The new 8th edition of the TNM classification system for esophageal and cardia or esophagogastric junction cancer provides important innovations in the TNM stages. Two classifications are presented, updated by stages, clinical (cTNM) and pathological (pTNM) methods, together with another pathological classification applicable to cases receiving neoadjuvant treatment (ypTNM). There is a notable increase in complexity compared to previous versions, but it is still early to determine whether the current modifications will result in a clear improvement in the prognostic discrimination of survival among the patient groups (which is their main objective), although the initial expectations are favorable.
La nueva 8.ª edición del sistema de clasificación TNM para el cáncer de esófago y cardias, o de la unión esofagogástrica, aporta importantes novedades en la confección de los estadios TNM. Se presentan 2 clasificaciones actualizadas por estadios, clínicos (cTNM) y patológicos (pTNM), junto a otra clasificación patológica aplicable a los casos que reciben tratamiento neoadyuvante (ypTNM). Hay un notable aumento de la complejidad con respecto a versiones anteriores, pero aún es pronto para conocer si las actuales modificaciones redundarán, como es su objetivo principal, en una manifiesta mejora de la discriminación pronóstica de la supervivencia entre los grupos de pacientes que configuran, si bien las expectativas iniciales son favorables.
In December 2017, the 8th Edition of the American Joint Committee on Cancer (AJCC-TNM) Staging Manual (TNM8) was published.1,2 In certain tumors, such as adenocarcinoma of the esophagogastric junction (EGJ), the manual provides notable changes that aim to refine its potential prognosis in terms of survival, along with possible repercussions in therapeutic management. However, this has resulted in its increased complexity.
The TNM classification system is comparable in objectives and operation to any other prediction model focused on the prognosis of disease survival. Its presumed utility is based on having good calibration and survival determination capabilities among the patient groups that it defines. If properly calibrated, the prognosis within the same group must be similar for all cases that are part of it. If there is good discrimination, the prognosis between the different groups must be clearly differentiated, without overlaps or excessive approximations of their curves on a survival graph. Generally, a model that correctly calibrates also discriminates properly, and while calibration is more important for prognosis, discrimination is in practice a great help for choosing the best therapeutic option. Furthermore, a model that discriminates well is able to stratify the results of a treatment in a randomized trial or constitutes an excellent variable for adjusting these results in a non-randomized trial. First of all, the modifications introduced in the new versions of the TNM classification always seek to improve discrimination and, therefore, to improve its application for therapeutic decision-making in real and research terms.
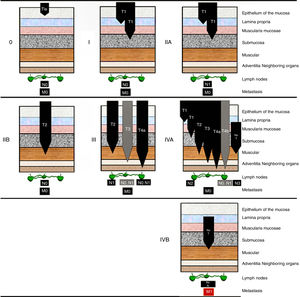
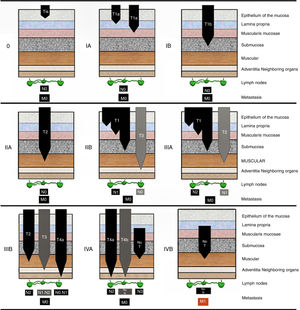
With this objective in mind, experts designed the new TNM8 classification for adenocarcinoma of the EGJ with 3 specific classifications: the first is a clinical classification (cTNM) that is applied before any therapeutic decision is made, based almost exclusively on diagnostic tests; a second pathological classification (pTNM) only applicable after tumor resection; and a third (ypTNM) applicable after neoadjuvant treatment followed by surgical resection. The problems of prognostic discrimination arising in the pTNM classification among the earliest stages (from IA to IIA) have been addressed in part with the introduction of other prognostic factors of recognized importance, such as the histological grade (G) of the tumor, thereby configuring the so-called pTNM-prognostic classification.
It is necessary to emphasize that these 3 basic classifications of adenocarcinoma of the EGJ are also valid for adenocarcinoma of the esophagus but not for squamous cancer of the esophagus, whose cTNM and pTNM have different features. However, for the ypTNM classification, there is no distinction between the two histopathological types of tumors.3 In this review, we will only deal with the TNM classification for adenocarcinoma of the EGJ.
Concepts and ElaborationFor any tumor, the TNM8 classification uses the information of its individual characteristics, which are called “categories”. For EGJ cancer, there are anatomical categories, such as the primary tumor (T), lymph nodes (N) and distant metastases (M), and non-anatomical categories, such as histological grade (G). A stage is defined as a group of categories that reflect a prognosis. The different stages arising from the categories are arranged in ascending order, correlating with a continuous decrease in survival. Within the stages, survival is as homogeneous as possible (calibration), but the contiguous stages are also as differentiated as possible (discrimination).
In order to construct the TNM8 classification system for EGJ cancer, collaborative groups were created at some 40 institutions on 6 continents in 2012 (Worldwide Esophageal Cancer Collaboration) in order to collect necessary data.4–6 Data from more than 22000 patients were analyzed from the standpoint of overall survival, defined by final mortality due to any cause after the initial therapeutic decision. General survival was estimated according to the Kaplan–Meier method without making risk adjustments. Subsequently, the risk functions (hazard function) for death were calculated and adjusted according to a multivariate statistical method of parametric temporal decomposition. The contradictions and inconsistencies in the results of this analysis were resolved by expert consensus.
Categories and TNM StagesIn general, there should be a histological confirmation of the disease and a division of cases according to topographic location and histological type. There is some correlation with the historical classification by Siewert, which is also applicable to adenocarcinomas and establishes 3 groups according to their topographic location. Unlike the TNM, however, the location is oriented toward the implications of the theoretically most appropriate surgical technique. Siewert type I is an adenocarcinoma whose epicenter is located 1–5cm proximally from the anatomical line of the cardia; type II has the epicenter between 1cm proximal and 2cm distal from the mentioned line; type III has the epicenter 2–5cm distal from the same anatomical line of the cardia, that is, in the stomach. In the TNM8, tumors whose epicenter are located 2cm proximal or distal to the anatomical EGJ are considered adenocarcinomas of the EGJ, which would correspond with some types I and all types II of the Siewert classification. A tumor with a more proximal epicenter would be considered an adenocarcinoma of the esophagus; this would include the remaining Siewert I tumors that the TNM8 classification does not consider as belonging to the EGJ itself. If the tumor epicenter is more distal than 2cm from the anatomical EGJ, the tumor would be considered and classified as gastric cancer. Thus, according to the TNM8 system, a Siewert III tumor is a gastric cancer that may or may not invade the esophagus. This implies a conceptual change compared to the 7th TNM edition, in which Siewert III tumors should be classified as esophageal cancer if they invade this organ proximally.7 This conceptual regrouping based on the prognosis for survival of adenocarcinomas of the esophagus and of the EGJ may have surgical repercussions because it indirectly suggests that Siewert I and II should perhaps be theoretically treated like any esophageal cancer, using subtotal esophagectomy, while a Siewert III could be treated by total gastrectomy extended to the distal esophagus. In any case, the best surgical technique to intervene the conflicting Siewert II tumors is still far from being clarified.8
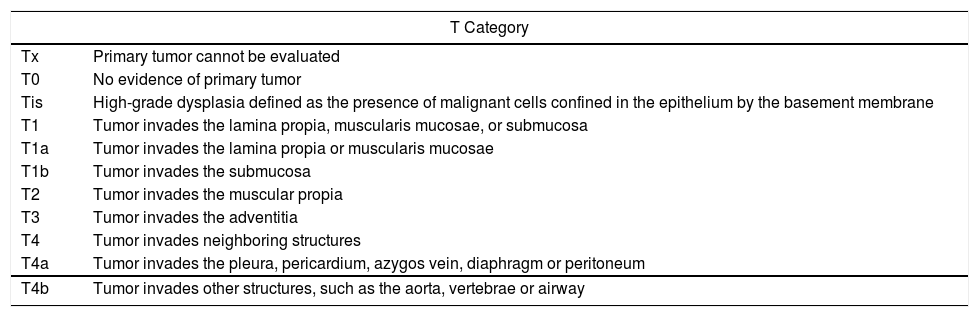
Regarding T category, the different groups or subcategories have not changed from the previous TNM edition, except for the inclusion of peritoneal invasion for T4a tumors. The lymph nodes to be analyzed (N), regardless of the location of the primary tumor, are those included in the esophageal lymphatic drainage area, also considering the cervical paraesophageal lymph nodes and those dependent on the celiac trunk, but not the supraclavicular.9 It is necessary to analyze at least 7 nodes (in case they were all positive) in order to establish the pN3 subcategory. An issue that the TNM8 system does not address is the number of lymph nodes to be analyzed to establish a pN0 case with sufficient guarantees if all were negative. However, it does establish that when less than 7 negative nodes are analyzed, the case will be classified as pN0.1,2 TNM categories can be obtained by physical examination, imaging tests, or by surgical examination, to which the information obtained by digestive endoscopy or airway endoscopy is added in category T. Table 1 shows the TNM categorization.
TNM8 Categories for EGJ Cancer.
| T Category | |
|---|---|
| Tx | Primary tumor cannot be evaluated |
| T0 | No evidence of primary tumor |
| Tis | High-grade dysplasia defined as the presence of malignant cells confined in the epithelium by the basement membrane |
| T1 | Tumor invades the lamina propia, muscularis mucosae, or submucosa |
| T1a | Tumor invades the lamina propia or muscularis mucosae |
| T1b | Tumor invades the submucosa |
| T2 | Tumor invades the muscular propia |
| T3 | Tumor invades the adventitia |
| T4 | Tumor invades neighboring structures |
| T4a | Tumor invades the pleura, pericardium, azygos vein, diaphragm or peritoneum |
| T4b | Tumor invades other structures, such as the aorta, vertebrae or airway |
| Category N | |
|---|---|
| Nx | Regional lymph nodes cannot be evaluated |
| N0 | No metastasis in the regional lymph nodes |
| N1 | Metastasis in 1–2 regional lymph nodes |
| N2 | Metastasis in 3–6 regional lymph nodes |
| N3 | Metastasis in 7 or more regional lymph nodes |
| Category M | |
|---|---|
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Category G: Histology Grade | |
|---|---|
| Gx | Unknown grade |
| G1 | Well differentiated |
| G2 | Moderately differentiated |
| G3 | Poorly differentiated or undifferentiated |
As mentioned above, the grouping of categories into stages for adenocarcinoma of EGJ has created 3 TNM classifications: clinical (cTNM), pathological (pTNM) in its ‘pure’ version or with the addition of the histological grade (prognostic pTNM), and the pathological type combined with neoadjuvant therapy (ypTNM). The introduction of these 3 differentiated classifications, with the increase in complexity involved, is due to several compelling reasons.3 In the past, the survival prognosis was established on pathological findings after surgical resection as the only main treatment (pTNM); however, this is not enough to make the initial therapeutic decisions that are based on clinical and imaging findings, yet on very limited histopathological data. On the other hand, currently and in many cases the neoadjuvant treatment administered modifies the final pathological findings, especially in advanced stages, with the consequent appearance of certain groups of unlikely categories for said pathological classification, such as TisN1-3M0 or T0N1-3M0. Finally, the pTNM classification loses relevance in the more advanced stages, in which neoadjuvant therapy is usually administered, because the prognosis is similarly terminal in all of them, unlike in the early stages.
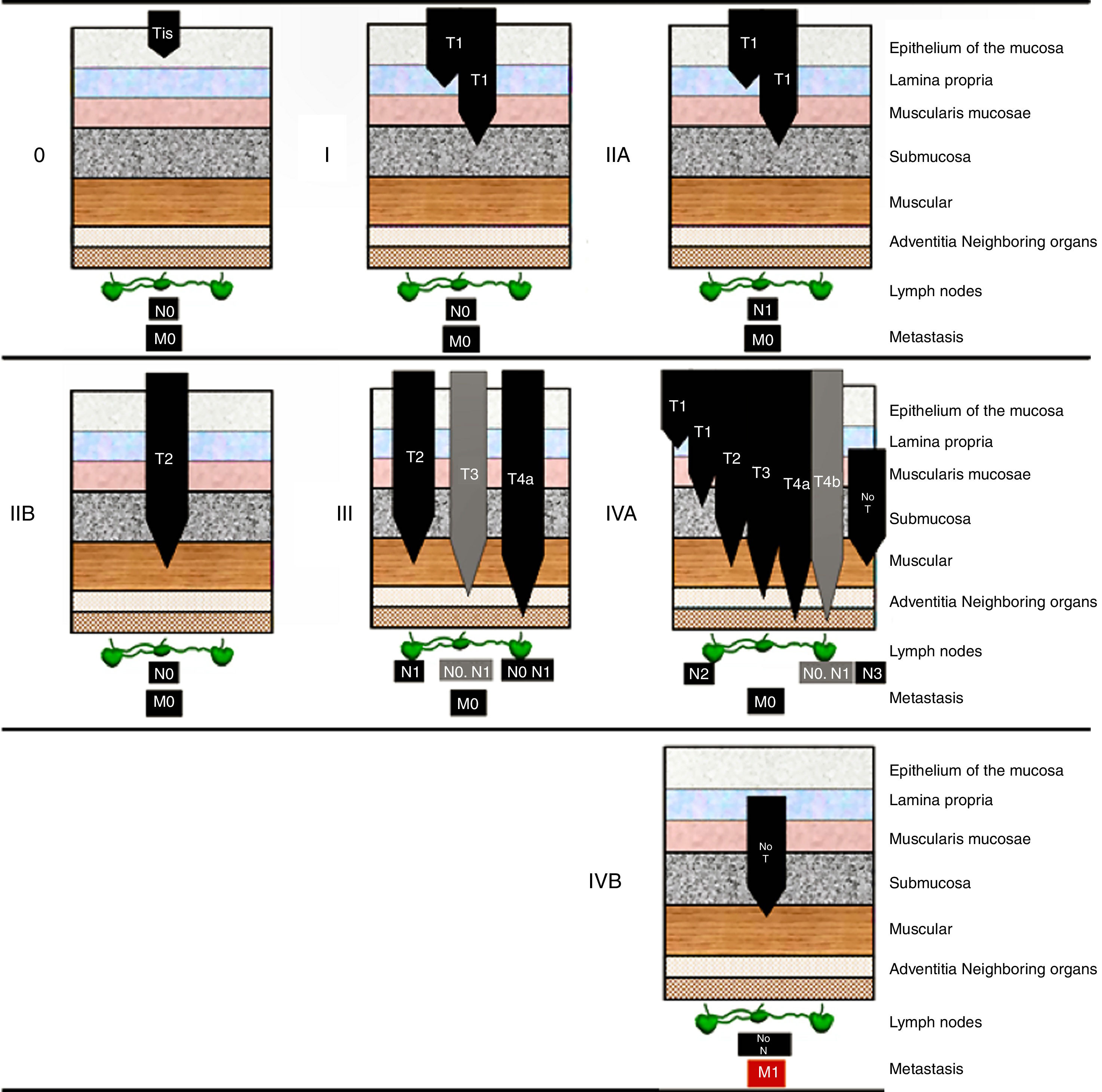
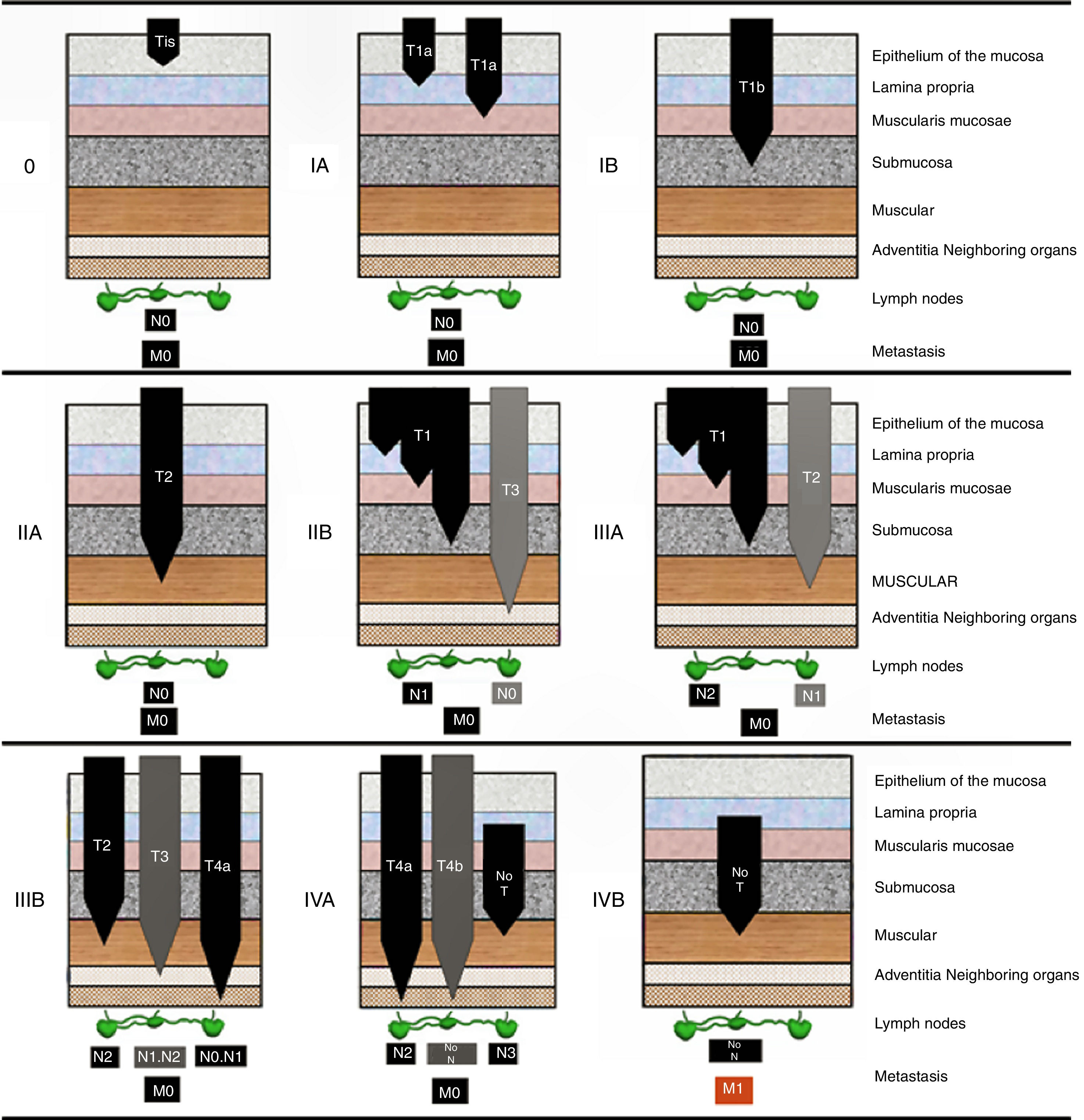
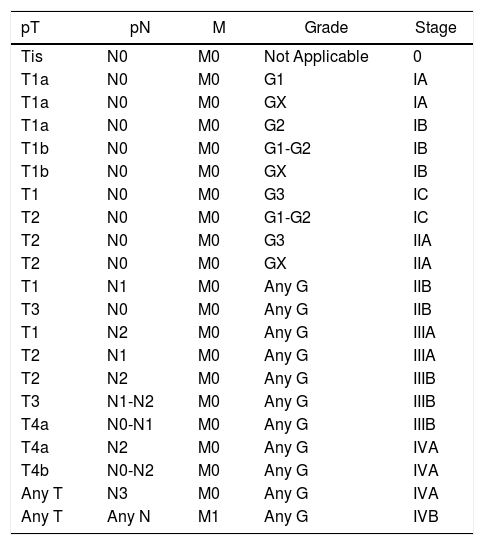
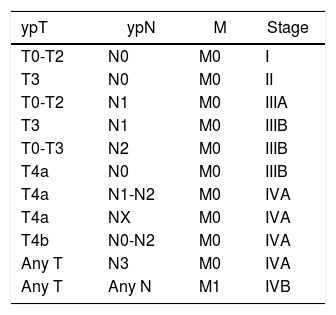
The new cTNM and pTNM stages are shown as diagrams in Figs. 1 and 2, respectively. The prognostic pTNM stages and the ypTNM stages are shown in Tables 2 and 3, respectively.
pTNM Stages That Are Prognostic for GEJ Adenocarcinoma.
| pT | pN | M | Grade | Stage |
|---|---|---|---|---|
| Tis | N0 | M0 | Not Applicable | 0 |
| T1a | N0 | M0 | G1 | IA |
| T1a | N0 | M0 | GX | IA |
| T1a | N0 | M0 | G2 | IB |
| T1b | N0 | M0 | G1-G2 | IB |
| T1b | N0 | M0 | GX | IB |
| T1 | N0 | M0 | G3 | IC |
| T2 | N0 | M0 | G1-G2 | IC |
| T2 | N0 | M0 | G3 | IIA |
| T2 | N0 | M0 | GX | IIA |
| T1 | N1 | M0 | Any G | IIB |
| T3 | N0 | M0 | Any G | IIB |
| T1 | N2 | M0 | Any G | IIIA |
| T2 | N1 | M0 | Any G | IIIA |
| T2 | N2 | M0 | Any G | IIIB |
| T3 | N1-N2 | M0 | Any G | IIIB |
| T4a | N0-N1 | M0 | Any G | IIIB |
| T4a | N2 | M0 | Any G | IVA |
| T4b | N0-N2 | M0 | Any G | IVA |
| Any T | N3 | M0 | Any G | IVA |
| Any T | Any N | M1 | Any G | IVB |
The TNM classification system is a prognostic model and, like any prognostic model, it should be validated (confirming goodness of fit) in our own patients if we want to know how useful it is to us. Generally, a model like the TNM that claims to be universal will work quite accurately in many specific environments, but this does not absolutely guarantee all its parts or components. Simple, visual, and immediate verification would entail creating general survival curves (such as Kaplan–Meier graphs) using our own data, without adjustment. In this way, we can determine whether the TNM classification has significant discrimination gaps in the survival prognosis of our patients. If few cases are analyzed, these defects are more likely.
When a new TNM version appears, validation studies are published (often with disparate results) about the value of the new contributions of the analyzed classification.10 The external validity of these studies is minimal, unless our own patient population and our patient management methods are very similar. As for the TNM8 classification for EGJ cancer, there is still little bibliographic material due to its short life span. For now, published studies focus more on the prognostic value of the ypTNM, which may be the most important novelty. Currently, it seems to provide advantages over previous systems, although its usefulness to determine the administration of additional treatments after surgery is limited.11,12
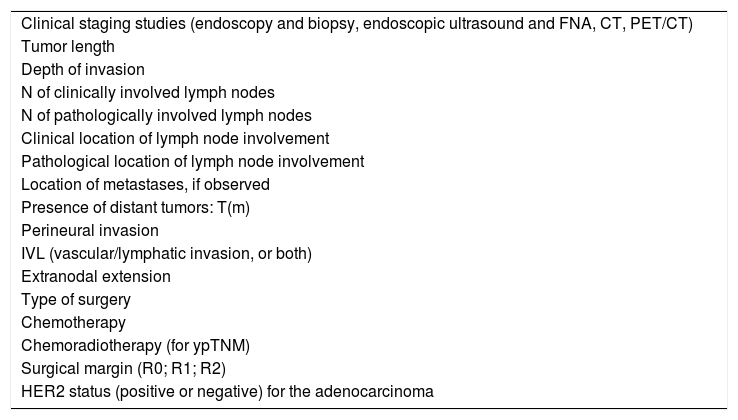
All this means that there is ample room for improvement. Prognostic factors of recognized individual value, such as lymph node ratios, lymphovascular invasion, certain genetic and molecular markers, still have not become part of the categories. For future modifications of the TNM system, it is essential for the various groups that treat these patients to meticulously record specific data that can be used for this purpose, apart from constantly updating the survival data of these patients. In this direction, some of the experts3 who have developed the TNM8 classification have proposed registering a minimum number or variables, as shown in Table 4.
Basic EGJ Cancer Registry Data.
| Clinical staging studies (endoscopy and biopsy, endoscopic ultrasound and FNA, CT, PET/CT) |
| Tumor length |
| Depth of invasion |
| N of clinically involved lymph nodes |
| N of pathologically involved lymph nodes |
| Clinical location of lymph node involvement |
| Pathological location of lymph node involvement |
| Location of metastases, if observed |
| Presence of distant tumors: T(m) |
| Perineural invasion |
| IVL (vascular/lymphatic invasion, or both) |
| Extranodal extension |
| Type of surgery |
| Chemotherapy |
| Chemoradiotherapy (for ypTNM) |
| Surgical margin (R0; R1; R2) |
| HER2 status (positive or negative) for the adenocarcinoma |
More generally, to cover future expectations of improvement in the TNM8 classification, the registration of collected data should be oriented toward a series of strategic points3: (1) more precise clinical staging; (2) the search for solutions for pathological staging in endoscopically resected cancers; (3) the integration of genomics in staging; and (4) the consideration of individualized treatments with target therapies.
Conflict of InterestsThere are no conflicts of interest.
Please cite this article as: Escrig Sos J, Gómez Quiles L, Maiocchi K. La 8.ª edición de la clasificación AJCC-TNM: nuevas aportaciones a la estadificación del cáncer de la unión esofagogástrica. Cir Esp. 2019;97:432–437.