Laparoscopic ventral hernia repair is in full development with the appearance of surgical techniques that try to diminish the disadvantages associated with this procedure. Totally endoscopic subcutaneous ventral hernia surgery with suprapubic access is a new minimally invasive surgical technique that surgically corrects the hernia defect associated or not with diastasis recti, with the advantages of not penetrating the intra-abdominal space and avoiding the prosthesis placement in contact with the viscera, with the consequent complications derived from it (appearance of adhesions or fistulas).
El abordaje mínimamente invasivo de la hernia ventral se encuentra en pleno desarrollo con la aparición de técnicas quirúrgicas que intentan disminuir las críticas asociadas al abordaje laparoscópico tradicional. La cirugía totalmente endoscópica subcutánea de acceso suprapúbico de la hernia ventral es una nueva técnica quirúrgica mínimamente invasiva que corrige quirúrgicamente el defecto herniario asociado o no a diástasis de rectos, con las ventajas de no penetrar en el espacio intraabdominal y evitando la colocación de la prótesis en contacto con las vísceras, con las consiguientes complicaciones derivadas de ello (aparición de adherencias o fístulas).
The laparoscopic approach of ventral hernias is associated with a series of advantages over conventional open surgery, including shorter hospital stay, lower incidence of surgical site infection and hemorrhagic events.1 In recent years, prospective studies have demonstrated that, in cases of coexisting midline ventral hernia and diastasis recti, the correction of both entities is recommended. If only the hernia defect is repaired, the hernioplasty is performed on an anatomically weak area (diastasis recti), and there is a greater probability of hernia recurrence in the mid to long term.2
This article describes a new minimally invasive surgical technique for midline hernia repair, which provides for simultaneous correction of associated diastasis recti in cases of its existence. We have come to call this technique Full Endoscopic Suprapubic Subcutaneous Access (FESSA).
Surgical TechniqueThis technique is indicated in patients diagnosed with primary ventral or midline incisional hernia smaller than 10 cm in transverse diameter, with or without associated diastasis recti. Midline hernias can be repaired at any location, regardless of their distance to the pubis. An inter-recti distance of 2 cm or less associated with the hernia is not considered pathological and, therefore, does not require surgical correction.3
The patient is placed supine with the lower limbs in abduction. The surgeon stands between the legs and the assistant on the patient’s left side.
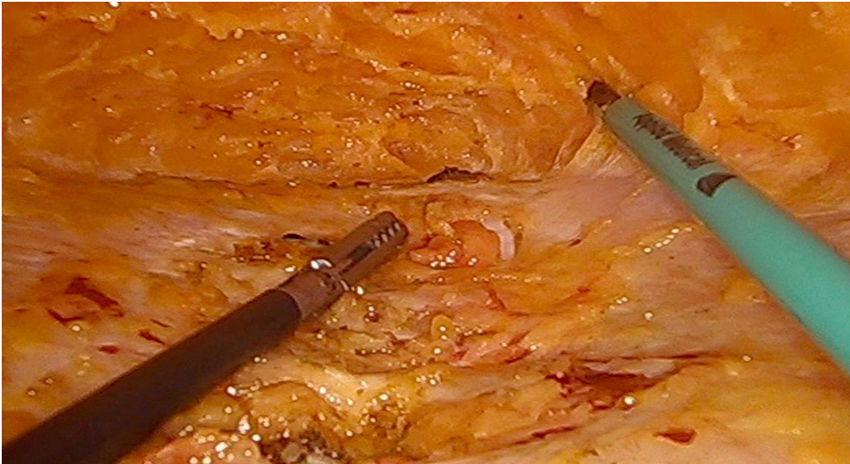
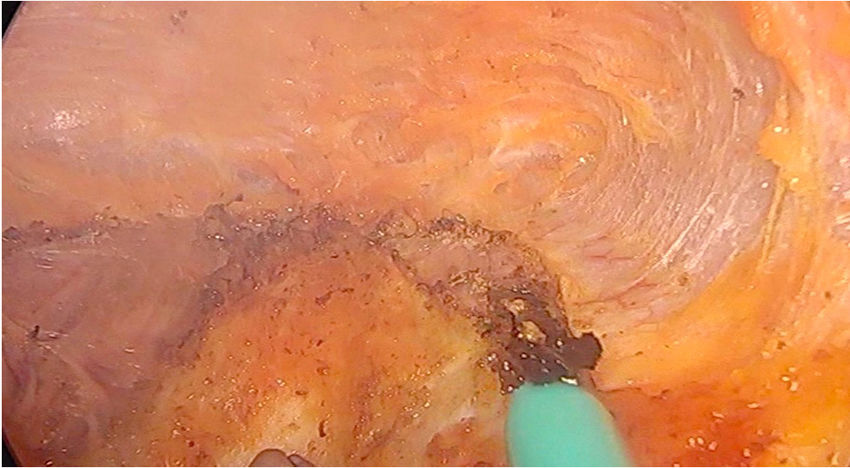
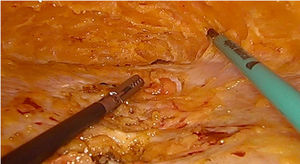
After a 2 cm long incision is made in the suprapubic region, the supra-aponeurotic space is dissected bluntly immediately above the pubis. Afterwards, a 10-mm trocar is placed through said incision with two 5-mm trocars on each side, separated by a distance of 5−6 cm between them (Fig. 1). Using a working pressure of 8 mmHg, the supra-aponeurotic space is dissected subcutaneously using cautery scissors, exposing the linea alba. Once the hernia sac is identified, it is released and reduced to the intra-abdominal space. The base of the navel is de-inserted, followed by the dissection of the linea alba cranially to the subxiphoid region if the patient presents associated supraumbilical diastasis recti greater than 2 cm wide. The dissection should reach 3−5 cm laterally over each medial edge of the anterior sheath of both recti muscles (Fig. 2).
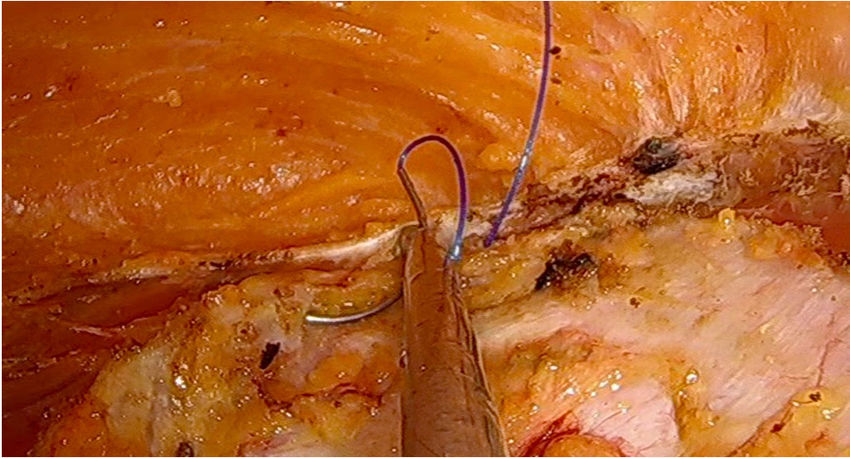
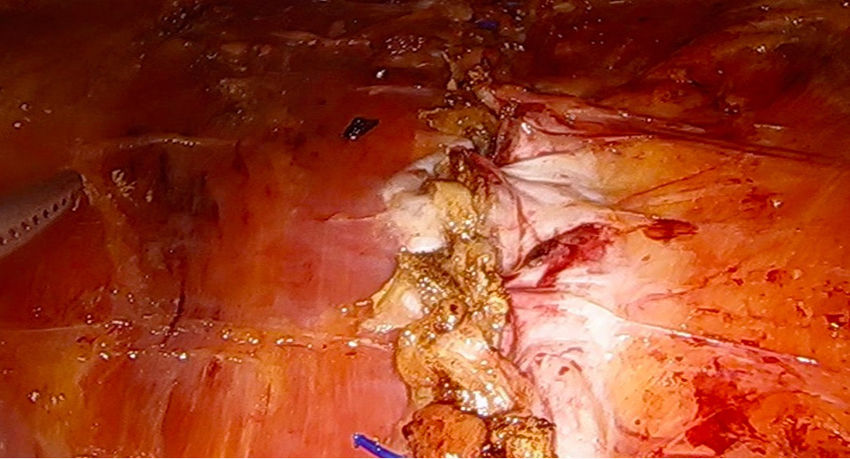
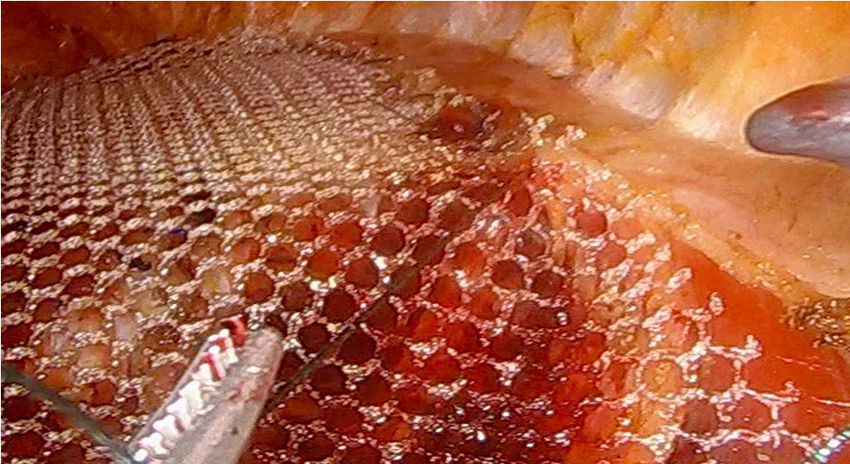
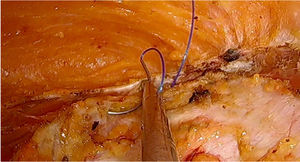
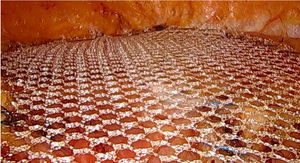
Next, an incision is made in the anterior sheath of both rectus abdominis muscles along the entire defect and the diastasis, about 2−3 cm laterally to the medial edge of the hernia orifice and at the same distance from the medial edge of the fascia of the diastatic area (Fig. 3). For defects measuring 9 cm in transverse diameter, the incision is made about 4−5 cm from the medial margin of the defect for tension-free closure.4 Both medial edges of the opening of the aponeurosis are sutured on the midline with 2/0 barbed suture (V-Loc™, Medtronic, Madrid, Spain) to cover the defect and diastasis without tension, reconstructing the midline (Figs. 4 and 5). Low-density polypropylene mesh (48 g/m2) with a wide pore (3.6 × 2.8 mm) (Optilene Mesh elastic®, B. Braun Surgical, Rubí, Barcelona) are inserted in the onlay position and sutured to the outer edge of the opening of the recti sheaths using continuous 2/0 barbed suture (Figs. 6 and 7). The surgery is finished with the re-insertion of the navel in its original position with 2/0 suture to the midline and the placement of a suction drain.
ResultsBetween October 2017 and May 2018, 8 patients diagnosed with primary abdominal hernia (5 patients with umbilical hernia and 3 patients with epigastric hernia) and 6 patients affected with symptomatic midline incisional hernia (M3W1 and M3W2) were treated with this approach. Eight patients (57%) presented diastasis recti associated with the hernia defect (5 with umbilical hernia, one epigastric hernia and 2 incisional hernias M3W1). The average body mass index (BMI) was 24 kg/m2.
The mean area of the hernia defect was 36 cm2, with a mean width of 5 cm. The average width of the repaired diastasis was 4 cm. The average area of the mesh used was 144 cm2. Mean operative time was 76 min, and mean hospital stay was 1.8 days. The average time before drain tube withdrawal was 5.3 days (done when the discharge was less than 10 cc in 24 h). Seroma was detected in 3 patients (21%), 2 treated for umbilical hernia with diastasis recti and one patient treated for an incisional hernia (M3W2) also associated with diastasis recti. All seromas were type I of the Morales-Conde classification,5 so they required no treatment and were not considered a complication, as established by this classification. We observed no surgical site infections and no cases of postoperative cutaneous necrosis in our patients.
Clinical follow-up was conducted after 1, 6, 12 and 24 months, and a CT scan of the abdomen was performed in all patients at the 12-month office visit for radiological follow-up of the abdominal wall. With a mean follow-up of 12 months, no clinical or radiological recurrence was observed in the 14 patients included.
DiscussionUntil a few years ago, the only surgical approaches for midline hernias associated or not with diastasis recti were open and laparoscopic surgery. Currently, new surgical techniques have appeared that are being developed, as is the case of the minimally invasive subcutaneous approach.
The totally endoscopic subcutaneous approach of ventral hernias is based on the supra-aponeurotic access first published in 1998 by Champault6 using intracorporeal or transfascial sutures. Subsequently, different articles appeared in the literature using the same approach in combination with abdominoplasty or mini-abdominoplasty, without the use of gas.7
The first published technique in which the minimally invasive suprapubic access was used by means of 3-trocars with CO2 at 8 mmHg was published in 2015 by our group.8 This technique was designed for the endoscopic surgical treatment of diastasis recti with associated midline hernia defects. Subsequently, and based on this approach, different techniques have appeared designed to also perform a correction of the diastasis and associated hernias. These techniques perform endoscopic plication of both anterior sheaths of the recti muscles with subsequent mesh placement in the supra-aponeurotic position,9,10 thereby generating tension in the midline due to the performance of said plication, with the consequent probability of greater postoperative pain and long-term recurrence.
As an alternative to these techniques, MILOS11 and ELAR12 are hybrid techniques also used for the joint correction of wall hernias and diastasis recti, which require a 6−7 cm peri-supraumbilical incision, with an open phase and later endoscopic phase.
The FESSA technique is a new, fully endoscopic surgical technique with suprapubic access that is based on the open techniques previously described by several authors, such as Rehn13 or Chevrel,14 in which a midline division and suture of the anterior sheath of the recti is done with subsequent onlay mesh placement, which is sutured to the outer edge of the division line of both sheaths. This new technique follows the same steps as open techniques but uses a minimally invasive supra-aponeurotic suprapubic approach. The MILAR15 technique is similar, with division of the anterior sheath of the rectus muscle, but using open access, flexible retractors with light.
This access has a number of advantages:
- •
Aesthetic results are better than with periumbilical techniques (MILOS and ELAR) or the open MILAR technique, especially in ventral hernias. Three small suprapubic incisions are sufficient to perform the technique, which become unnoticeable after a few months.
- •
This technique causes no tension on the midline. The division and midline suture of both medial margins of the anterior recti muscle sheaths restore them to their normal anatomical position, thereby reconstructing the linea alba without tension.12
- •
It potentially reduces the rate of wound complications. Since it is a totally endoscopic technique, the probability of wound superinfection is low compared to open or mixed techniques.
- •
The prosthesis is placed outside the intraperitoneal compartment. This endoscopic technique combines the advantages of being a minimally invasive approach with those derived from the placement of an extraperitoneal mesh, avoiding the contact of intra-abdominal viscera with the mesh and the resulting risk of adhesions or fistulae that may appear in the classic laparoscopic IPOM technique.
The main problem that could be associated with this technique is seroma due to the extensive subcutaneous dissection that is carried out. This appears in 21% of patients in our series, although all type I, so it is not a complication for the patient. To reduce its incidence, the use of an abdominal girdle and the maintenance of the suction drain until the discharge is less than 10 cc appear to be effective.
Likewise, a BMI > 30 kg/m2 is an additional difficulty for performing this technique, especially in patients with a large abdominal fat pad, due to the complexity in the identification and dissection of the supra-aponeurotic plane.
FundingThe authors have received no funding for the completion of this article.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bellido Luque J, Bellido Luque A, Tejada Gómez A, Morales-Conde S. Abordaje totalmente endoscópico suprapúbico de la hernia ventral. Ventajas de un nuevo procedimiento mínimamente invasivo. Cir Esp. 2020;98:92–95.