Oesophageal perforation or division in the course of thyroidectomy is an extremely uncommon but potentially serious complication that requires complex treatment. Only 7 cases have been published to date,1–6 and none of them reports a circumferential oesophageal lesion, as the case we present.
A 62-year-old woman with no relevant medical history had undergone total thyroidectomy due to multinodular goitre with a 3cm nodule in the left thyroid lobe. No intraoperative incidents or complications were reported by the surgeons. On the first day post-op, the patient presented a bitonal voice and discharge of ingested fluids through the surgical drain. The patient was reoperated on immediately, at which time a complete division of the cervical oesophagus was observed, which was impossible to repair with a primary closure due to the wide separation between the two oesophageal ends. The proximal oesophageal end was then externalized with a drain tube due to the impossibility of performing a cervical oesophagostomy given its short length; the distal oesophageal stump was closed with non-absorbable monofilament sutures, and a feeding jejunostomy was performed.
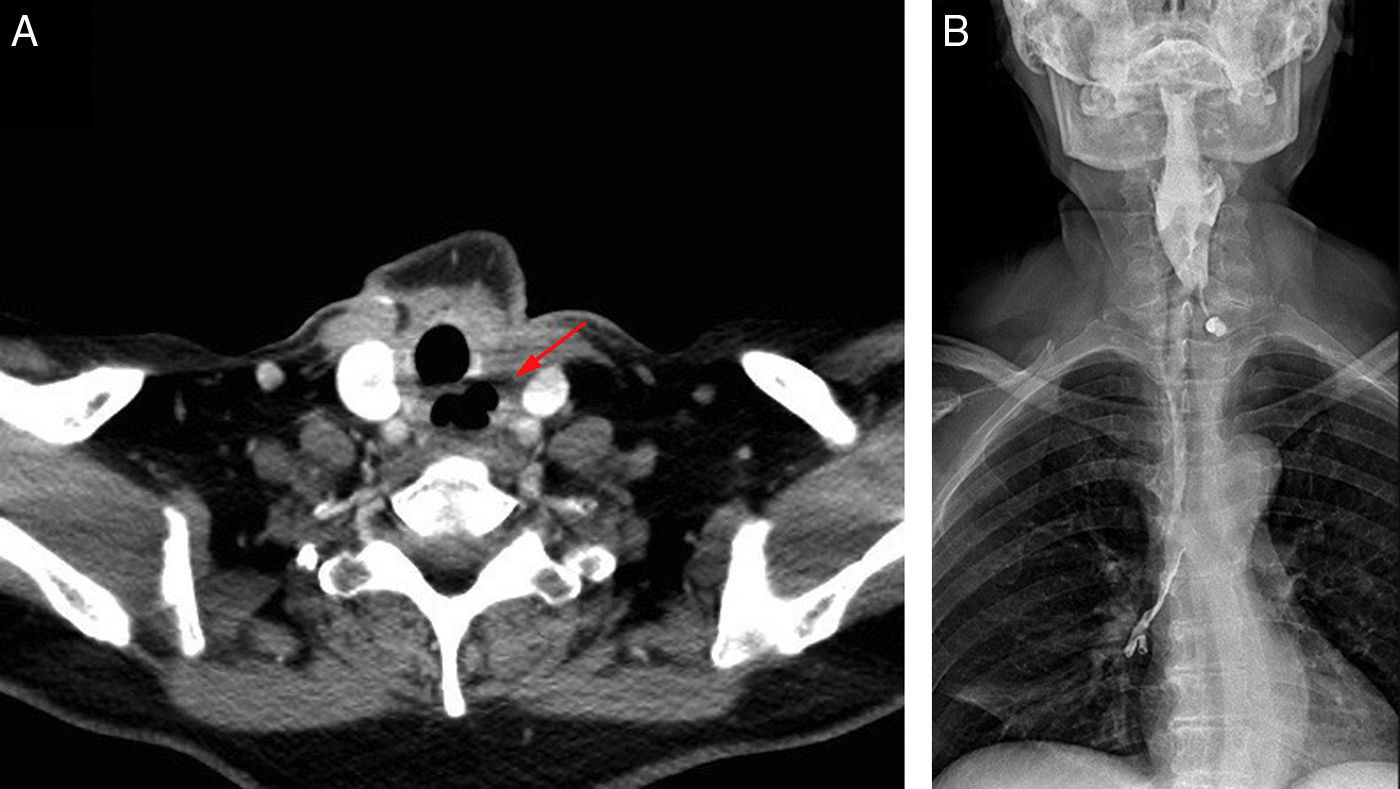
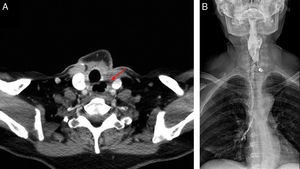
The patient was sent to our hospital 2 months later, where we completed the study with computed tomography (Fig. 1A), laryngoscopy (which demonstrated paralysis of the left vocal cord) and a swallow test (which confirmed the absence of a cervical oesophagus with a salivary fistula) (Fig. 1B), and the proximal oesophageal end was at least 2cm from the upper oesophageal sphincter. Surgery was scheduled for oesophageal reconstruction, at which time the proximal oesophageal end was identified 1.5cm under the cricopharyngeus muscle, while the distal oesophageal end was situated intrathoracically in the upper mediastinum, retracted by intense fibrosis. Its dissection required partial sternotomy, separation of the clavicle and intrathoracic anastomosis. Given these findings, an oesophagectomy was conducted by stripping with retrosternal gastric pull-up reconstruction and manual cervical oesophagogastric anastomosis. The patient's postoperative progress was satisfactory, and one year later she presents correct oral tolerance.
(A) Computed tomography: air space corresponding with a cervical oesophageal defect (arrow). (B) Oesophageal videofluoroscopic swallow study showing contrast extravasation through the cervical oesophageal fistula, with no passage to the distal oesophagus, and aspiration of the contrast to both main bronchi.
When faced with oesophageal perforation, quick treatment in less than 24h is of vital importance to avoid mediastinitis. There is a wide spectrum of therapeutic options,7 including surgical treatment, placement of endoluminal stents, or conservative management with drainage, nil per os and antibiotic therapy. In our case, the initial decision was urgent placement of a surgical drain in order to avoid sepsis and ensure patient survival.
For reconstruction of the cervical oesophagus, different possibilities can be contemplated, including: pedicled flaps or free flaps that may be either visceral or fasciocutaneous. The ascension of a tubular gastroplasty or rotational fundoplication requires a single anastomosis in the cervical region.8 This is the technique of choice when performing oesophagectomy, although the associated morbidity rate is high. Pedicled coloplasty may be a second option when it is not possible to use the stomach. The jejunal free flap is a classic pharyngo-oesophageal reconstruction method requiring 3 gastrointestinal anastomoses and 2 microsurgical vascular anastomoses.9 There are also other visceral free flaps, such as gastro-omental or colon free flaps, although experience with these is still limited.
Fasciocutaneous flaps, such as the radial free flap of the volar forearm and the anterolateral thigh free flap, are also valid options for pharyngo-oesophageal reconstruction of defects up to 15cm in length.10 However, to date there is no evidence on which of the 2 options is the most appropriate. These procedures do not require laparotomy, thereby avoiding associated morbidities. From a strictly theoretical point of view, they would therefore be ideal reconstruction options in short cervical circumferential oesophageal defects.
Undoubtedly, the best treatment for oesophageal lesions that occur during thyroidectomy is prevention through meticulous dissection. But, once they have occurred, cases of fistulas due to partial defects require drainage and conservative treatment.1–4 However, in circumferential defects, surgery is inevitable. We believe that the reconstruction method should always be selected according to the circumstances of each patient, as well as the surgical experience of the surgeon. In our case, tubular gastroplasty and total oesophagectomy were performed because this option allowed for a single cervical anastomosis, thereby avoiding, to the greatest extent, the lethal consequences of mediastinitis due to anastomotic fistula.
It is worth mentioning that the gastric pull-up pathway can be performed through the posterior mediastinum, which is more physiological and provides better functional results, but this requires dilation of the pathway after oesophagectomy by stripping with dilators or by inserting gauze. It should also be stated that immediate reconstruction of the oesophagus could have been carried out initially. However, as this complication was unexpected and difficult to manage, the surgeons opted to first resolve the urgent situation and postpone definitive treatment during surgery at a more experienced hospital, which we did not consider to be an incorrect decision.
In conclusion, oesophageal perforation or division is an extremely uncommon but very serious complication in thyroid surgery that requires complex treatment. In partial defects of the oesophagus, we propose a conservative approach using cervical drainage. When the defects are circumferential, and both oesophageal ends remain in the cervical area, oesophageal reconstruction with visceral or fasciocutaneous free flaps from the forearm or thigh are the best options. In cases in which the distal oesophageal end is situated intrathoracically, we propose oesophagectomy by means of stripping and reconstruction with vertical gastroplasty, as in the case of our patient.
Please cite this article as: Maupoey Ibáñez J, Ballester Pla N, García-Domínguez R, Vaqué Urbaneja J, Mingol Navarro F. Tratamiento de una sección completa esofágica ocasionada en el curso de una tiroidectomía total. Cir Esp. 2017;95:118–120.