Postoperative ileus is one of the main complications in the postoperative period. New measures appeared with the introduction of “fast-track surgery” to accelerate recovery: coffee, chewing gum and gastrograffin. We performed a summary of current evidence, reviewing articles from MEDLINE, Cochrane Database of Systematic Reviews, ISI Web of Science, and SCOPUS databases. Employed search terms were “postoperative ileus” AND (“definition” OR “epidemiology” OR “risk factors” OR “Management”). We selected 44 articles: 9 systematic reviews 11 narrative reviews, 13 randomized clinical trials, 6 observational studies, and the remaining 5 scientific letters, assumptions, etc. There is little literature about this topic, studies are heterogeneous, with disparity in the results. In addition, they only focus on colorectal and gynecological surgery. New high-quality studies are needed, preferably randomized clinical trials, in order to clarify the usefulness of these measures.
El íleo paralítico es una de las principales complicaciones del postoperatorio. Con la introducción de los protocolos fast-track para acelerar la recuperación, han aparecido nuevas medidas, como la toma temprana de café, mascar chicle y el gastrografín. Para conocer mejor estas actuaciones, se ha realizado un resumen de la evidencia actual, utilizando las bases de datos de MEDLINE, Cochrane Database of Systematic Reviews, Web of Science y SCOPUS. Los términos empleados fueron «postoperative ileus» AND («definition» OR «epidemiology» OR «risk factors» OR «management»). Se han seleccionado 44 artículos, de los cuales 9 son revisiones sistemáticas, 11 revisiones narrativas, 13 ensayos clínicos aleatorizados, 6 estudios observacionales y los 5 restantes cartas científicas, hipótesis, etc. Se ha visto que existe poca literatura acerca del tema, que los estudios son heterogéneos (con disparidad en los resultados) y se centran en cirugía colorrectal y ginecológica. Se necesitan nuevos estudios, preferentemente ensayos clínicos aleatorizados, que esclarezcan la utilidad de estas medidas.
Postoperative ileus is defined as a dysfunction, mainly of the small intestine after surgery, that has a prevalence of between 5% and 30% in rectal surgery series.1 It entails symptoms that cause patient discomfort, including nausea and vomiting, oral intolerance, abdominal distension, etc.
The physiopathology of this disease is multifactorial,2,3 with a neurogenic component (due to adrenergic activity caused by the aggression of surgery4), inflammatory component (activation of phagocytes of the intestinal wall, with a possible role of the mastocytes, which is still up for debate2,5,6), humoral component (loss of electrolytes, decrease in albumin and fluid overload, with the production of wall edema7) and pharmacological component (overuse of opioid agonists8).
The main treatment of prolonged postoperative ileus2 is the insertion of a nasogastric tube to decompress the digestive tube, a series of follow-up radiographs, correction of the water–electrolyte balance that may have been affected by intestinal losses and the placement of a urinary catheter to monitor diuresis. The use of gastrograffin has also been proposed as a prokinetic agent and for its diagnostic value in the treatment of prolonged ileus, but a recent trial9 has not shown it to be useful.
The objective of this study is to review the current situation of these measures, and to summarize evidence regarding the use of coffee, chewing gum and gastrograffin in the management of postoperative ileus, with a view to future studies to determine their actual utility.
MethodsWe reviewed the most important articles about the management of paralytic ileus, focusing on measures that have created controversy in recent years: the use of coffee, chewing gum and gastrograffin. For the bibliographic search, the following databases were used: MEDLINE (via PubMed), Cochrane Database of Systematic Reviews, ISI Web of Science and SCOPUS. The search terms used included: “postoperative ileus” AND (“definition” OR “epidemiology” OR “risk factors” OR “management”) and, for the more specific bibliographic references for our topic, “postoperative ileus” AND (“chewing gum” OR “coffee” OR “gastrograffin”). To select the articles, we thoroughly read the abstracts of all those publications whose titles had the terms “postoperative ileus” or “postsurgical paralytic ileus” and at least one of the previously stated terms. Preference was given to systematic reviews and randomized clinical trials.
After having selected the articles, each was read critically to rule out the publications that did not meet at least 70% of the criteria proposed by the CASPe for systematic reviews and meta-analyses, clinical trials and cohort studies,10 and we reviewed those articles whose reference had information that was relevant to our topic. Finally, we analyzed the conclusions of each of the articles and organized all the references to be included in this paper with the Mendeley Desktop© program.
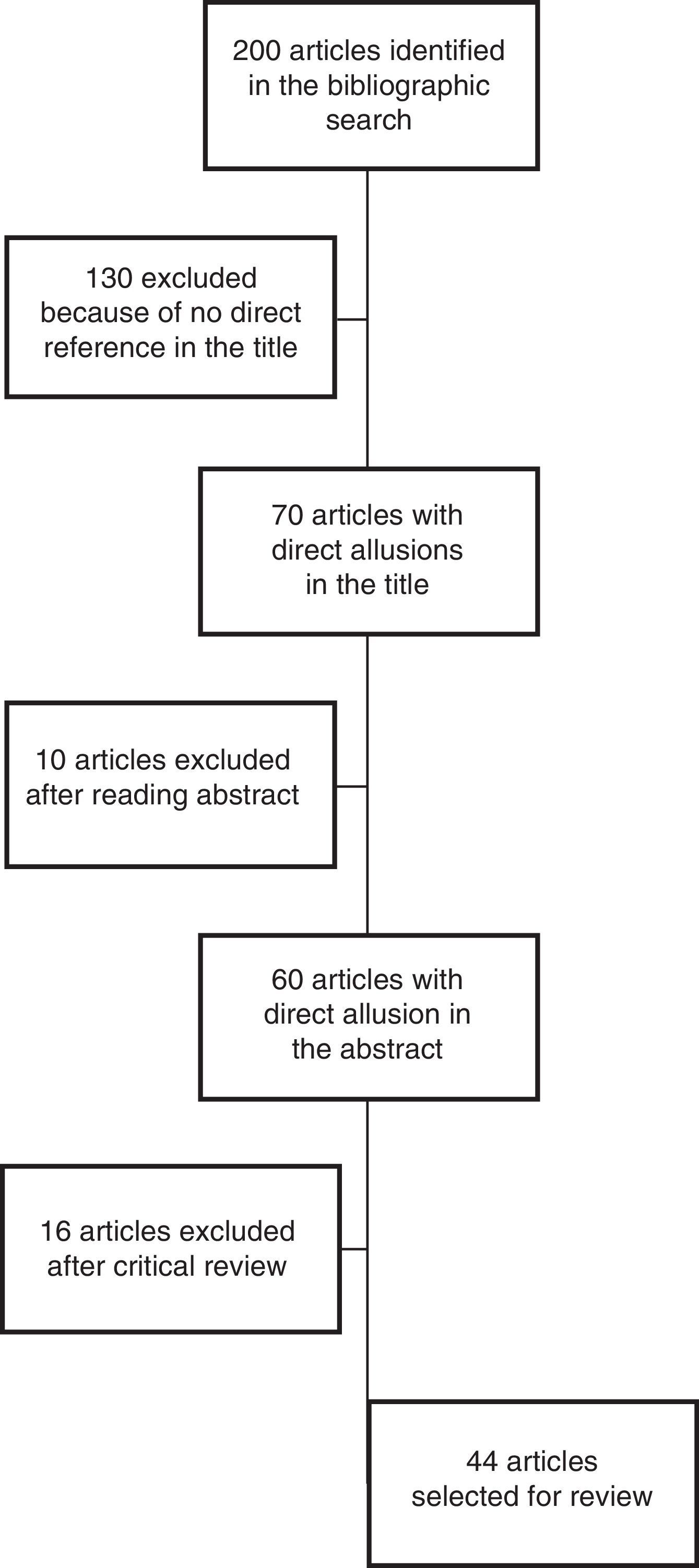
ResultsThe bibliographic search produced a total of 200 articles related with the management of postoperative ileus. Out of these, 70 articles were selected by their title, which directly referred to the subject. After reading the abstract, 10 were excluded, and another 16 articles were excluded after critical review, as they were not considered to have sufficient quality according to the CASPe criteria,10 leaving a total of 44 articles (Fig. 1). From these articles, we have selected the most relevant information from the discussion and conclusions about the definition, risk factors, general management and usefulness of coffee, chewing gum and gastrograffin, which is included in this study.
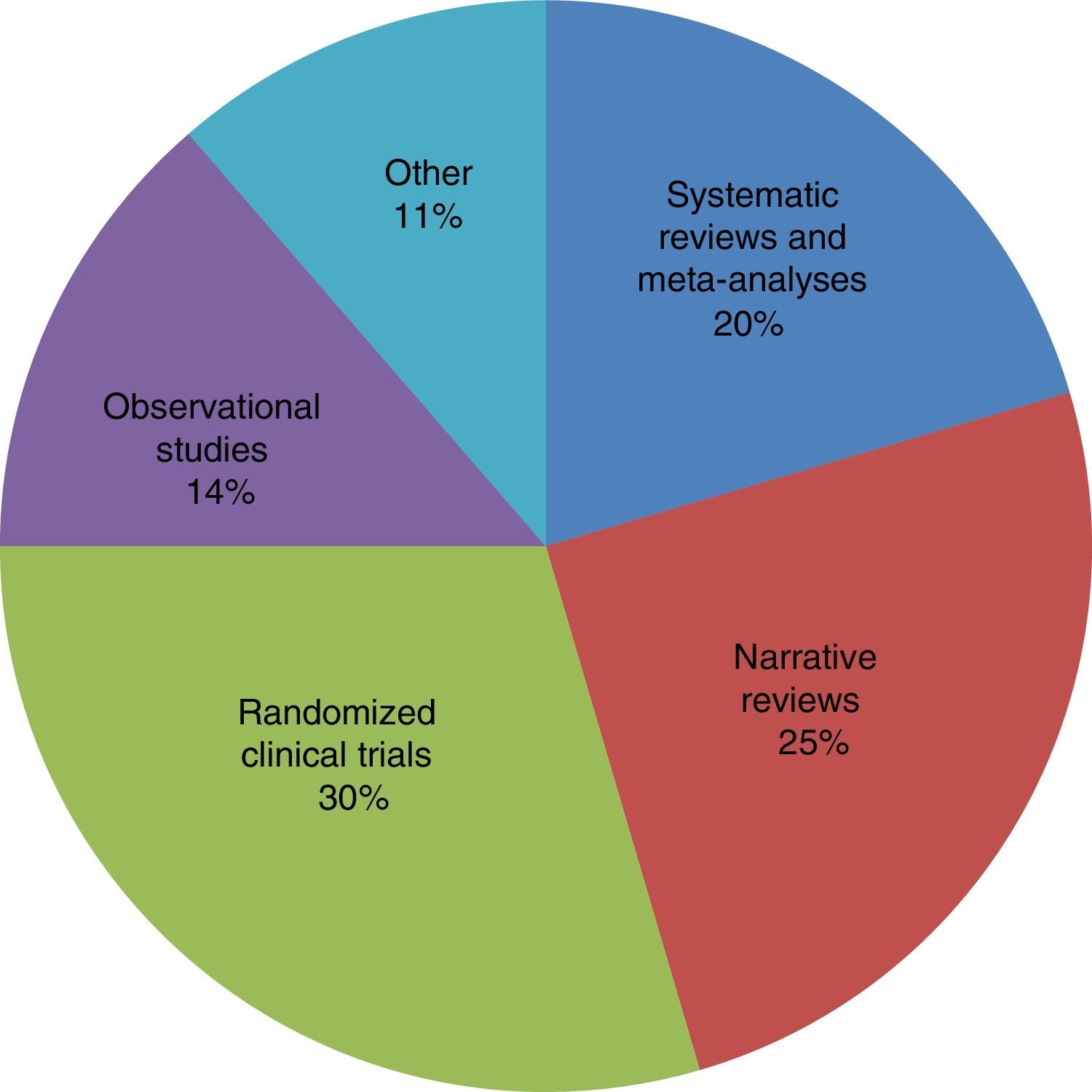
Among the selected articles, 9 were systematic reviews with meta-analyses of prospective studies and clinical trials, 11 narrative or systematic reviews without meta-analyses, 13 randomized clinical trials and 6 observational studies. The remaining 5 were case reports, hypothesis and reviews of the properties of certain studied substances, such as gastrograffin (Fig. 2).
The references used for each section were: for the introduction, 9 references; diagnosis and prevention of postoperative ileus, 15; use of coffee, 4; use of chewing gum, 8; and use of gastrograffin, 8 references, subdivided into 4 for adhesion-related bowel obstruction and another 4 for postoperative ileus. The following section discusses the most important aspects of each article as well as current scientific opinions about the matter in question.
Discussion and Summary of the Evidence FoundDiagnosis and Prevention of Postoperative Paralytic IleusCurrently, there is still no consensus on the moment or criteria to diagnose paralytic ileus.1,11 In 2013, Vather et al.11 proposed the period of 4 days of persisting symptoms to define prolonged postoperative ileus, while Wolthuis et al.1 consider the insertion of a nasogastric tube the main diagnostic–therapeutic criterion.
Several retrospective studies12–15 suggest the correlation of different factors with the risk for developing postoperative paralytic ileus. Independent factors described include: male sex, low preoperative albumin, transfusion of red blood cells, use of opiates and SIRS, and preoperative sepsis. There are other factors, such as laparoscopic surgery, the type of anastomosis performed and the use of epidural analgesia, but current studies are contradictory.13,16 Likewise, possible early postoperative predictive markers have been studied, including the increase in Th1 lymphocytes, monocytes, circulating PMN and serum IL-12, although the results have not been conclusive.17
As for the management of postoperative paralytic ileus, this should begin before surgery2 with measures that tend to reduce operative stress, such as the use of minimally invasive techniques when possible and the use of epidural analgesia. Kehlet et al.18 described fast-track surgery based on the affirmation that reducing postoperative stress helps the patient with faster recovery, more comfort and well-being, and shorter hospital stay. In addition to taking into account the previously described factors, patients should be properly informed of all the possible postoperative complications, correct fluid therapy should be used, oral tolerance and mobilization should be initiated early on (always preferring enteral over parenteral nutrition)19 and pain should be properly controlled, while trying to minimize the use of opiates due to their astringent effect. These measures have been shown to reduce hospital stays and costs of postoperative patients and to reduce postoperative morbidity, without affecting readmission or mortality rates.20,21 However, there are still no clear data about the effectiveness of these actions in minimally invasive surgery,20 so new studies in this direction are necessary.
Currently, new drugs are being researched, and the results are promising. Alvimopan, an opioid receptor antagonist that acts at the intestinal level, has demonstrated in several clinical trials21–24 a reduction in the incidence of postoperative paralytic ileus, costs22 and hospital stay, without affecting morbidity and mortality. Methylnaltrexone, another opioid antagonist, has presented contradictory results, but it has also been demonstrated to be a safe drug, without major postoperative complications.25 Likewise, some simple and inexpensive measures have been shown to be useful, such as the use of chewing gum and drinking coffee at the initiation of oral tolerance, which could help in the early initiation of intestinal motility.
Use of CoffeeThe prokinetic effect of coffee is widely known. Since the 1990s, there have been studies26,27 proposing coffee as a treatment for constipation, even in surveys conducted in the general population.26 However, there are currently few reports in the literature about the use of coffee to induce postoperative peristalsis. Only 2 randomized clinical trials were found in the databases used in our search.
The first study published specifically about the subject28 is an open, multi-center, randomized clinical trial that randomized the use of coffee in 80 patients who had undergone open or laparoscopic hemicolectomy: 40 patients were given water and 40 caffeinated coffee. In the patients who had consumed coffee, the first bowel movement was significantly earlier than in patients who had only drunk water (60h vs 74h). Nonetheless, the authors found no significant differences in time to oral tolerance or hospital stay, nor did they analyze whether the effect of the coffee was due to the caffeine or other components. This factor was recommended for study in further research.
In the most recent study,29 the authors took note of the observation by Müller and conducted a prospective study at a single center that randomized a relatively small sample (105 patients), who had been treated laparoscopically for left colon tumors, into 3 different study arms: one treated with water alone, another with decaffeinated coffee, and the third with caffeinated coffee. The group that consumed decaffeinated coffee had a shorter time until the first bowel movement than the group that ingested coffee with caffeine and the water group (3 vs 3.75 vs 4.14 days, respectively). Time until the tolerance of solid food was also shorter in the decaffeinated coffee group (1.85 vs 2.60 vs 2.80 days). Therefore, the hypothesis that a coffee component other than caffeine has an effect starts to gain strength, although new studies (preferably randomized clinical trials) should be done to confirm this finding.
Use of Chewing GumIn the last decade, it has been hypothesized that chewing gum could have an activation effect on peristaltic waves and thereby prevent postoperative ileus. Several systematic reviews have been published with meta-analyses of randomized clinical trials,30–32 but their results were inconclusive due to the disparity observed in the results, the heterogeneity of the studies and their low quality.
The most recent systematic review, and one that probably has had the greatest impact, was published by Short et al. in 2015 for the Cochrane Database Systematic Review,30 which identified and analyzed 81 studies that were exclusively about colorectal surgery and cesarean sections. This review demonstrated that there was statistical evidence that chewing gum shortens the time until passing of gas (mean 10.4h), time until bowel movement (12.7h), and hospital stay (only 0.7 days). Nonetheless, all these studies are heterogeneous and most are low-quality, small trials; also, most of them applied the previously mentioned fast-track postoperative protocol, which may be a confounding factor. Thus, the author concluded that new larger randomized clinical trials are necessary, which consider the rapid recovery protocol as an independent factor and analyze the role of chewing gum in the post-op of other types of surgery, such as upper gastrointestinal tract or trauma surgery.
Other recent systematic reviews and meta-analyses, such as those by Su’a et al.31 or Li et al.,32 have similar conclusions: current studies show heterogeneity to be comparable; the early initiation of oral tolerance can disguise the effect of the chewing gum; and, there are no conclusive results about the effectiveness of chewing gum in laparoscopic surgery. Therefore, they insisted on the need for higher quality studies.
As these reviews have already stated, current clinical trials show disparity in the results obtained, while also being focused on colorectal and gynecological surgery. Only Andersson et al.33 have studied the effect of gum on pancreatic surgery, without being able to demonstrate conclusive results and stating the need for studies in other types of surgeries. In other trials about the usefulness of chewing for recovery after colorectal surgery,34,35 there are no statistically significant differences between the chewing gum group and the control group. Furthermore, they reported possible negative effects, such as burping and indigestion, which, while not major complications, can cause patient discomfort.
The results shown by van den Heijkant et al.36 are very interesting. In addition to studying the effect of chewing gum in the post-op of colorectal surgery, they measured inflammatory factors, such as IL-6, IL-8 and TNFRSF1A, and found statistically significant differences between the gum and control groups, with lower levels in the former. These results indicate that one of the mechanisms of action of chewing gum is that it reduces bowel wall inflammation, and motility is consequently restored.
It is currently accepted that the possible mechanism of action of chewing gum is multifactorial. Reportedly, the most important process is the action of chewing itself, which causes cephalic-vagal stimulation, producing hormones that activate intestinal motility, the production of saliva and pancreatic juices. Tandeter37 hypothesizes that some sweeteners in sugar-free gum, including hexitols (sorbitol, mannitol, maltitol and xylitol), can also have a direct effect on the gastrointestinal tract by activating it and improving motility. However, there are no related clinical trials. Thus, in order to demonstrate this theory, studies must be designed to compare post-op patients who use chewing gum with and without hexitols.
Use of gastrograffinGastrografin® (diatrizoate meglumine and diatrizoate sodium) is a radiological contrast medium used in the past for radiological studies of the colon, gastrointestinal tract in general and for computed tomography studies of the digestive tract, which is currently its main use. The compound is able to remain stable for at least 30 days at 25°C with 60% humidity and in a setting without light.38 It is a known hyperosmotic agent,2,39 so it could theoretically assist in the resolution of obstructive and pseudo-obstructive symptoms as the wall edema is reabsorbed due to the increased intraluminal osmotic pressure.
There are several clinical trials40,41 and systematic reviews with meta-analyses42,43 that demonstrate the utility of gastrograffin in the management of adhesion-related bowel obstruction by reducing the resolution time of symptoms, hospitalization and surgical indication. In 2008, Di Saverio et al.40 published a multi-center randomized trial with 76 patients, in which they found significant differences in the symptom resolution time (6.4 vs 43h with gastrograffin; P<.01) and hospitalization time (7.8 vs 4.7 days with gastrograffin; P<.05). Similar results were found in 2013 by Mora López et al.,41 who applied the protocol for use of this agent in 170 episodes of bowel obstruction and demonstrated a reduction in hospitalization from 5.5 to 2 days and a reduction in surgical indication time. The systematic reviews confirm the veracity of these findings: a review of prospective studies and clinical trials done for the Cochrane Database of Systematic Reviews42 reported that the appearance of contrast medium in the colon in a simple abdominal radiograph within the first 24h of its administration has a sensitivity to rule out surgery of 0.97 and a specificity of 0.96. It also reduces hospital stay by 1.83 days. However, its use does not reduce the need for surgery, so its therapeutic value in the resolution of symptoms is limited.
The most current systematic review dates from January 201643 and includes 21 studies in the meta-analysis. This article, in addition to confirming the former data, reports that gastrograffin also reduces the need for surgery (odds ratio 0.55; P=.003), which could demonstrate its therapeutic role. Nonetheless, the authors warn that only one of these articles is considered good quality, so additional studies are still necessary for verification.
Due to these findings, it was suggested that gastrograffin could also play an important role in the management of functional obstruction symptoms (paralytic ileus), especially in the postoperative period. In 1985,44 a test was conducted in a series of 47 patients with general and gynecological surgery, and faster resolution of ileus was found in those patients who had been administered water soluble contrast medium. Nevertheless, there are currently very few related studies, and almost all referred to colorectal and gynecological surgery. Chen et al.39 had very promising results in their randomized clinical trial in the post-op after colorectal surgery, which found significant differences in the initiation time of oral tolerance (3.3 days with gastrograffin, vs 4.8 days in the control group) and hospitalization time (7.6 vs 10.2 days). However, in better quality studies9,45 also in the post-op of colorectal surgery, no significant differences were found in the parameters studied (resolution time, need for a nasogastric tube, initiation of oral tolerance and hospital stay). Only Vather et al.9 found differences in the resolution time for abdominal distension (52.8 vs 77.7h) and in time until bowel movement (18.9 vs 32.7h). Both studies conclude that the related evidence is very limited and emphasize the need for better designed clinical trials for clarification.
ConclusionsAfter analyzing these studies, it is clear that there is limited scientific evidence about the usefulness of coffee and gastrograffin to prevent and treat postoperative ileus. More articles have been published regarding chewing gum, including several reviews with meta-analyses. However, they all come to the same conclusion: the existing studies are heterogeneous, show disparate results and are only focused on the postoperative period after colorectal and gynecological surgery. Therefore, we coincide with current reviews about this subject and emphasize the need for new high-quality studies, preferably randomized clinical trials, that compare and clarify the usefulness of these measures.
FundingThe authors have received no financial assistance for the completion of this article.
Authorship/CollaboratorsFlores-Funes D: Study design, data collection, analysis and interpretation of the results, composition of the article.
Campillo-Soto A: Analysis and interpretation of the results, critical review.
Pellicer-Franco E: Analysis and interpretation of the results, critical review.
Aguayo-Albasini JL: Critical review, approval of final version.
Conflict of InterestsThe authors have no conflict of interests regarding the content of this article.
Please cite this article as: Flores-Funes D, Campillo-Soto Á, Pellicer-Franco E, Aguayo-Albasini JL. Uso de café, chicle y gastrografín en el manejo del íleo postoperatorio: revisión de la evidencia actual. Cir Esp. 2016;94:495–501.