Schwannomas are benign tumors derived from Schwann cells that represent approximately 5% of mesenchymal tumors.1 They are most frequently found in the stomach and small intestine, and are uncommon in the duodenum. The only curative treatment is complete surgical resection.2
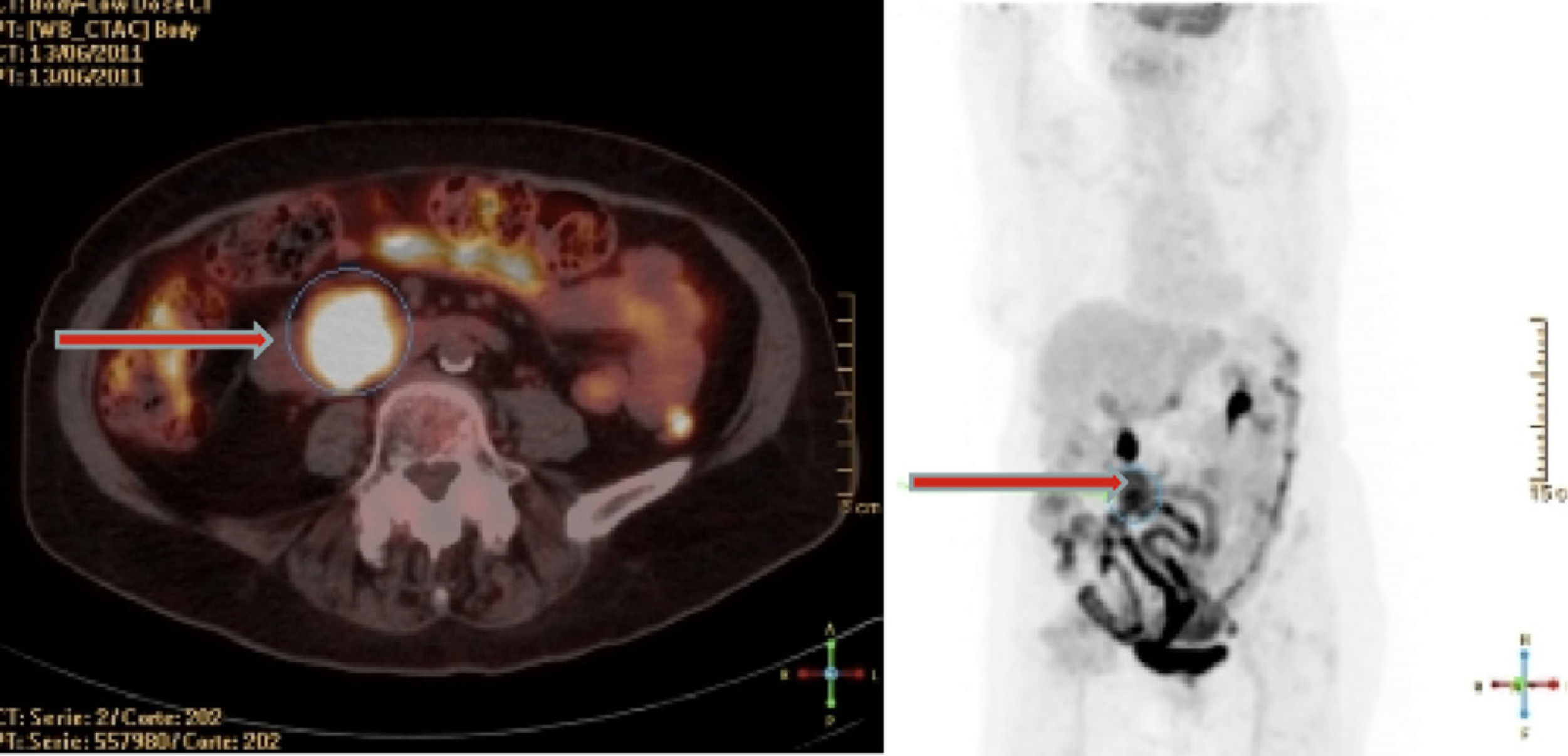
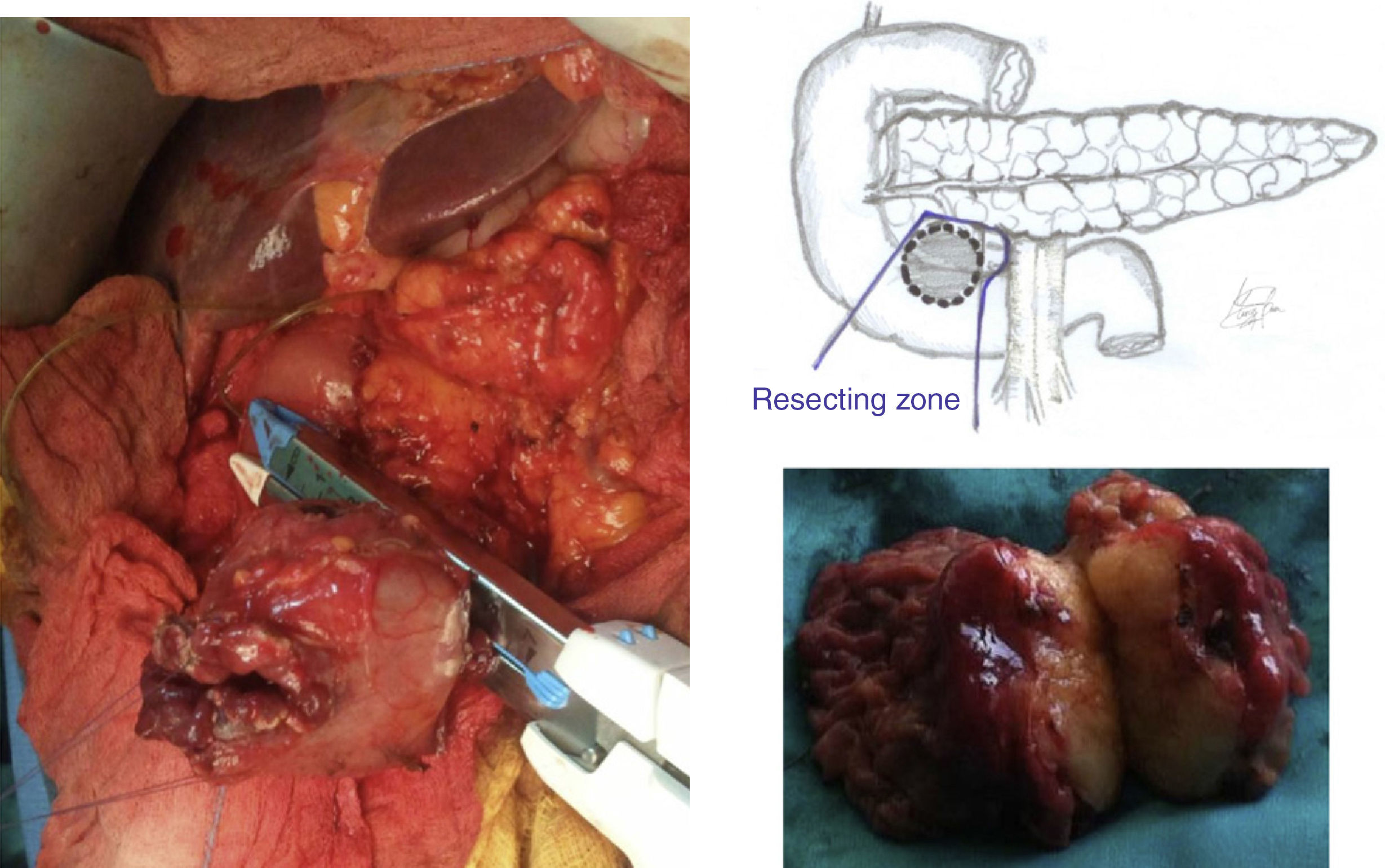
The patient is an 80-year-old woman with a history of arterial hypertension, diabetes mellitus, and osteoarthritis. Due to abdominal discomfort and chronic anemia, an abdominal ultrasound and a tomography were performed that identified a mid-abdominal tumor of the duodenum or uncinate process of the pancreas measuring 5cm in diameter. The gastrointestinal tract showed a defect in the third portion of the duodenum, and upper gastrointestinal endoscopy identified a tumor that was neoplastic in appearance on the upper side of this area. It was ulcerated on the surface and caused partial stenosis of the lumen. Biopsies showed fibrinopurulent material and chronic duodenitis. Positron-emission tomography (PET) detected a mass with pathologic metabolic activity in the third portion of the duodenum (Fig. 1), with a maximum standard uptake value (SUV) of 10.4uCi/ml. After the nuclear magnetic resonance (NMR) angiography study found no evidence of infiltration of the mesenteric-portal axis, the patient underwent surgery. Exploratory laparotomy and an extensive Kocher maneuver were performed, which were able to identify a hard, round tumor measuring 5cm in diameter in the third portion of the duodenum that encompassed the uncinate process of the pancreas but did not affect the superior mesenteric vessels. Cholecystectomy was performed; the transcystic approach was used for cannulation of the papilla, which was 2cm away from the tumor. The proximal and distal duodenum areas were freed from the tumor, avoiding the right gastroepiploic and gastroduodenal arteries, and the duodenal segment and uncinate process were resected en bloc using Ligasure® and a linear endostapler (Fig. 2). The intestinal tract was reconstructed using an end-to-end anastomosis of the duodenum.
Post-op recovery was uneventful with recovery of intestinal transit and oral tolerance, and the patient was discharged on the fifth post-op day. The pathology study diagnosed a duodenal schwannoma measuring 45mm×40mm, with its entire capsule, low cell density, atypical nuclei, and less than 5 mitoses per 50 high-power fields. Immunochemistry was positive for S-100 and negative for CD117 (characteristic of GIST tumors), CD34, actin, desmin, and cytokeratins AE1 and AE3.
Schwannomas are neural tumors of ectodermal origin predominantly located in the muscle wall of the digestive tract, which develop from the Schwann cells of peripheral nerve sheaths in the Meissner and Auerbach plexuses.3 They are usually benign, although they may occasionally become malignant, and surgical resection is therefore required.
The clinical manifestations of these tumors are vague and non-specific, including abdominal discomfort, palpable mass or obstructive symptoms, or more commonly digestive bleeding, as in the case we have presented. A definitive diagnosis is sometimes difficult, as these submucosal tumors may go unnoticed with conventional endoscopy; moreover, taking biopsies from these tumors is also difficult.4 Contrast radiology, ultrasound, computed tomography, NMR, double-balloon enteroscopy, and capsule endoscopy are explorations that can aid in making the diagnosis, while endoscopic ultrasonography is a highly valued technique that allows for directed biopsies to be taken when necessary.5 In the case of malignant tumors, because almost half of cases present metastases (predominantly in the liver), computed tomography is essential for correct extension studies.
In localized tumors, complete surgical resection without lymphadenectomy is the most appropriate therapeutic option. In cases located in the duodenum, it is essential to determine the relationship with the papilla, pancreas, and mesenteric vessels, and require local resection by means of duodenectomy, segmental duodenectomy or even cephalic duodenopancreatectomy in cases of periampullary tumors.6 For tumors found in this location, Nakao proposes resecting the head of pancreas together with a duodenal segment, preserving the right gastroepiploic and gastroduodenal arteries with their duodenal branches as well as the inferior pancreaticoduodenal artery in order to maintain complete vascularization of the third portion of the duodenum.7 However, in the case of our patient, the tumor was in close contact with the uncinate process, without affecting the head of the pancreas or papilla. We therefore decided to perform en bloc resection of the affected duodenal segment and uncinate process, without touching the right gastroepiploic and gastroduodenal arteries, as well as the lower pancreaticoduodenal branches that were not encompassed by the tumor (Fig. 2). This type of “atypical” resection allowed for complete exeresis of the tumor with capsular integrity and free margins, avoiding the need for more aggressive and extensive surgery such as a cephalic duodenopancreatectomy in an elderly patient.
Chemotherapy or radiotherapy are not effective in this type of tumors, and there is no evidence of any type of benefit with imatinib mesylate or other drugs that have demonstrated results of improved survival in the case of other high-risk or advanced gastrointestinal stromal or mesenchymal tumors.8
Tumor size and stage, cell proliferation rate and the state of the resection margins and tumor capsule are the most important prognostic factors in this type of tumors.9 A strict post-operative follow-up is necessary because 30% of cases may present recurrence or metastasis.9 Overall 5-year survival is estimated at approximately 50% in high-risk patients.10
Please cite this article as: Bruna M, et al. Schwannoma de tercera porción duodenal: resección en bloque con inclusión del proceso uncinado del páncreas. Cir Esp. 2013;91:126–8.