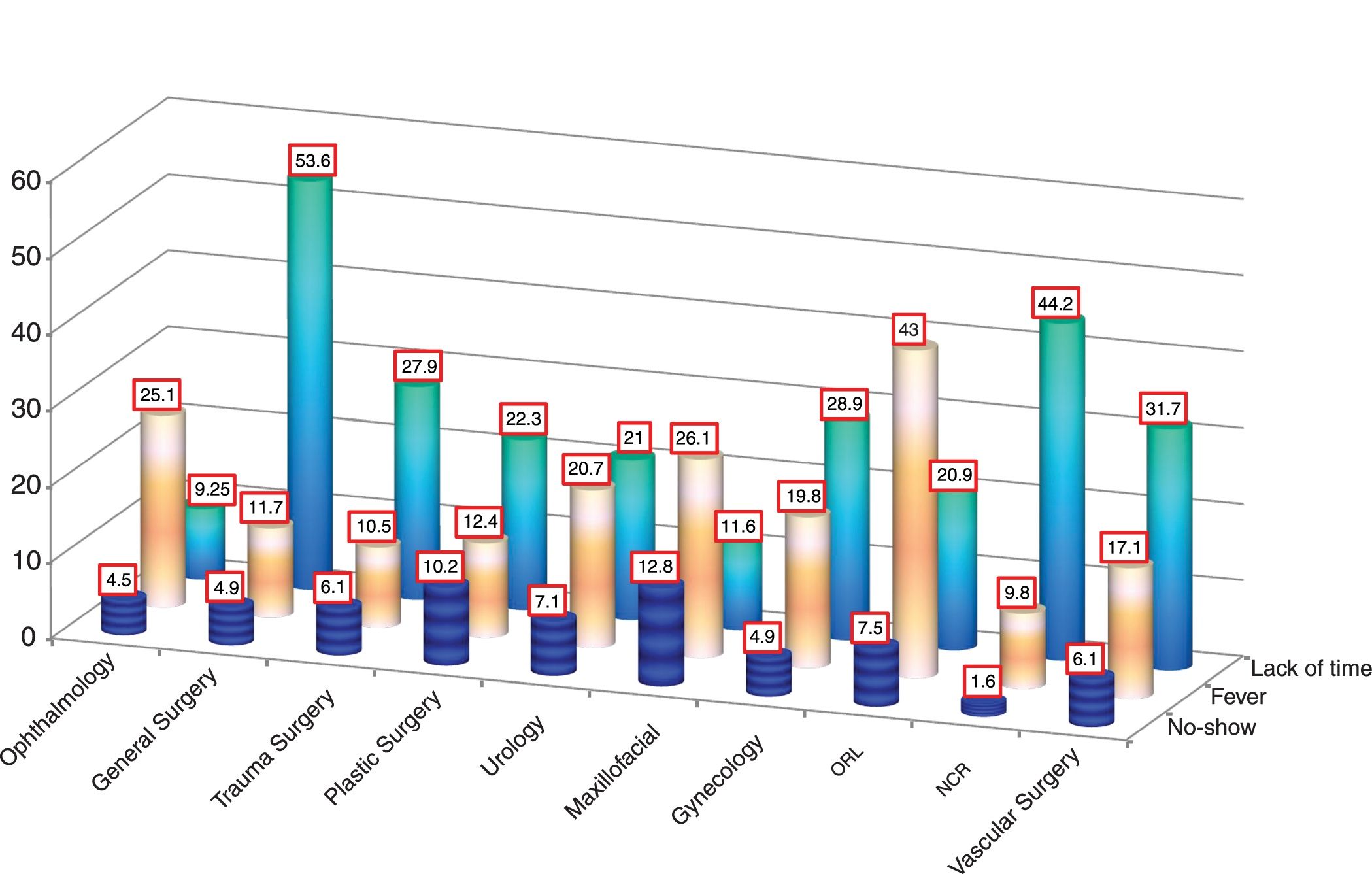
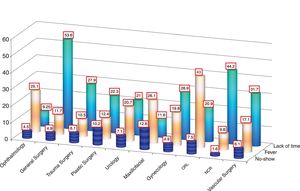
Infection or fever was the cause of most cancellations of the Oral and Maxillofacial Surgery (26.1%), Otolaryngology (43%) and Ophthalmology (25.1%) services. Lack of time, however, affected more specialties with greater use of surgical time, such as General Surgery (53.6%) and Neurosurgery (44.2%) (Fig. 2). As for patient absence, no statistically significant differences were found in correlation with the surgical service.
With the multivariate analysis, we found several risk factors associated with cancelled surgeries: age group (OR 1.62; IQR [1.4–1.88], P<.001); ASA (OR 1.29; IQR [1.19–1.4], P<.001); operating room shift (OR 1.20; IQR [1.1–1.32], P<.001); season (OR 1.073; IQR [1.032–1.11], P<.001); surgical service (OR 1.02; IQR [1.01–1.03], P<.001); and the year (OR 0.92; IQR [0.9–0.94], P<.001).
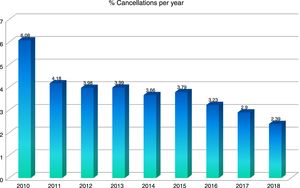
Regarding the annual follow-up indicator for cancellations, Table 2 and Fig. 3 show how these have been decreasing over the years after the progressive implementation of measures specifically described in the FMEA (Fig. 1).
DiscussionThe overall cancellation rate in our study was 3.66%, a figure that can be considered acceptable compared with other published articles, although we must admit there are limitations for comparing our results with other hospitals that have different definitions, characteristics and organization.
A recent study9 reviewed 61 articles with regard to cancelled surgeries. The authors found great variability in the results, with cancellation rates ranging from 0.48% to 38%.
Other authors10–12 have reported that there is no agreement on what the “acceptable” rate of cancellations should be, as these may vary over a very wide range and depend on the references consulted. According to the proposed standards and the indicator established by Galván-Montaño and Flores-Nava,1 a “good” result should be below 3.1%. Even so, we found published results far above this objective: 7.6%,9 16.1%13 and 37.28%.14 In our opinion, it is important to differentiate between potentially avoidable causes and those that are not, as we should focus our improvement efforts on avoidable causes. Some authors have also made this distinction by distributing the causes of cancellation by their possibility of prevention,15 which, according to Macarthur et al., could reach 50%.16 In our study, avoidable causes reached 64.8% of the total causes for cancellation. If we omit the unavoidable causes (35.2% of the total), we would obtain a final cancellation rate of 2.38%, which is considered a “good” standard, as defined in the article by Galván-Montaño and Flores-Nava, mentioned above.1
Potentially preventable causes are easy to detect if they appear early enough. However, if they appear the night before surgery, for example, the cancellation would be unavoidable because there would be no time to schedule another patient. The corrective measures implemented (reflected in the FMEA [Fig. 1]) and the training and awareness of staff have led to the progressive decrease in the annual rate of cancelled surgeries (Fig. 3).
By carefully analyzing the results obtained, it is easy to explain why the suspension rate was higher in older and ASA 4 patients. Their frailty and comorbidities make them more likely to experience a deterioration of their baseline disease, requiring new tests or inter-consultation with another service to optimize their condition before surgery.
The higher cancellation rate in winter was likely related to the higher incidence of respiratory and infectious processes, which are more common in the cold months. In this period of time, MAS had a higher suspension rate than elective surgery with hospital admission (3.79% vs 3.51%). These results are similar to reports in the literature for ambulatory patients (4.1%),15 although lower than the results published at our hospital in sedations for digestive endoscopy during the same period (more than 6% per year).17
As for the hospital shift, at our hospital there was a higher rate of cancellations during the afternoon shift (4.07% compared to 3.53% during the morning shift). Other reports in the literature show variability, but at certain hospitals this was also true.18 However, at other hospitals, cancellations occurred mainly in the morning shift,19,20 and this is explained by the variability that exists among hospitals for surgery scheduling and individual strategies.
In the study by Gonzalez-Arevalo et al.10 in Spain, 20% of patients were no-shows and 18% of surgeries were suspended due to infectious processes and fever. However, in other studies in our setting, the cause of ‘intercurrent disease, infection and fever’ was slightly higher, at around 25.7%.15
The lack of surgical time is also very variable, reported to be around 27.2% in the study by Abeldaño and Coca12 and reaching higher figures of up to 63% in other studies.21
In our study, patient absenteeism was the cause in 6.3% of the total number of cancellations, similar to other studies,22 but it reached figures of up to 70% in other published articles.17,23
The lack of time was evident above all in departments that try to optimize scheduling to achieve better performance of the surgical block.24 This objective is necessary in terms of efficiency, although occasionally the unexpected prolongation of a scheduled surgery makes it necessary to cancel and reprogram the surgeries of other patients, which has been associated with greater patient dissatisfaction.25
It has already been demonstrated that preoperative evaluation is extremely important to reduce the cancellation rate of scheduled surgeries.2,26 We analyzed the time transpired between the pre-operative anesthesia consultation and surgery and found that this time is associated with cancelled surgeries (longer times in cancelled surgeries versus completed surgeries, P<.001).
The most frequent cause of cancelled surgery at our hospital was lack of time. To optimize scheduling, it is important to involve all staff due to the importance of this issue.1,12
Regarding patient absenteeism, possible root causes may include an inconvenient date for surgery, forgetfulness about appointments, and fear or doubt prior to surgery.23
The percentage of cancellations per year has been progressively decreasing, and we feel that this is related to the improvement measures that have been implemented. At our hospital, we have proposed the implementation of several measures specified in the FMEA (Fig. 1), with annual re-evaluation, which we consider the reason for the decrease in surgical suspensions that have occurred over the years.
In some articles, a preoperative phone call is proposed as a tool to reduce the number of cancellations, as there has been evidence that the use of generic lists for telephone calls reduced surgical cancellations by up to 53%,27 although other authors recommend the use of an individualized list for every situation.28
Although our study has limitations when extrapolating the results to other hospitals due to differences in structure, population, personnel and administrative services,7 we believe that the methodology used could be applied at other hospitals and adapted to the established organization.
In conclusion, our study shows a low rate of surgical cancellations and a reduction in these cancellations over time based on the introduction of steps for improvement.
FundingThis research study has received no specific funding from public, private or non-profit organizations.
AuthorshipAndrea Broullón Dobarro: design, review of causes, FMEA, article composition, final correction.
Rafael Cabadas Avión: design, software development, review of causes, FMEA, article composition, final correction.
María Sonsoles Leal Ruiloba: design, review of causes, article composition, final correction.
Ana Vázquez Lima: design, review of causes, article composition, final correction.
María Ojea Cendón: design, review of causes, article composition, final correction.
Noelia Fernández García: design, review of causes, article composition, final correction.
Paula Nespereira García: design, review of causes, article composition, final correction.
Antonio Climent Aira: design, review of causes, article composition, final correction.
Conflict of InterestsThe authors have no conflict of interests to declare in association with this article.
Please cite this article as: Broullón Dobarro A, Cabadas Avión R, Leal Ruiloba MS, Vázquez Lima A, Ojea Cendón M, Fernández García N, et al. Análisis retrospectivo de las suspensiones quirúrgicas y de los factores influyentes durante 8 años. Cir Esp. 2019;97:213–221.