The rapid spread of SARS-CoV-2 infection has led to a radical reorganization of healthcare resources. Surgical Departments need to adapt to this change.
Patients and methodsWe performed a prospective descriptive observational study of the incidence of COVID-19 in patients and surgeons of a General Surgical Department in a high prevalence area, between the 1 st and 31 st of March 2020.
ResultsPatients: The incidence of SARS-CoV-2 infection in elective surgery patients was 7% (mean age 59.5 years). All survived. Of 36 patients who underwent emergency surgery, two of them were SARS-CoV-2 positive and one was clinically highly suspicious of COVID-19 (11.1%). All three patients died of respiratory failure (mean age 81 years). Surgeons: There were a total of 12 confirmed SARS-CoV-2+ cases among the surgical department staff (24.4%) (8 out of 34 consultants and 4 out of 15 residents). Healthcare activity: The average number of daily emergency surgical interventions declined from 3.6 in February to 1.16 in March. 42% of the patients who underwent emergency surgery had peritonitis upon presentation.
ConclusionsThe fast pace of COVID-19 pandemia, should alert surgical departments of the need of adopting early measures to ensure the safety of patients and staff.
La rápida expansión de la infección por SARS-CoV-2 ha supuesto una radical reorganización de los recursos sanitarios y la exposición de profesionales al contagio. Los servicios de Cirugía General y del Aparato Digestivo también necesitan adaptarse a este cambio.
Pacientes y métodosSe realiza un estudio observacional descriptivo prospectivo de los casos de COVID-19 en pacientes y cirujanos de un Servicio de Cirugía General en un área de alta incidencia de infección entre el 1 y el 31 de marzo de 2020.
ResultadosPacientes: La incidencia de infección por SARS-CoV-2 en los pacientes programados con hospitalización en el postoperatorio inmediato fue del 7%. Su edad media fue de 59,5 años y todos evolucionaron satisfactoriamente en planta. De 36 pacientes intervenidos de urgencia, dos fueron SARS-CoV-2+ y uno altamente sospechoso de COVID-19 (11,1%). Los tres pacientes fallecieron por insuficiencia respiratoria, su edad media era de 81 años. Cirujanos: Hubo un total de 12 casos SARS-CoV-2 + confirmados (24,4%) (8 de 34 adjuntos y 4 de 15 residentes). Actividad asistencial: El número medio de intervenciones quirúrgicas urgentes diarias bajó de 3,6 en febrero a 1,16 en el mes de marzo. El 42% de los pacientes intervenidos a partir de la entrada en vigor de las primeras medidas de aislamiento a nivel regional, presentaban cuadros evolucionados.
ConclusionesEl aumento de casos en la población general de COVID-19 debe alertar a los Servicios de Cirugía General de la necesidad de tomar de medidas de forma precoz que garanticen la seguridad de los pacientes y de los cirujanos.
Since the first cases of severe pneumonia due to SARS-CoV-2 were reported in Wuhan, China in December 2019, infection with this coronavirus has been spreading throughout the world and was declared a pandemic by the WHO on March 11, 2020.1
In a short time, hospitals have needed to reorganize healthcare resources to care for patients with COVID-19, especially in the emergency departments and the ICU. Hospitals in areas with a high incidence of cases have had to adapt quickly to this situation and organize COVID-19 patient treatment according to daily necessities.2,3
In addition to increasing the number of hospital beds and ICUs, it has been necessary to adapt the work activities of other hospital departments, such as General Surgery and their staff, to the common goal of treating these patients.
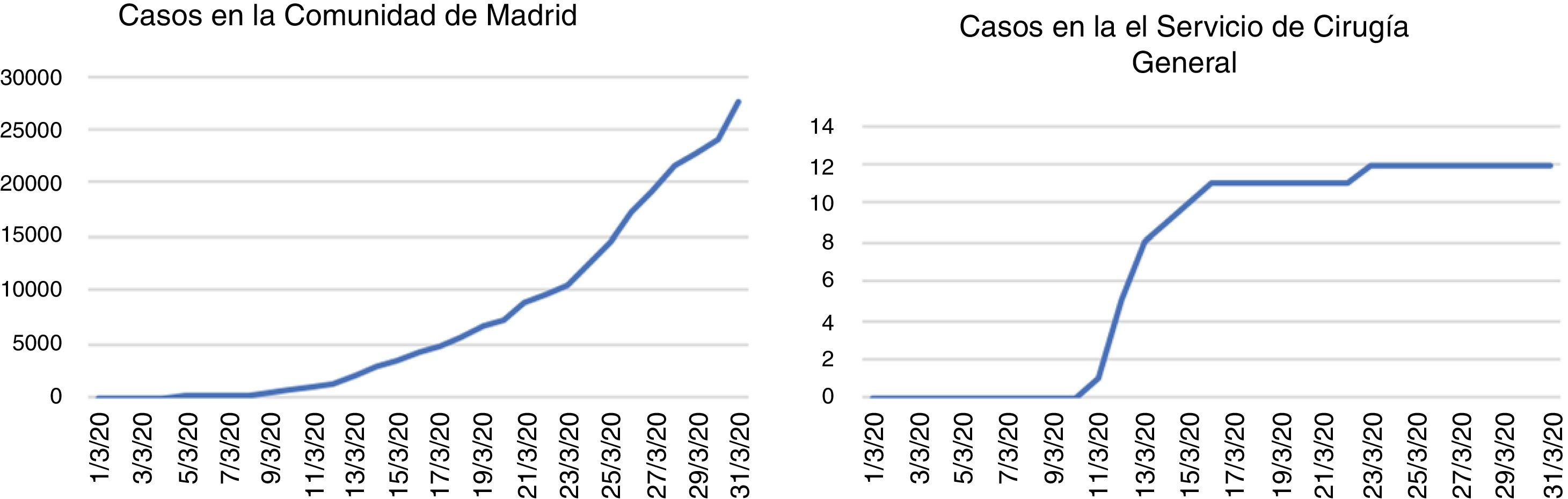
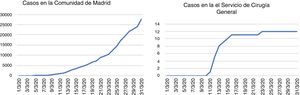
SARS-CoV-2 infection among the population of the Community of Madrid developed rapidly after the detection of the first case imported from Italy in late February 2020. Despite the measures that were gradually adopted, both regionally as well as nationally, the number of cases continues to increase to this day.
The first case of SARS-CoV-2 infection was detected in Madrid on February 24, 2020. The patient was a young male who had returned from a trip through northern Italy. After March 8th, the growth of COVID-19 cases increased sharply, and on March 9th the Government of the Community of Madrid announced the first measures to prevent the propagation of the virus among the population: cancellation of classes at all educational levels for 2 weeks, as well as the possibility of cancellation or delay of medical consultations, diagnostic testing and non-essential surgeries.4,5
Parallel with the progressive increase in cases in the general population and the increase in consultations in the Emergency Department due to respiratory conditions and symptoms compatible with COVID-19, we also began to see patients in the General Surgery Department with suspected SARS-CoV-2 infection, and the first cases of infection were detected among surgeons of the department.
This study provides a descriptive analysis of the impact that the SARS-CoV-2 pandemic has had in a General and Gastrointestinal Surgery Department at a tertiary hospital in Madrid (Spain) during the first weeks of spread of the disease among its population. The objective is to analyze the incidence of cases of patients and professionals with COVID-19 in a General Surgery Department as the incidence increases among the general population of their regional care area, as well as to study the impact of infection on the service’s healthcare activity and to evaluate the effect of the measures adopted.
MethodsStudy setting. We prospectively included in this study patients who had been treated by the General Surgery Department at Hospital Universitario La Paz from March 1 to 31 who presented symptoms compatible with COVID-19, as well as cases with symptoms compatible with COVID-19 among attending surgeons and residents of the service during the same period of time. Ours is a SERMAS (Madrid Health Service) public hospital with 1358 beds, and the General and Gastrointestinal Surgery Department has 34 assistant surgeons and 15 residents.
Definition of cases. The presence of at least one of the following symptoms was considered compatible with COVID-19 infection: cough, dyspnea, sore throat, chest pain, anosmia, dysgeusia or the onset of fever.1 For the confirmation of suspicious cases, the RT-PCR technique was used (according to the methodology available in the Hospital’s microbiology laboratory) performed with a sample obtained with a nasopharyngeal swab. Patients and physicians with a negative RT-PCR who had maintained symptoms compatible with COVID-19 were re-tested by RT-PCR. Radiological signs that we considered compatible with COVID-19 included: the appearance of peripheral ground glass opacities, diffuse alveolar pattern, bilateral patchy shadows, cobblestone pattern and organizing pneumonia.6
ResultsImpact of the SARS-CoV-2 Pandemic on Surgical Patients Treated by the General Surgery Department at the Hospital Universitario La PazFrom March 1 to March 31, 2020, 189 patients underwent surgery in the General and Gastrointestinal Surgery Department: 100 were scheduled surgeries with hospitalization, 36 urgent surgeries, and 53 major outpatient surgery at Hospital Carlos III.
From March 1 to 10, the service maintained its usual healthcare activity. As of March 11, surgical procedures for benign pathologies were suspended. Starting March 16, patients with oncological pathology were selected, prioritizing those with risk of imminent complications.
Out of the 153 patients who underwent scheduled surgery from March 1 to 31, 2020, 7 presented symptoms compatible with COVID-19, and RT-PCR confirmed SARS-CoV-2 infection (4.57%) in the immediate postoperative period. In the group of patients who underwent surgery with hospitalization, the percentage of patients who developed COVID-19 was 7%.
During the postoperative period of the 36 patients who underwent urgent surgery, 2 were SARS-CoV-2+, confirmed by RT-PCR, and one had symptoms highly suggestive of COVID-19 (11.1%). All 3 patients died of respiratory failure.
The mean age of the SARS-CoV-2-positive patients who underwent scheduled surgery was 59.5 years, and the mean age of patients who underwent urgent surgery was 81 years. In terms of sex, 42.8% of all patients with infection were male. The most frequent comorbidities among these patients were obesity, DM and COPD (present in 3 patients), followed by HTN and heart failure (2 patients).
We should also mention a 72-year-old patient who underwent urgent surgery for perforation of the small intestine, followed by a slow recovery due to intra-abdominal abscesses and 23 days of hospitalization, who later presented respiratory symptoms 8 days after hospital discharge. Pneumonia due to COVID-19 was confirmed by CT scan and RT-PCR in 2 nasopharyngeal samples.
Impact on Patients in Scheduled SurgeryOut of the 153 patients who underwent scheduled surgery, 7 presented COVID-19 with confirmation by PCR (4.57%).
From March 1 to 31, 13 patients who had undergone scheduled surgery with hospitalization presented respiratory symptoms and fever between postoperative days 2 and 7. All underwent RT-PCR testing and began wearing surgical masks from the moment of clinical suspicion. In 6 cases, SARS-CoV-2 infection was confirmed during hospitalization (in 2 cases, 2 and 3 samples were taken to confirm infection due to high clinical suspicion and first and/or second negative RT-PCR). The procedures that had been performed were 2 total gastrectomies for gastric adenocarcinoma, 3 Hartmann procedures (one case for diverticulitis with rectovesical fistula, and 2 for rectal invasion, one for bladder tumor and another for cervical cancer) and one wall closure scheduled after intestinal resection for mesenteric ischemia 6 weeks earlier. In addition, an 81-year-old patient who underwent laparoscopic cholecystectomy was admitted 11 days after discharge for COVID-19 pneumonia.
The confirmed SARS-CoV-2 patients were transferred or admitted through the hospital protocol to an isolation floor, with clinical follow-up by an Internal Medicine or Pulmonology team. None of these patients required intensive care due to worsening of symptoms; 3 patients were discharged, 4 remain hospitalized in the ward, and no deaths were registered.
One 42-year-old patient out of the 53 treated in a major ambulatory surgery regimen consulted for fever and digestive symptoms 19 days after open inguinal hernia surgery; the patient was admitted 3 days later for bilateral SARS-CoV-2-positive pneumonia. This contagion was probably community-acquired since it was beyond the maximum 14-day incubation period described for COVID-19.
Impact on Urgent Surgery PatientsDuring the first 10 days of March 2020, 2 patients underwent urgent surgery who were not suspected for COVID-19 infection: one with incarcerated abdominal wall hernia (87 years), and one for perforated acute appendicitis with generalized peritonitis (67 years). In both cases, orotracheal intubation was carried out with general anesthesia and open surgery. Both patients had a positive SARS-CoV-2 result on postoperative days 6 and 8, respectively, after RT-PCR testing. The first patient went to a hospital ward for 48 h, again needing orotracheal intubation and ICU admission for respiratory failure on postoperative day 3, and exitus on postoperative day 9. The second patient remained in the ICU intubated from surgery until death on day 10 after surgery.
Similarly, an 89-year-old patient underwent urgent surgery for acute perforated appendicitis with suspected SARS-CoV-2 infection, suggested by right-basal pneumonia on preoperative chest radiograph as well as compatible respiratory symptoms (cough and dyspnea), although preoperative RT-PCR was negative. Open appendectomy was performed using an infraumbilical midline laparotomy under regional anesthesia, and the surgical team donned personal protective equipment (PPE). This approach was agreed upon with the on-call anesthesiology team in order to reduce the possibility of contagion during orotracheal intubation. The patient died of respiratory failure on the third postoperative day.
Starting on March 24, following the recommendations of the Spanish Association of Surgeons,7 chest CT8 and preoperative RT-PCR were performed on all patients requiring urgent surgery. From March 24 to 31, 6 patients underwent urgent surgery, all of whom were tested with RT-PCR, 5 thoracic CT scan and one chest radiography. All were negative for SARS-CoV-2 infection. During the postoperative period, they had no symptoms until the last day of the review.
Impact of the SARS-CoV-2 Pandemic on the Urgent Care Activity of the General Surgery Department at the Hospital Universitario La PazIn the period from February 1 to 29, 2020, 104 urgent procedures were performed (3.6 surgeries per day). Meanwhile, in the period from March 1 to 31, 36 urgent procedures were performed (1.16 operations per day).
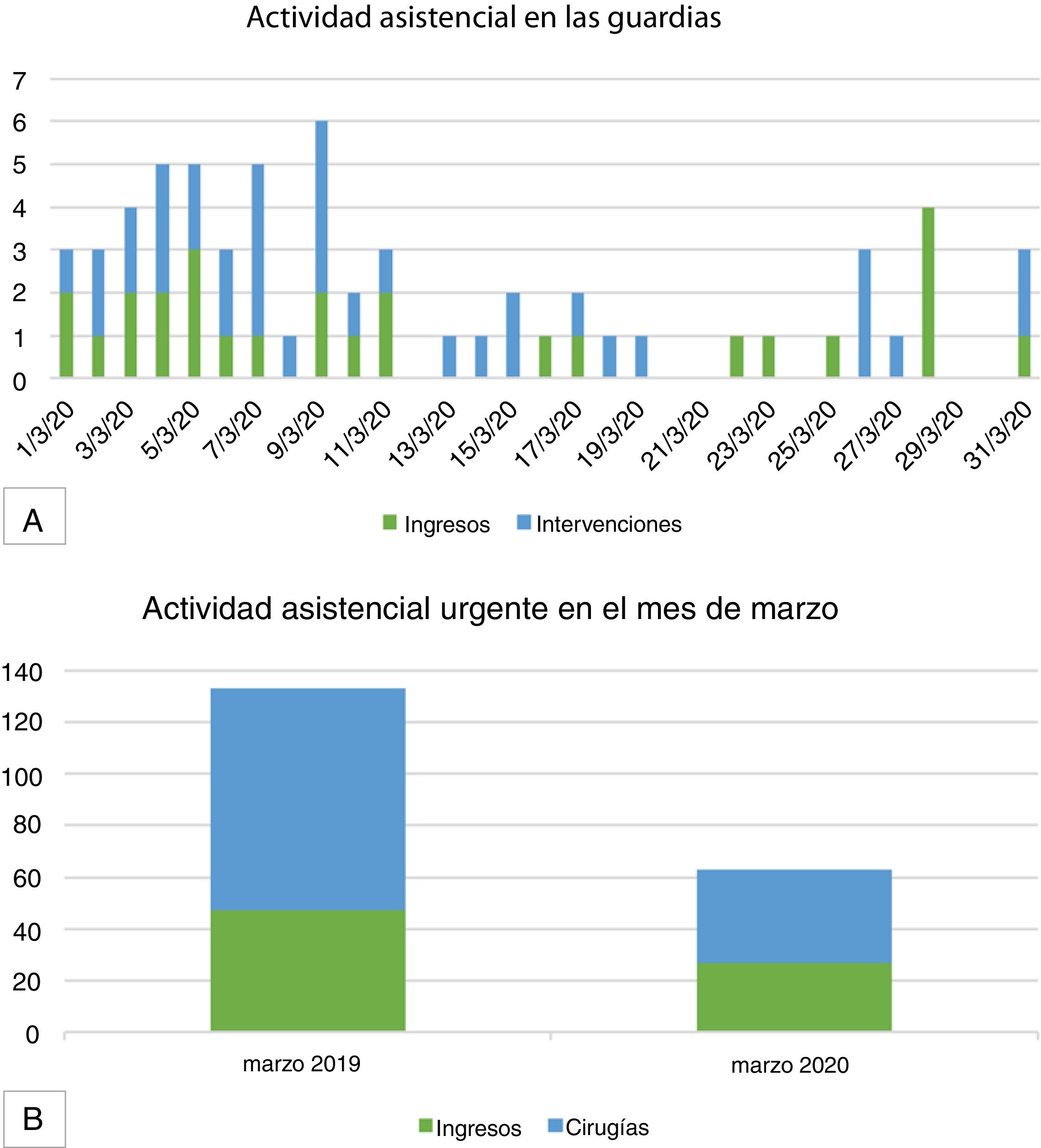
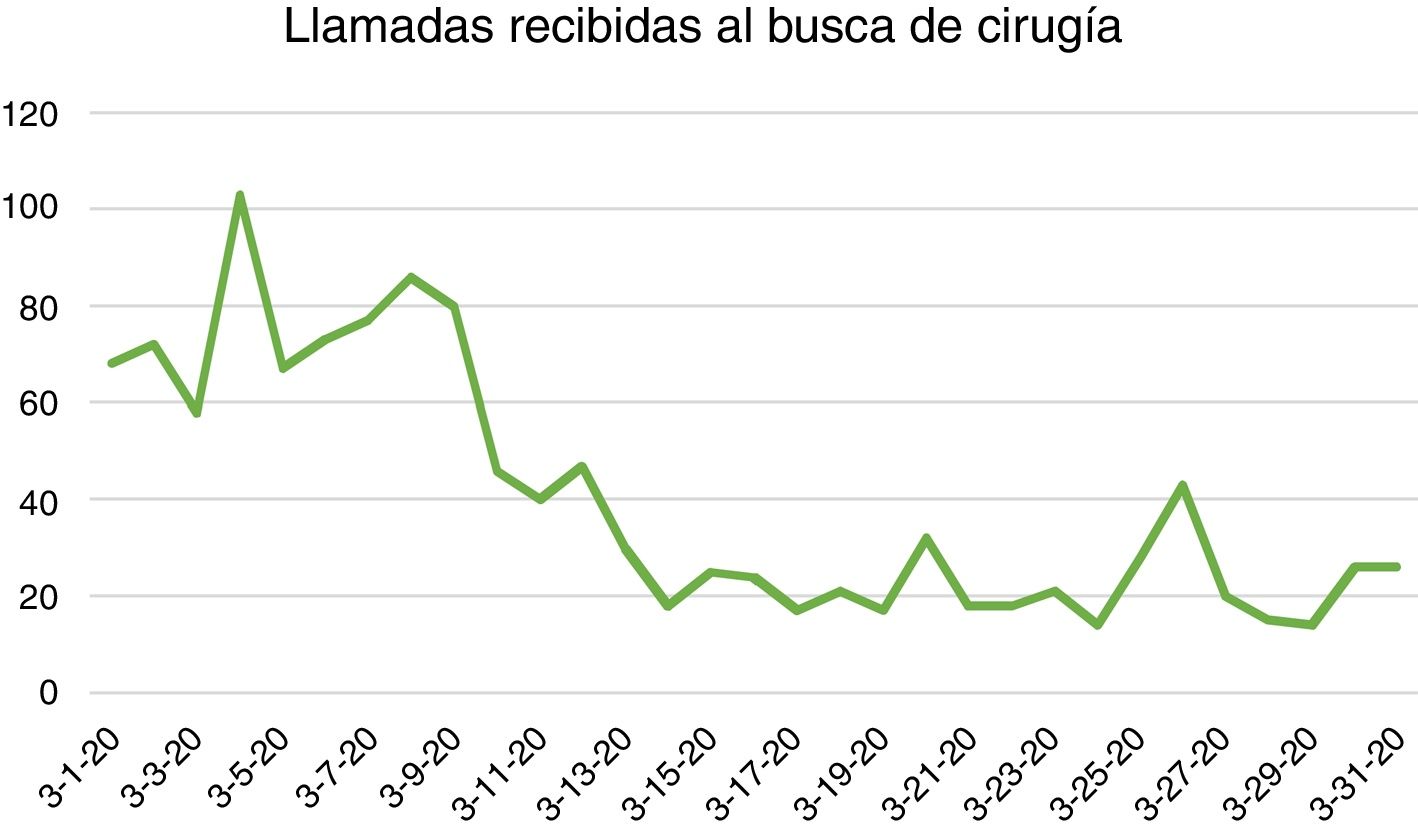
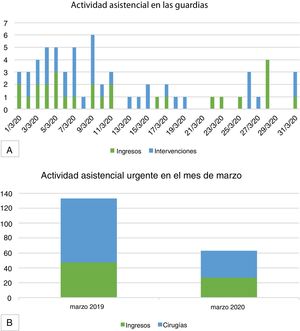
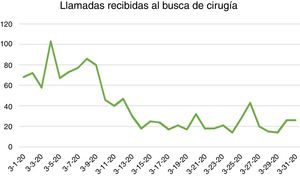
Comparing the activity from March 1 to 31, 2020 with the month of March 2019, the activity (measured in number of admissions and surgical interventions) decreased by 52.7% (Figs. 1 and 2).
A) Daily activity (measured in numbers of admissions and number of urgent surgeries) of on-call general surgery duties in the month of March 2020; B) Urgent care activity in the General Surgery Department (number of admissions and number of urgent surgeries); comparison between the months of March 2019 and March 2020.
From March 1 to March 10, 22 urgent surgical interventions were performed. From March 11 (the day that social isolation measures were activated by the Government of the Community of Madrid) until the 31st, 14 patients were urgently operated on: 4 perforated acute appendicitis with associated peritonitis, 3 phlegmonous appendicitis, one incarcerated incisional hernia, one incarcerated hernia that did not require intestinal resection, 2 acute perforated diverticulitis with peritonitis in which Hartmann operations were performed, one obstructive splenic angle tumor in which a subtotal colectomy with terminal ileostomy was performed, as well as 2 perianal abscesses. In other words, out of the 14 patients who underwent urgent surgery after March 11, 42% presented peritonitis at diagnosis.
During this period of time, interdisciplinary consultations of COVID-19 patients potentially requiring surgery have also been carried out. Six patients were evaluated: 2 had acute cholecystitis, and one had an appendicular plastron that was treated conservatively with antibiotics. Another patient had an incarcerated inguinal hernia that was reduced in the hospital ward. Conservative treatment was used to treat 2 patients with thrombosis of the mesenteric vein and rectus sheath hematoma.
Thus, in all patients with SARS-CoV-2 infection who were hospitalized with pathologies that potentially required surgery, conservative treatment was successful.
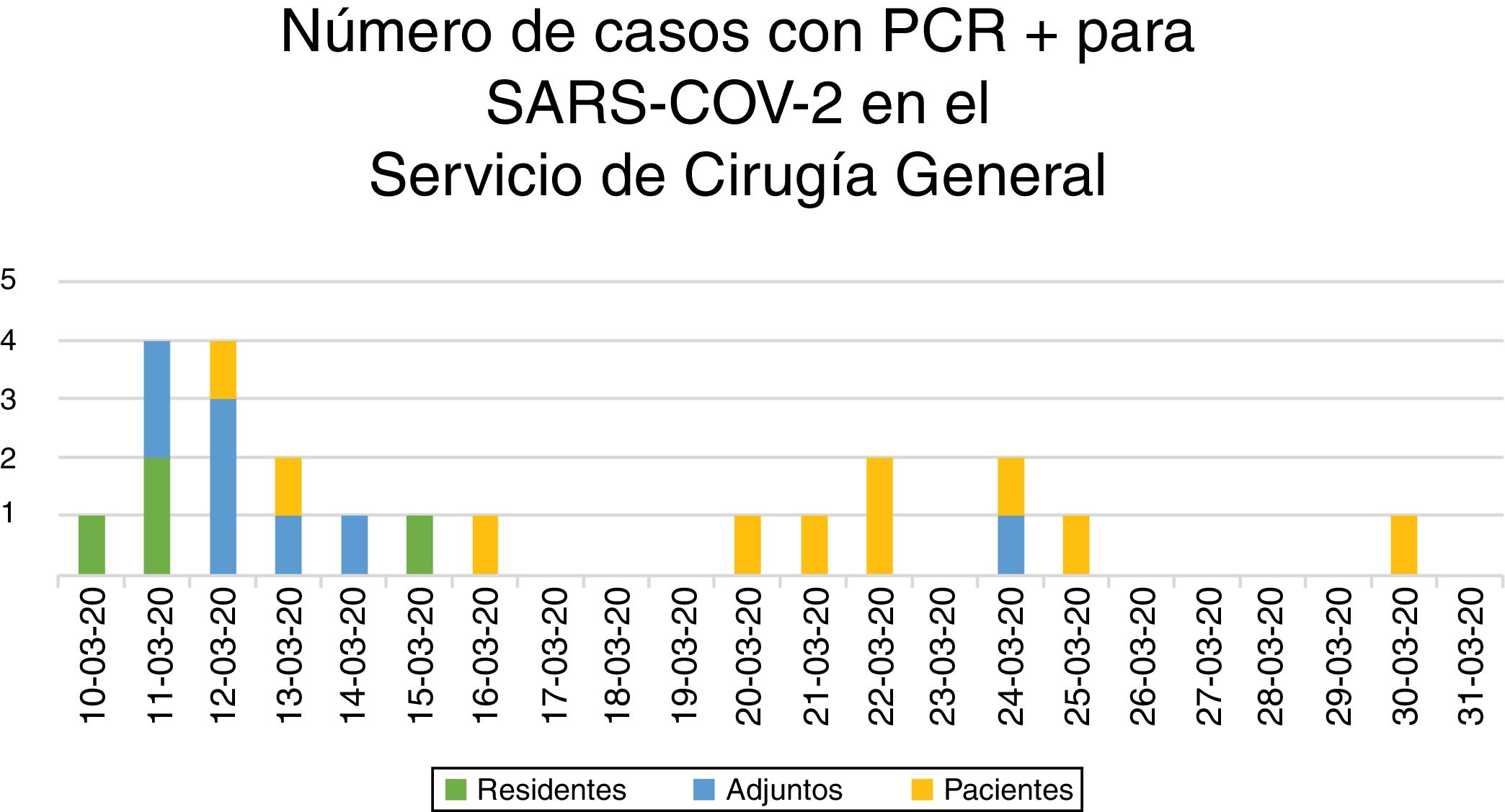
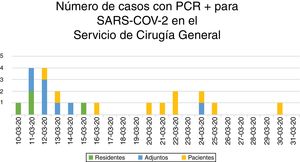
Impact of the SARS-CoV-2 Pandemic on Surgeons of the General Surgery DepartmentThe period of maximum concentration of cases among surgeons of the General Surgery Department, confirmed with positive RT-PCR for SARS-CoV-2, was between March 10 and 15, with the appearance of 11 cases (7 attendings and 4 residents), and fever was the main symptom (10 out of 11) (Figs. 3 and 4). In addition, that same week PCR was performed for respiratory symptoms on 4 surgeons, whose results were negative.
Starting March 11, precautionary measures were increased (suspension of clinical sessions and in-person multidisciplinary committee meetings, wearing hospital scrubs and footwear, surgical mask throughout the working day, avoiding touching the face, disinfecting common work surfaces and washing hands with hydroalcoholic solution when entering and leaving the hospital and before and after each patient, even when wearing gloves). From March 15 to March 31, only one new case was reported among the surgeons of the department.
Three male surgeons with BMI ≥ 30 presented bilateral pneumonia, and 2 required hospital admission. One of the cases required ICU care.
DiscussionOn March 9 in the Community of Madrid, the first measures were announced against the rapid expansion of the SARS-CoV-2 coronavirus in order to protect the population. All in-person classes were cancelled, from Early Childhood Education to University levels, which became effective on March 11. Medical consultations, diagnostic tests and non-essential elective surgeries were also cancelled.4
On March 11, the WHO declared the COVID-19 infection as a pandemic,9 and on this day the Community of Madrid registered 1024 infected cases and 32 deaths, in a population of 6.6 × 106 inhabitants.4
Also from this day on, all face-to-face meetings were suspended in the General Surgery Department of the Hospital Universitario La Paz, and multidisciplinary committee meetings were held online.
Likewise, previously scheduled surgical procedures for benign pathology were suspended,10 non-oncological consultations of the Department were canceled, and precautionary measures were maximized among the hospital’s medical and administrative staff.
During the following 2 weeks, elective surgeries were scheduled for cancer patients, selecting the highest priority cases due to the risk of early complications. The patients selected did not present fever or active respiratory pathology either at admission or in days prior, and they had had no direct contact with confirmed COVID-19 cases.
The COVID-19 pandemic has had a significant impact on healthcare systems worldwide. In general surgery services, three relevant aspects have been affected, all of which have had significant repercussions on the system:
- a)
Almost complete reduction of scheduled surgical activity, even in oncology patients, selecting only cases with a high risk of obstruction or perforation, and suspension of all other elective surgery for benign pathology.
- b)
Significant reduction of the care burden for on-call services and the number of patients coming to the emergency department with surgical pathologies (appendicitis, cholecystitis, diverticulitis, etc.). Urgent cases present with greater complexity due to more evolved disease or complicated symptoms when patients finally come to the ER.
- c)
The contagion of surgeons, which entails a consequent period of quarantine and home isolation (and even hospital admission in the most acute cases), results in a reduced workforce available for daily activities, the coverage of on-call duties and support for other units in the hospital.
In our case series of highly suspected or confirmed COVID-19 patients, 6 underwent scheduled surgery and 3 had urgent surgery. All patients with urgent procedures died from acute respiratory failure, while the patients treated on a scheduled basis had respiratory symptoms of varying severity, but all responded to medical treatment in a conventional hospital ward, without requiring orotracheal intubation.
We cannot conclude that COVID-19 infection was the differential element between the two groups of patients, since the mean age of each group (81 vs. 59.5 years) and the clinical severity do not enable us to make comparisons.
In the current situation of the SARS-CoV-2 pandemic, the indication for surgery (both for urgent and programmed procedures) must be evaluated individually, and the benefit of surgery should be weighed against existing alternatives (antibiotic therapy, percutaneous drainage, cholecystostomy, stent placement or delayed surgery until the disease is less prevalent).11
In hospitals that serve an area with a high incidence of COVID-19 cases, preoperative screening is recommended for all patients who are to undergo surgery12 (using RT-PCR and/or thoracic CT scan). This is necessary in order to select the best available treatment for the patient, as well as the best approach in case of surgery (laparoscopy or laparotomy) and for healthcare workers to take the necessary protective measures (personal protective equipment).7,8,13,14
In any case, the main objective of patient safety is based on two actions: first, to avoid operating on infected patients who may experience worsened respiratory condition due to intubation and surgical aggression; and, second, to avoid intrahospital infection of non-COVID-19 patients during the postoperative period.15 This has been suggested by various national and international guidelines as the impact of COVID-19 disease on surgical patients has become known.16–18
Despite the initial measures taken, the incidence of COVID-19 among surgeons of the General Surgery Department was high during the first part of the study period (23.5% of attending surgeons and 26.6% of surgery residents of the Department were positive). This was parallel to the rapid increase in cases in an area of high incidence (Community of Madrid). In this first period in which the peak of cases occurred among surgeons, all the key measures for the protection of healthcare personnel were being implemented, and personal contact until then had been the usual.
Transmission probably occurred in the days prior to taking population and hospital measures, as the incubation period for the coronavirus is 2–14 days, with a peak in the appearance of symptoms between days 4 and 5.
After the first confirmed cases in our department, we strictly complied with individual protection measures, as well as disinfection of common areas and the cancellation of physician meetings. These measures, together with the home isolation of all surgeons with suspicious symptoms or confirmed infection, reduced the rate of appearance of new cases.
The infection of healthcare workers is an added concern in the management of this social and health crisis.19,20 From the Spanish Association of Surgeons (AEC), action guidelines have been developed for the treatment of patients who have confirmed or highly suspected SARS-CoV-2 infection, defining which measures must be implemented in general surgery departments at this time. These guidelines are based on the existing literature and are subject to revision as the pandemic evolves in our country.7
A top concern of all healthcare workers, which increases in intensity when someone becomes infected, is the contagion of family members with whom they live. This concern is personal, but it is also institutional because the infection of hospital staff reduces the response capacity of the healthcare system and is a means for propagation of the virus.
ConclusionsThe SARS-CoV-2 pandemic is having a major impact on healthcare systems worldwide, requiring available resources to be reorganized. In order to cope with the rapid spread of the coronavirus and the severity of the symptoms it causes, general surgery departments have to drastically modify their surgical and healthcare activities.
Since the onset of COVID-19 cases in the Community of Madrid, a high incidence of infections has been registered in our Department (24.4%).
The rate of cases with COVID-19 infection managed with surgery and hospitalization was 7%. Mortality was concentrated in senior patients with pathologies requiring urgent surgery.
Conflict of InterestsThe authors have no conflict of interests to declare.
Ayuela García S, Cantero Cid R, Castell Gómez JT, Corripio Sánchez R, Del Castillo Díez F, Díaz San Andrés B, Forero A, Gazo Martínez JA, González Alcolea N, González Gómez C, González Sánchez JA, Guerrero Vaquero A, Gutiérrez Iscar E, Heras Garceau M, Losa Boñar N, Marijuán Martín JL, Mata Juberías A, Moquillaza Soller L, Nasimi Sabbagh R, Pérez Robledo JP, Piñero Redondo S, Prieto Nieto MI, Quadros Borrajo P, Salinas Gómez J, Tone Villanueva F, Valderrábano González S, York E, Zapata Syro C, Arteaga Asensio P, Asensio Gómez L, Chavarrías Torija N, Gegúndez Simón A, Georgiades A, Guevara Martínez J, Marcano Chavez C, Moratilla Lapeña L, Prieto Le Noire F, Ramos Martín P, Saavedra Ambrosy J, Sarmiento Caldas MC, Toribio Vázquez C, Urbieta Jiménez A, Vicario Bravo M, Villadóniga Sánchez A, Yebes Alonso A.
Please cite this article as: Álvarez Gallego M, Gortázar de las Casas S, Pascual Migueláñez I, Rubio-Pérez I, Barragán Serrano C, Álvarez Peña E, et al. Impacto de la pandemia por SARS-CoV-2 sobre la actividad y profesionales de un Servicio de Cirugía General y del Aparato Digestivo en un hospital terciario. Cir Esp. 2020;98:320–327.