Sump syndrome (SS) is defined as the accumulation of bile, biliary sludge, calculi or detritus in the bile reservoir (infraanastomotic common bile duct), either after side-to-side choledochoduodenostomy as the most frequent cause,1,2 or after side-to-side Roux-en-Y hepaticojejunostomy.3
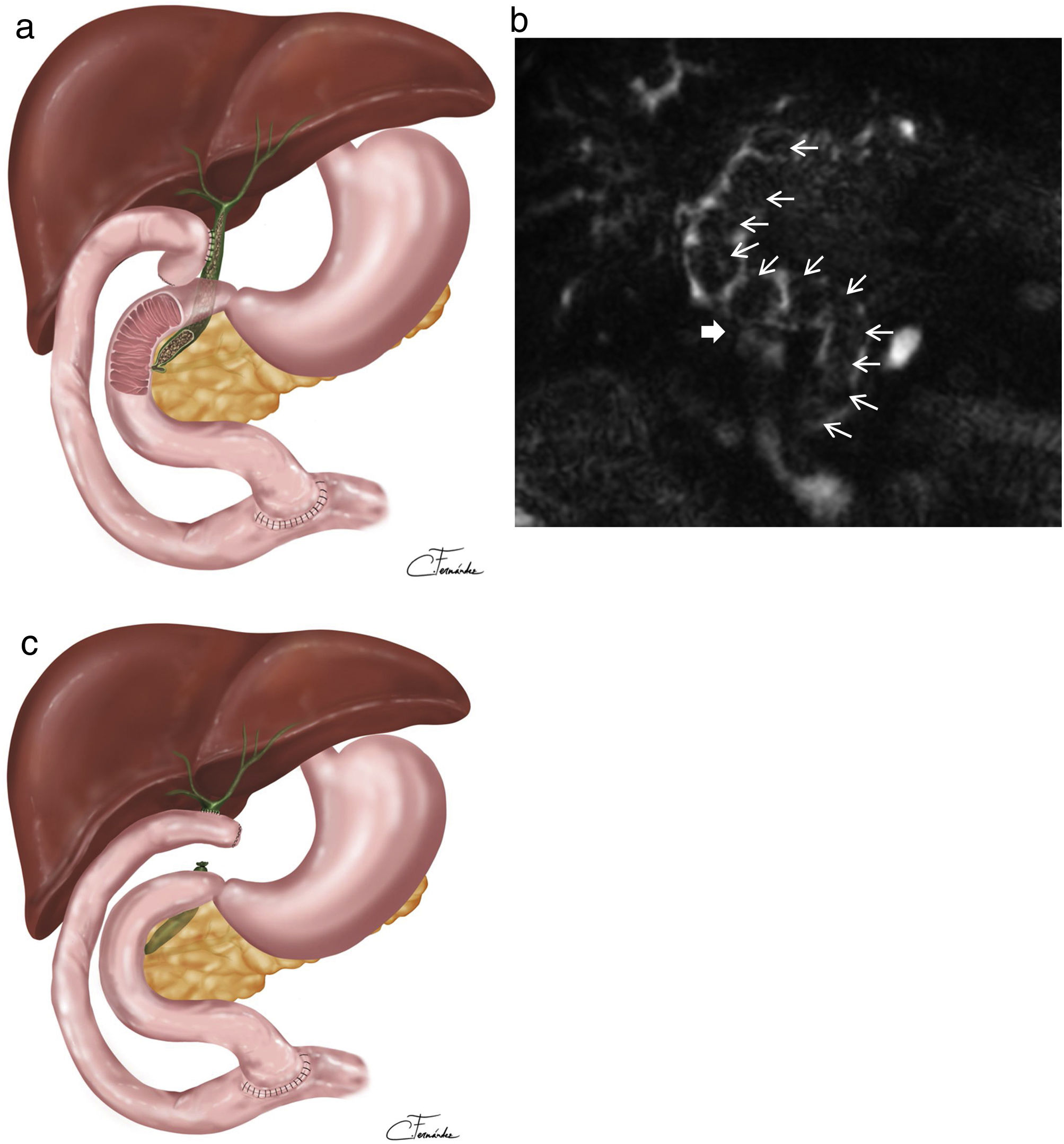
We present 2 cases of SS. The first is a 74-year-old man who underwent Roux-en-Y side-to-side hepaticojejunostomy 26 years ago due to iatrogenic injury to the hepatic duct during laparoscopic cholecystectomy. In the past 2.5 years, he had been hospitalized for multiple episodes of acute cholangitis and various liver abscesses. The patient was treated with antibiotic therapy, PTC-guided dilatations of the hepaticojejunostomy, and placement of a biodegradable stent in 2019. MRI was not performed due to the presence of shot (pellets) after a hunting accident; instead, a CT scan showed dilation of the intrahepatic and extrahepatic bile ducts occupied by gallstones. After a failed papillotomy to remove the common bile duct stones, the patient came to our hospital, where surgery was indicated. Surgery performed 4 months ago revealed almost complete obstruction of the side-to-side hepaticojejunostomy as well as the intra- and extrahepatic bile ducts dilated with biliary sludge and abundant soft calculi (Fig. 1a). A 45-cm afferent jejunal loop was observed; the hepaticojejunostomy was divided, and stones and sludge were removed from the intra- and extrahepatic bile duct using lavage and a Fogarty catheter. Clear passage to the duodenum was confirmed, and the common bile duct was sutured. The bile duct at the confluence was widened to 2.5 cm in diameter by longitudinal division of the left hepatic duct, concluding with an end-to-side hepaticojejunostomy and repositioning of the afferent loop 70 cm from the biliojejunal anastomosis. The postoperative period was uneventful, and the patient has been asymptomatic ever since.
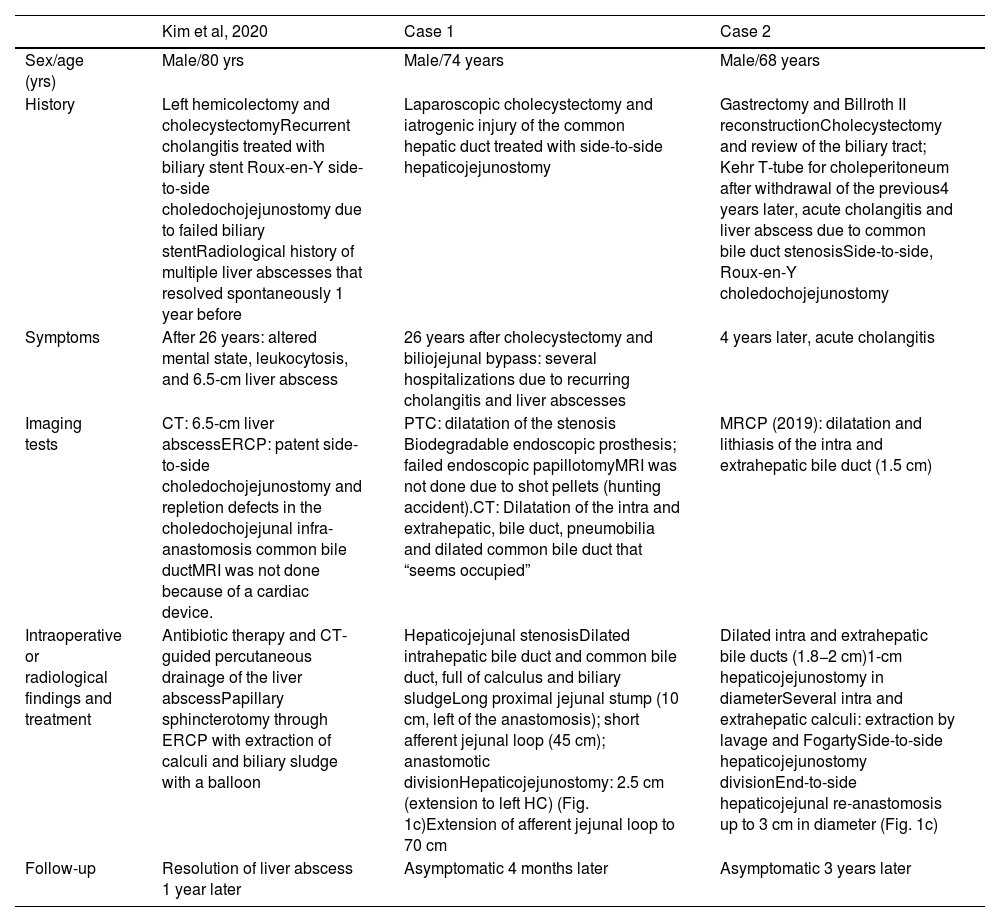
(a) Sump syndrome in side-to-side hepaticojejunostomy due to accumulation of sludge and calculi in the common bile duct below the hepaticojejunal anastomosis. (b) Magnetic resonance cholangiopancreatography in the coronal plane showing dilation of the bile duct due to the presence of numerous lithiases (thin arrows) occupying the proximal extrahepatic and intrahepatic bile duct, in a patient with side-to-side choledochoduodenostomy (thick arrow). (c) Roux-en-Y end-to-side hepaticojejunostomy.
The second case is a 68-year-old male patient with a history of a Roux-en-Y side-to-side hepaticojejunostomy after choledochal stenosis secondary to Kehr tube placement. Four years later, he presented an episode of acute cholangitis; MRI detected lithiasis and a 1.5 cm dilation of the intra and extrahepatic bile duct on magnetic resonance cholangiopancreatography (MRCP) (Fig. 1b). Surgery was indicated due to intrahepatic lithiasis and SS, and we confirmed the permeability of the hepaticojejunostomy (1 cm diameter), intrahepatic and extrahepatic biliary dilatation (1.8−2 cm), and abundant intrahepatic and extrahepatic calculi. As in the first case, the bile duct was enlarged to 3 cm at the confluence, extracting intrahepatic and common bile duct stones and subsequently performing end-to-side Roux-en-Y hepaticojejunostomy with the biliopancreatic limb at a distance of 70 cm. After an uneventful postoperative period, the patient remains asymptomatic 3 years later.
In spite of its rarity, the most frequent presentation of SS is 5–9 years after side-to-side choledochoduodenostomy. Symptoms at presentation may include abdominal pain, fever, cholangitis, pancreatitis, liver abscesses, and moderately elevated liver enzymes, while ERCP sphincterotomy is currently the accepted treatment of choice.2,4,5 When endoscopic treatment is not possible or insufficient, surgical intervention is the most accepted indication.1,2,5
Risk factors for SS are long common bile duct length (below the choledochoduodenostomy or hepaticojejunostomy), choledochoduodenal or hepaticojejunal stenosis, residual or recurrent choledocholithiasis, and papillary stenosis or dysfunction.2,6,7 A case similar to ours is the Kim et al. report3 (Table 1) of a patient treated with side-to-side hepaticojejunostomy who, 26 years later, debuted with symptoms of leukocytosis and a liver abscess measuring 6.5 cm, which was treated with antibiotic therapy, percutaneous drainage and ERCP/papillotomy, extracting calculi and sludge from the common bile duct and showing no evidence of hepaticojejunal stenosis. The indication for surgery in our first case was due to almost complete obstruction of the hepaticojejunostomy and intrahepatic and extrahepatic lithiasis with several failed attempts at ERCP/papillotomy to resolve the SS, while in the second it was due to intrahepatic and extrahepatic lithiasis (within the common bile duct or sump).
Case published in the literature and our experience of 2 cases.
| Kim et al, 2020 | Case 1 | Case 2 | |
|---|---|---|---|
| Sex/age (yrs) | Male/80 yrs | Male/74 years | Male/68 years |
| History | Left hemicolectomy and cholecystectomyRecurrent cholangitis treated with biliary stent Roux-en-Y side-to-side choledochojejunostomy due to failed biliary stentRadiological history of multiple liver abscesses that resolved spontaneously 1 year before | Laparoscopic cholecystectomy and iatrogenic injury of the common hepatic duct treated with side-to-side hepaticojejunostomy | Gastrectomy and Billroth II reconstructionCholecystectomy and review of the biliary tract; Kehr T-tube for choleperitoneum after withdrawal of the previous4 years later, acute cholangitis and liver abscess due to common bile duct stenosisSide-to-side, Roux-en-Y choledochojejunostomy |
| Symptoms | After 26 years: altered mental state, leukocytosis, and 6.5-cm liver abscess | 26 years after cholecystectomy and biliojejunal bypass: several hospitalizations due to recurring cholangitis and liver abscesses | 4 years later, acute cholangitis |
| Imaging tests | CT: 6.5-cm liver abscessERCP: patent side-to-side choledochojejunostomy and repletion defects in the choledochojejunal infra-anastomosis common bile ductMRI was not done because of a cardiac device. | PTC: dilatation of the stenosis Biodegradable endoscopic prosthesis; failed endoscopic papillotomyMRI was not done due to shot pellets (hunting accident).CT: Dilatation of the intra and extrahepatic, bile duct, pneumobilia and dilated common bile duct that “seems occupied” | MRCP (2019): dilatation and lithiasis of the intra and extrahepatic bile duct (1.5 cm) |
| Intraoperative or radiological findings and treatment | Antibiotic therapy and CT-guided percutaneous drainage of the liver abscessPapillary sphincterotomy through ERCP with extraction of calculi and biliary sludge with a balloon | Hepaticojejunal stenosisDilated intrahepatic bile duct and common bile duct, full of calculus and biliary sludgeLong proximal jejunal stump (10 cm, left of the anastomosis); short afferent jejunal loop (45 cm); anastomotic divisionHepaticojejunostomy: 2.5 cm (extension to left HC) (Fig. 1c)Extension of afferent jejunal loop to 70 cm | Dilated intra and extrahepatic bile ducts (1.8−2 cm)1-cm hepaticojejunostomy in diameterSeveral intra and extrahepatic calculi: extraction by lavage and FogartySide-to-side hepaticojejunostomy divisionEnd-to-side hepaticojejunal re-anastomosis up to 3 cm in diameter (Fig. 1c) |
| Follow-up | Resolution of liver abscess 1 year later | Asymptomatic 4 months later | Asymptomatic 3 years later |
We believe that, in our first case, the almost complete hepaticojejunal stenosis and papilla dysfunction or stenosis that would facilitate the passage of bile to the infrahepaticojejunal common bile duct must have contributed significantly to the development of SS, in addition to the short afferent loop (45 cm) that facilitated the ascending cholangitis. Side-to-side hepaticojejunostomy has been reported with good results in patients with biliary iatrogenesis based on less dissection, which prevents biliary ischemia.8 However, end-to-side hepaticojejunostomy prevents SS, since common bile duct closure prevents the passage of bile and calculi into the common bile duct.8
A rare case of patent end-to-side post-hepaticojejunostomy SS has recently been published, caused by fistulization between the afferent loop (2 cm below the hepaticojejunostomy) and the distal common bile duct, resulting in recurrent cholangitis, which was treated by papillotomy.9
SS associated with side-to-side hepaticojejunostomy (currently rarely used) is extremely rare. Our experience presents 2 patients who were treated surgically for intrahepatic lithiasis and associated hepaticojejunal stenosis in the first case, with favorable outcomes.
FundingThe authors have received no funding.
Conflicts of interestsThe authors have no conflicts of interests to declare.