Breast surgery is a key part of training and competency in general surgery in Spain and is a “frontier area” that can be efficiently managed by general surgeons and gynecologists. The main objective of the training process consists of the surgical treatment of breast cancer, including conservative surgery, oncoplastic and reconstructive techniques.
This article analyses the current status of breast surgery training in Spain and schematically proposes potential targets of the different training programs, to improve access and training for surgeons and residents in this area, taking into account the RD 639/2014 and European regulation. The priority is to specify the level of training that should be achieved, in relation to the group of professionals involved, considering their area of competency: surgery resident, educational programs, and surgeons with special dedication to this area.
La cirugía de la mama forma parte fundamental en la formación y competencia de la cirugía general en España, constituyendo un «área frontera» asumida eficientemente por cirujanos y ginecólogos. El objetivo fundamental del proceso formativo está constituido por el tratamiento quirúrgico del cáncer de mama, que incluye la cirugía conservadora y las técnicas oncoplásticas y reconstructivas.
En este artículo, se realiza un análisis de la situación actual de la formación en cirugía mamaria en nuestro país y se plantean esquemáticamente los posibles objetivos de los diversos programas formativos, para optimizar el acceso y la capacitación de los residentes y cirujanos en esta área teniendo en cuenta el RD 639/2014 y la normativa europea. Resulta prioritario concretar el nivel de formación que se pretende alcanzar, en relación con el grupo de profesionales a quien va dirigido, teniendo en cuenta su ámbito competencial: residente de cirugía, formación continuada y especial dedicación a esta área.
Breast surgery is part of the classical training nucleus and skill set of general and gastrointestinal surgeons, together with endocrine, abdominal wall, esophagogastric, hepatobiliary–pancreatic and colorectal surgery. It involves surgical treatment of both benign as well as malignant breast pathologies.
Currently, several important aspects involved in this type of surgery must also be considered:
- 1.
Surgical treatment of breast pathologies has become fully incorporated into the “portfolio of services” and training spectrum of Obstetrics and Gynecology.
- 2.
The increasing use of reconstructive surgical techniques after mastectomy and oncoplastic surgery involved in breast-conserving surgery has justified the involvement of Plastic Surgery in these areas. This often promotes efficient surgical synergies and teamwork, although occasionally conflicts do arise.
- 3.
The fundamental nucleus of this pathology involves the treatment of breast cancer, aspects of its clinical diagnosis, early diagnosis (from screening programs) and prophylactic surgery (hereditary cancer, genetic counseling).
- 4.
This type of surgery, which is currently a frontier in our specialty, is currently being performed most often by general surgeons and gynecologists in the surgical setting of regional, general or reference hospitals as well as teaching oncology hospitals, whether or not they are equipped with specific “organic” or “functional” breast surgery units. Therapeutic decisions are established by multidisciplinary breast tumor committees in all cases following protocols.
In fact, in our country, there are still very few hospitals that have certified breast treatment units. In 2003, a survey was published about the surgical departments of 241 Spanish hospitals in order to confirm the existence of functional breast treatment units in Spain, and the involvement of the surgery departments. The response rate was 68% (164 responses), and it was observed that breast cancer treatment was coordinated by general surgeons in most hospitals (n=131) and in association with gynecologists in 51 cases. Structured, functional breast treatment units had been created in 82 hospitals.1
- 5.
In recent years, significant modifications have taken place in the surgical treatment of breast cancer, fundamentally with the application and proposition of oncoplastic and reconstructive breast procedures whose main objective has been to improve the quality of breast-conserving surgery and immediate breast reconstruction. These changes have been led by a fair number of surgical specialists (surgeons or gynecologists) who have decidedly become involved in obtaining specific certified training in breast reconstruction and remodeling, with optimal results.
Breast-conserving surgery and oncoplastic/reconstructive techniques are currently part of the therapeutic arsenal and current portfolio of services in the treatment of patients with malignant breast pathologies. The designation of the medical professionals responsible for performing oncoplastic and reconstructive procedures should be an agreed decision based on the services available, training and the history of the institution itself. It is also necessary to continuously promote training in these procedures to guarantee their use in the highest number possible of patients.
- 6.
The countries of the European Union face similar challenges when offering appropriate, high-quality treatment to oncological patients. In their extensive review, Merck et al.,2 described the different approaches to multidisciplinary treatment of breast disease in certain European countries (United Kingdom, Sweden, Italy, France or Spain) and concluded that they are basically systematized into two unit models: the first is a functional unit, proposed by EUSOMA, and the second could be included within the concept of oncology institutes.
Therefore, and given the organizational diversity within the healthcare system in Spain, common European guidelines would be beneficial in order to harmonize and improve the surgical/therapeutic process in this pathology.
In this situation, we have proposed conducting an analysis (or, better put, a “snapshot”) of the current situation of breast surgery training in Spain, without any intention of dogmatizing or developing a specific training model. The proposition, establishment and suitability of such a training model should be the responsibility of official institutions and specific scientific societies.
In general, it is necessary to consider several different levels of surgical training in this area, given the scope that it involves: (1) General Surgery and Gastrointestinal Surgery residents; (2) maintaining specialists involved in breast pathology treatment, and their skills, up to date (continuing education and professional development); and, (3) guidelines and requirements for access to and achievement of specialized diplomas (fellow) in breast surgery for specialists integrated in specific breast units who are dedicated to this area of surgery.
Current training of residents in SpainSpecialized training in general and surgical training in particular are both based on the MIR training system and proper coordination of its three pillars: the training program, certified training units, and tutors. The MIR process is an efficient educational program that is able to transform medical graduates into specialists, with similar learning outcomes regardless of the place of residency. Afterwards, specialized training can be completed in a specific area, such as breast surgery, in accordance with the specifications of the program itself and the Law for Healthcare Professions.3
In our country, breast surgery is conducted efficiently and safely in both general surgery departments without structured functional units as well as those that do have such units, whether or not there is an “accredited” breast surgery unit.
Breast surgery is a fundamental aspect in general and specialized surgical training for two basic reasons: first of all, due to the frequency of this pathology; and, secondly, due to the accessibility and systematization of this anatomical area, together with techniques that entail a medium level of complexity, which provide for optimal learning, progression and later autonomous or tutored reproduction of these techniques.
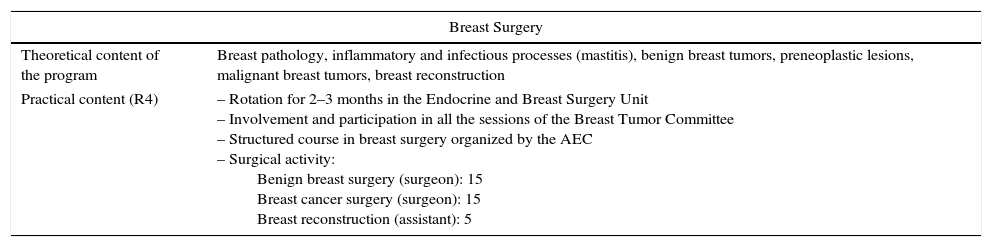
The training objectives of the specialty program5 (Table 1) are similar to those of the European Board of Surgery.4 Regarding breast surgery, the program requires a series of theoretical knowledge that residents should acquire during training: breast pathologies, inflammatory and infectious processes (mastitis), benign breast tumors, preneoplastic lesions, malignant breast tumors and breast reconstruction.
Program for the General and Gastrointestinal Surgery Specialty (2007).
| Breast Surgery | |
|---|---|
| Theoretical content of the program | Breast pathology, inflammatory and infectious processes (mastitis), benign breast tumors, preneoplastic lesions, malignant breast tumors, breast reconstruction |
| Practical content (R4) | – Rotation for 2–3 months in the Endocrine and Breast Surgery Unit – Involvement and participation in all the sessions of the Breast Tumor Committee – Structured course in breast surgery organized by the AEC – Surgical activity: Benign breast surgery (surgeon): 15 Breast cancer surgery (surgeon): 15 Breast reconstruction (assistant): 5 |
Source: BOE no. 110.4
In this context, and referring to the results observed in surgical training, the program dictates the minimum number of surgeries that residents should perform during training: 15 benign breast surgeries and 15 breast cancer surgeries.4
According to the content of the training program, it is not until the 4th year of MIR training when residents begin training in breast pathologies and surgery, with a rotation in a specific breast surgery unit for 2–3 months. And although in general surgical training the activity of residents in breast surgery seems to be done adequately, with a mean of between 29 and 25 surgical interventions of each type,5 it would be more desirable for training in this area to be initiated earlier on and within different areas of the training itinerary.
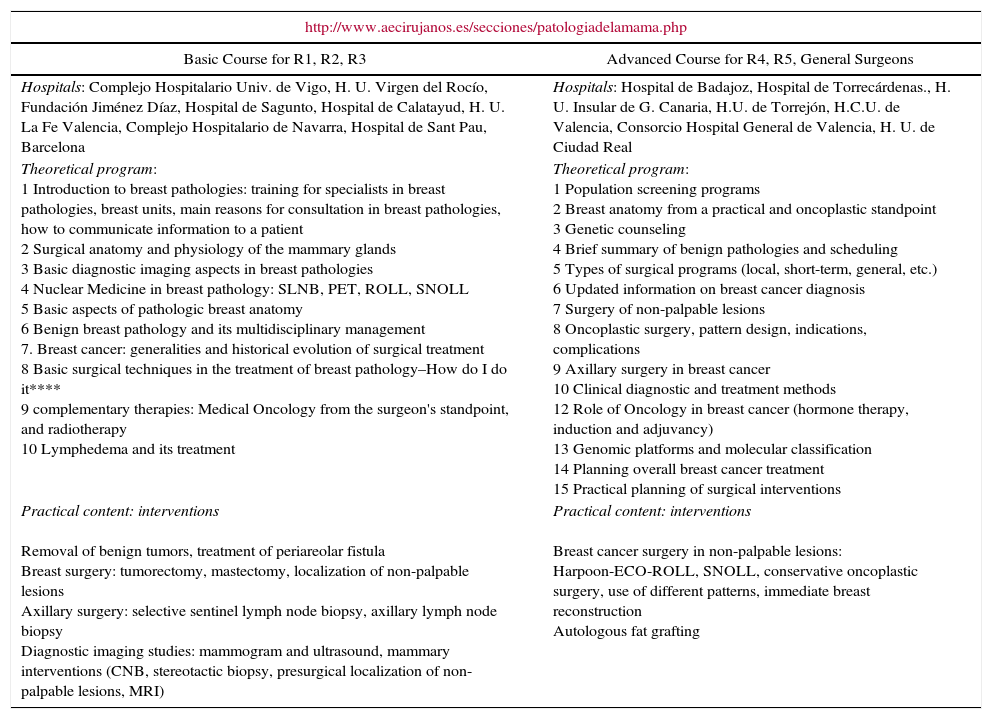
The program also contemplates completing at least one accredited breast surgery course, such as those proposed by the Breast Pathology Section of the Spanish Association of Surgeons (Association Española de Cirujanos, or AEC) (http://www.aecirujanos.es/secciones/patología de la mama.php/, both basic and advanced). Table 2 shows the sites, objectives and programs of these courses.
Courses Organized by the Spanish Association of Surgeons, Breast Pathology Section.
| http://www.aecirujanos.es/secciones/patologiadelamama.php | |
|---|---|
| Basic Course for R1, R2, R3 | Advanced Course for R4, R5, General Surgeons |
| Hospitals: Complejo Hospitalario Univ. de Vigo, H. U. Virgen del Rocío, Fundación Jiménez Díaz, Hospital de Sagunto, Hospital de Calatayud, H. U. La Fe Valencia, Complejo Hospitalario de Navarra, Hospital de Sant Pau, Barcelona | Hospitals: Hospital de Badajoz, Hospital de Torrecárdenas., H. U. Insular de G. Canaria, H.U. de Torrejón, H.C.U. de Valencia, Consorcio Hospital General de Valencia, H. U. de Ciudad Real |
| Theoretical program: 1 Introduction to breast pathologies: training for specialists in breast pathologies, breast units, main reasons for consultation in breast pathologies, how to communicate information to a patient 2 Surgical anatomy and physiology of the mammary glands 3 Basic diagnostic imaging aspects in breast pathologies 4 Nuclear Medicine in breast pathology: SLNB, PET, ROLL, SNOLL 5 Basic aspects of pathologic breast anatomy 6 Benign breast pathology and its multidisciplinary management 7. Breast cancer: generalities and historical evolution of surgical treatment 8 Basic surgical techniques in the treatment of breast pathology–How do I do it**** 9 complementary therapies: Medical Oncology from the surgeon's standpoint, and radiotherapy 10 Lymphedema and its treatment | Theoretical program: 1 Population screening programs 2 Breast anatomy from a practical and oncoplastic standpoint 3 Genetic counseling 4 Brief summary of benign pathologies and scheduling 5 Types of surgical programs (local, short-term, general, etc.) 6 Updated information on breast cancer diagnosis 7 Surgery of non-palpable lesions 8 Oncoplastic surgery, pattern design, indications, complications 9 Axillary surgery in breast cancer 10 Clinical diagnostic and treatment methods 12 Role of Oncology in breast cancer (hormone therapy, induction and adjuvancy) 13 Genomic platforms and molecular classification 14 Planning overall breast cancer treatment 15 Practical planning of surgical interventions |
| Practical content: interventions Removal of benign tumors, treatment of periareolar fistula Breast surgery: tumorectomy, mastectomy, localization of non-palpable lesions Axillary surgery: selective sentinel lymph node biopsy, axillary lymph node biopsy Diagnostic imaging studies: mammogram and ultrasound, mammary interventions (CNB, stereotactic biopsy, presurgical localization of non-palpable lesions, MRI) | Practical content: interventions Breast cancer surgery in non-palpable lesions: Harpoon-ECO-ROLL, SNOLL, conservative oncoplastic surgery, use of different patterns, immediate breast reconstruction Autologous fat grafting |
CNB, core needle biopsy; SLNB, sentinel lymph node biopsy; PET, positron emission tomography; MRI, magnetic resonance imaging; ROLL, radioguided occult lesion localization; SNOLL, sentinel node and occult lesion localization.
Meanwhile, certain surgical procedures in major ambulatory surgery programs, such as benign breast pathologies, harpoon-guided biopsies, selective sentinel lymph node biopsies, and some types of oncoplastic surgeries, are not systematically included in the current official program. However, they would be beneficial to the training process, even in light of the technical, organizational and educational implications involved in this “healthcare circuit”.
Thus, while taking into account that patients are usually selected and the programs standardized, possibly the structured participation of residents in these programs and techniques (apart from specific rotations) would possibly be one of the most appropriate aspects that is still pending in breast surgery training.
However, in many occasions, the performance, learning process and perfecting of more specialized oncoplastic techniques by the staff, at different points of the learning curve, in specific breast surgery units or in departments or units with important involvement in this type of surgery, could temporarily displace residents or those from other departments or units to learn these techniques.
The recently published Royal Decree for Core Requirements and Specific Training Areas (STA)6 will result in a drastic modification of the training program for the specialty of General and Gastrointestinal Surgery.7 It is therefore a transcendental moment for the AEC and its Breast Pathology Section to take a stand and to propose and promote specific modifications to the new General and Gastrointestinal Surgery program.
Maintaining Specialists’ Training up to DateAlthough the current training program specifies among its objectives “to initiate complementary training in some areas according to the circumstances of each resident and hospital”, the final result is that of a Specialist in General and Gastrointestinal Surgery who should be able to demonstrate specific clinical and surgical competence.
According to the Spanish Law for Healthcare Professions,8 maintained professional competence and continuous training refers to the permanent process of teaching and active learning that is initiated upon finalizing the specialization period. It is aimed at updating and improving the knowledge, skills and approaches of healthcare professionals given the constant evolution of science, technology, requirements and needs, both for society as well as for the healthcare system itself. Medical professionals have the right and obligation to participate in this training, regardless of their status, years of work or setting in which they carry out their clinical/hospital activity.
With regard to breast pathologies, it is essential that adequate means be available in order to obtain, maintain and/or perfect skills in this area of practice, for surgical specialists in general or for those especially involved in this pathology, whether or not they work in specific units.
Currently, the development of breast surgery training criteria for general surgeons (or gynecologists), in our country as well as in Europe, where there is no specific specialty, can be defined by Syllabus 2014 of the UEMS (www.uems.net), which specifies the training and curricular requirement for obtaining specific certification (BOARD) in the area of specialization (Fellow of European Board of Surgery (FEBS)/Breast Surgery), as well as the criteria proposed by the European Society of Mastology (EUSOMA),9 which would define the requirements of the surgical specialists involved in breast units and would generally be as follows: (a) knowledge and treatment of benign and malignant breast pathologies; (b) capacity to perform at least 40 surgical interventions of the breast; (c) dedication of at least 50% of the work week to aspects related with breast pathologies; (d) capacity to perform basic breast construction techniques and oncoplasty.10
The different methods for meeting these criteria, which would be complementary in many cases, would include:
- 1.
Specific courses, such as the advanced level courses proposed by the Breast Pathology Section of the AEC (http://www.aecirujanos.es/secciones/patologiadelamama.php) and/or the most specialized oncoplastic surgery courses at different reference hospitals (http://www.aecima.com)
- 2.
A master's degree or expert diploma obtained from an accredited university or institute
- 3.
Official assignation to a specific breast surgery unit, preferably accredited, in accordance with the recommendations of EUSOMA5 or the Spanish Society of Senology and Breast Pathologies (http://www.sespm.es/unidades/)
- 4.
Integration in a specific unit or special dedication in a surgery department
- 5.
Regular assistance to and participation at medical conferences, symposiums, national and international meetings organized by scientific societies and entities: Spanish Society of Surgeons (http://www.aecirujanos.es/secciones/patologiadelamama.php), Spanish Society of Senology and breast Pathologies (http://www.sespm.es/), Spanish Society of Breast Surgeons (http://www.aecima.com/).
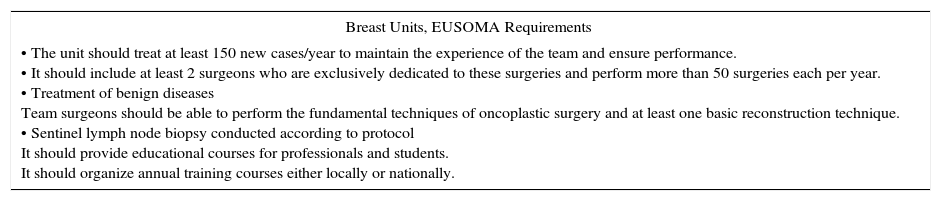
In many instances, it is a justification of the requirements proposed by EUSOMA regarding the minimum criteria required for surgery and the accreditation of specialized units9 (Table 3).
EUSOMA Requirements: Minimal Criteria in the Surgical Setting.
| Breast Units, EUSOMA Requirements |
|---|
| • The unit should treat at least 150 new cases/year to maintain the experience of the team and ensure performance. • It should include at least 2 surgeons who are exclusively dedicated to these surgeries and perform more than 50 surgeries each per year. • Treatment of benign diseases Team surgeons should be able to perform the fundamental techniques of oncoplastic surgery and at least one basic reconstruction technique. • Sentinel lymph node biopsy conducted according to protocol It should provide educational courses for professionals and students. It should organize annual training courses either locally or nationally. |
Source: BOE no. 190.7
One fundamental aspect in the specific preparation of surgeons in oncological breast surgery should refer to conventional oncoplastic surgery and basic reconstructive surgery using expanders or prostheses in subcutaneous, total and “skin-saving” mastectomies. Conventional techniques and more complex breast reconstruction could be general skills acquired by plastic surgeons. This would allow for increased indications of breast preservation with adequate control of the process, and good esthetic results could be achieved to reduce the psychological impact of the disease.
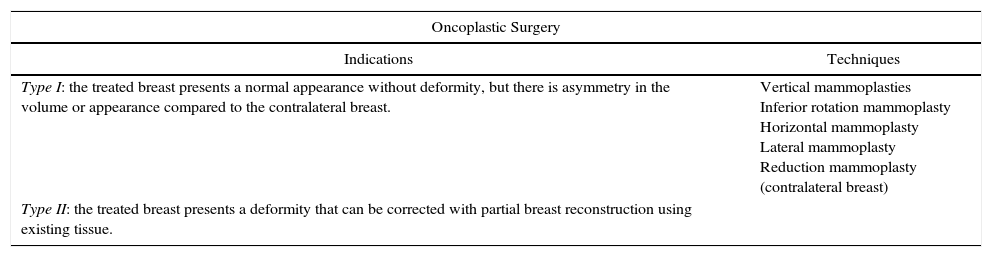
Competence in these oncoplastic techniques will comprise the following aspects: appropriate oncological techniques for the removal of the tumor; immediate remodeling of the resulting defect/deformity; repositioning of the nipple–areolar complex and correction of the asymmetry of the contralateral breast.11 Indications and techniques are presented in Table 4.12
Indications and general techniques in oncoplastic surgery.a
| Oncoplastic Surgery | |
|---|---|
| Indications | Techniques |
| Type I: the treated breast presents a normal appearance without deformity, but there is asymmetry in the volume or appearance compared to the contralateral breast. | Vertical mammoplasties Inferior rotation mammoplasty Horizontal mammoplasty Lateral mammoplasty Reduction mammoplasty (contralateral breast) |
| Type II: the treated breast presents a deformity that can be corrected with partial breast reconstruction using existing tissue. | |
Access to and achievement of a an official European diploma as Specialist in Breast Surgery (European Board in Breast Surgery), granted and certified by the Division of Breast Surgery of the Section of Surgery of the European Union of Medical Specialists, although with no correlation with an official specialty degree, means that the Specific Training Area Diplomas from our country are not established or officially approved. These documents are prestigious and transcendental for surgeons who are especially involved or dedicated in breast units.13
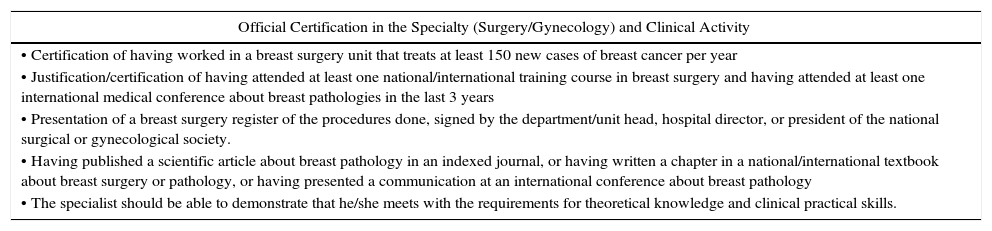
The Division of Breast Surgery advises in matters related with professional practice and training as well as patient care in breast surgery in Europe, working in close collaboration with EUSOMA and the European Society of Surgical Oncology. The main objective of the Division is to promote a high level of care for breast surgery in Europe, including high-quality training and certification. This involves a study plan, evaluation protocol and certification. Access to the training program, training requirements and evaluation testing are specified in Table 5.
Criteria Required in the Process to Obtain European BOARD Certification in Breast Surgery.
| Official Certification in the Specialty (Surgery/Gynecology) and Clinical Activity |
|---|
| • Certification of having worked in a breast surgery unit that treats at least 150 new cases of breast cancer per year |
| • Justification/certification of having attended at least one national/international training course in breast surgery and having attended at least one international medical conference about breast pathologies in the last 3 years |
| • Presentation of a breast surgery register of the procedures done, signed by the department/unit head, hospital director, or president of the national surgical or gynecological society. |
| • Having published a scientific article about breast pathology in an indexed journal, or having written a chapter in a national/international textbook about breast surgery or pathology, or having presented a communication at an international conference about breast pathology |
| • The specialist should be able to demonstrate that he/she meets with the requirements for theoretical knowledge and clinical practical skills. |
Source: BOE no. 280.9
Finally, one point of interest in special cases is the possibility to obtain an Honorary Diploma in Breast Surgery from the European Union of Medical Specialists, which recognizes the experience and prestige of certain breast surgeons who actively contribute and/or have contributed with their activity, contributions and prestige to the development of the field of breast surgery. General requirements for obtaining these diplomas can be found at: http://www.uemssurg.org/divisions/breast-surgery/honorary-diploma.
Core Requirements and Specific Training AreasRoyal Decree 639/20146 defines, among other things, the so-called specific training areas (STA), which “cover a set of knowledge, skills, and approaches added as an extension to those required by the official program of one or several specialties, provided this group of competencies are of relevant scientific, medical, social and organizational interest”. It regulates the procedure for requesting and obtaining an STA specialization diploma.
The request to create an STA should be justified by the following requirements: (1) a significant increase in the professional competencies required by the official programs of the specialties involved; (2) a relevant medical, scientific, social and organizational interest that requires the dedication of a significant number of professionals; and (3) the inability to satisfy these competencies through training in other specialties, other specific qualification diplomas or advanced certification.
Once the STA has been approved, admittance and later certification will be regulated by a specific training program that is monitored and evaluated. Physicians’ positions will be reserved for them, and they will be considered resident specialists in training. Access to the training process for the acquisition of an STA diploma will be done through annual public selection processes, and it will be necessary to be in possession of a corresponding degree as specialist and to certify a minimum of 2 years of effective professional practice in the specialty since the start of the constitution of the STA.7
In this context, it would be coherent for the Spanish Association of Surgeons through the Breast Pathology Section to propose a project that is coherent and appropriate for the current clinical, hospital and legislative situation, which should include a structured training program for residents (in the new core training program) as well as specialists for their different expectations: keeping themselves up-to-date (continuous training and professional development) and access to obtaining a Specific Training Area Diploma in Breast Surgery. The training proposal would precisely define the training program objectives and establish the “roadmap” to optimize the access and preparation of residents and surgeons in this area.
Finally, in accordance with all the previous considerations and premises, aside from any official position and assuming a priori possible criteria discrepancies, a proposed general structured model could be helpful to define the skills to acquire at different levels: cognitive, behavioral and practical during the training period, at each level of training, as well as the method for their evaluation.
Although many of the ideas have been previously discussed, the requirements could be broken down into the following aspects:
- •
Theoretical knowledge, as specified in the current MIR program in the theoretical program of the basic and advanced courses of the Breast Pathology Section of the AEC (Table 2) and in the “Breast Surgery Syllabus” of the Fellow of European Board of Breast Surgery
- •
Management knowledge (based on EUSOMA recommendations)
- •
Training in specific techniques (specified in the MIR program, in the theoretical program of the basic and advanced course of the Breast Pathology Section of the AEC (Tables 2 and 4) and in the “Breast Surgery Syllabus”). Said techniques would include: stereotactic/“harpoon-guided” biopsy; sentinel node biopsy; breast-conserving surgical techniques; mastectomies (total, modified radical, “skin-saving”, radical; implants (prostheses and expanders); oncoplastic techniques; breast reconstruction techniques (latissimus dorsi, TRAM)
- •
Teaching and research
Evaluation would be based on the use of the following methodology:
- •
Written exams–multiple-choice tests and the Script Concordance Test are considered the best instruments, as they can evaluate abstract knowledge, contextualized knowledge, clinical reasoning, decision making.
- •
Structured observation of clinical practice using Mini-CEX (miniature clinical examination) as well as observation in simulated contexts, in order to evaluate the following skills: clinical interview, professional practice, clinical judgment, communication, organization and effectiveness
- •
Medical record audits to analyze the quality of the records generated by the physician evaluated in terms of indictors used and quality standards.
- •
Officially accredited activity records/portfolio
- •
Research and teaching curriculum
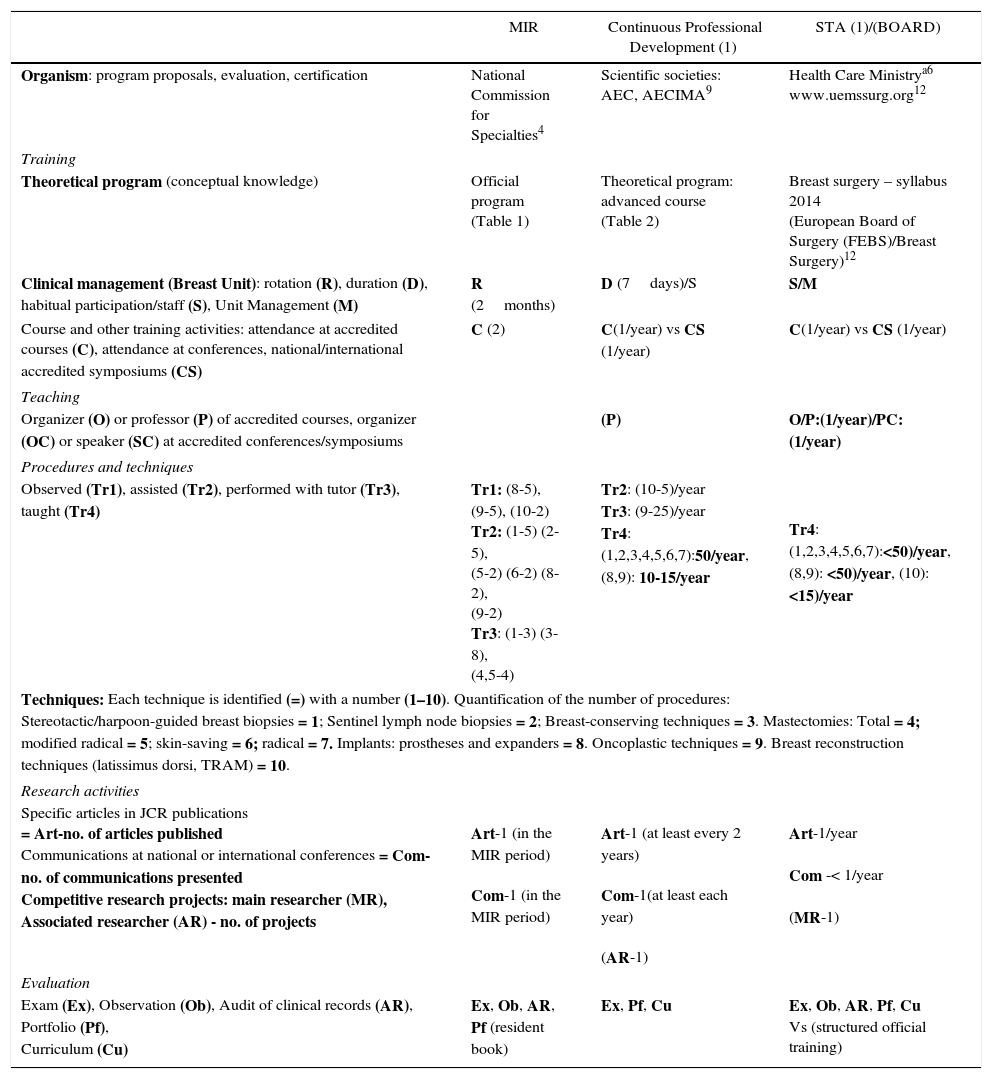
Because explaining the development of all these aspects for the three training levels would be overwhelming, Table 6 systematizes and specifies this proposal in detail by contemplating a general program in extenso and specifies for each the objectives to be reached and the methods to obtain, evaluate and certify them.
Proposal for Training.
| MIR | Continuous Professional Development (1) | STA (1)/(BOARD) | |
|---|---|---|---|
| Organism: program proposals, evaluation, certification | National Commission for Specialties4 | Scientific societies: AEC, AECIMA9 | Health Care Ministrya6 www.uemssurg.org12 |
| Training | |||
| Theoretical program (conceptual knowledge) | Official program (Table 1) | Theoretical program: advanced course (Table 2) | Breast surgery – syllabus 2014 (European Board of Surgery (FEBS)/Breast Surgery)12 |
| Clinical management (Breast Unit): rotation (R), duration (D), habitual participation/staff (S), Unit Management (M) | R (2months) | D (7days)/S | S/M |
| Course and other training activities: attendance at accredited courses (C), attendance at conferences, national/international accredited symposiums (CS) | C (2) | C(1/year) vs CS (1/year) | C(1/year) vs CS (1/year) |
| Teaching | |||
| Organizer (O) or professor (P) of accredited courses, organizer (OC) or speaker (SC) at accredited conferences/symposiums | (P) | O/P:(1/year)/PC:(1/year) | |
| Procedures and techniques | |||
| Observed (Tr1), assisted (Tr2), performed with tutor (Tr3), taught (Tr4) | Tr1: (8-5), (9-5), (10-2) Tr2: (1-5) (2-5), (5-2) (6-2) (8-2), (9-2) Tr3: (1-3) (3-8), (4,5-4) | Tr2: (10-5)/year Tr3: (9-25)/year Tr4: (1,2,3,4,5,6,7):50/year, (8,9): 10-15/year | Tr4: (1,2,3,4,5,6,7):<50)/year, (8,9): <50)/year, (10): <15)/year |
| Techniques: Each technique is identified (=) with a number (1–10). Quantification of the number of procedures: Stereotactic/harpoon-guided breast biopsies = 1; Sentinel lymph node biopsies = 2; Breast-conserving techniques = 3. Mastectomies: Total = 4; modified radical = 5; skin-saving = 6; radical = 7. Implants: prostheses and expanders = 8. Oncoplastic techniques = 9. Breast reconstruction techniques (latissimus dorsi, TRAM) = 10. | |||
| Research activities | |||
| Specific articles in JCR publications = Art-no. of articles published Communications at national or international conferences = Com-no. of communications presented Competitive research projects: main researcher (MR), Associated researcher (AR) - no. of projects | Art-1 (in the MIR period) Com-1 (in the MIR period) | Art-1 (at least every 2 years) Com-1(at least each year) (AR-1) | Art-1/year Com -< 1/year (MR-1) |
| Evaluation | |||
| Exam (Ex), Observation (Ob), Audit of clinical records (AR), Portfolio (Pf), Curriculum (Cu) | Ex, Ob, AR, Pf (resident book) | Ex, Pf, Cu | Ex, Ob, AR, Pf, Cu Vs (structured official training) |
AEC, Association Española de Cirujanos (Spanish Association of Surgeons); AECIMA, Association Española de Cirujanos de la Mama (Spanish Association of Breast Surgeons); FEBS, Fellow of European Board of Surgery; JCR, journal citation reports; TRAM, transverse rectus abdominis myocutaneous flap.
(1): area/(diploma) specific training/European Board.
Both authors have contributed equally to the preparation of this manuscript, from the design and structure to the analysis and interpretation of the data and final composition.
Conflict of InterestsThe authors have no conflict of interests to declare.
Part of the information contained in the manuscript was sent for inclusion in the 2nd Edition of the Breast Pathology Manual of the AEC. The Editor of the Manual, Dr. F. Domínguez Cunchillos, has authorized its presentation in this manuscript. The authors would like to acknowledge this authorization.
Please cite this article as: Miguelena JM, Domínguez Cunchillos F. Formación en cirugía mamaria en España. Cir Esp. 2016;94:323–330.