Perineal injuries are uncommon, but not rare. They may present a wide variety of injury patterns which demand an accurate diagnostic assessment and treatment. Perineal injuries may occur as isolated injuries to the soft tissues or may be associated with pelvic organ, abdominal or even lower extremity injury. Hence the importance to know in depth not only the anatomy of the perineum and its organs, but also the implications of the patient's hemodynamic stability on the decision making process when treating these injuries using established trauma guidelines. The purpose of this review is to describe the current epidemiology and clinical presentation of perineal injuries in order to provide specific guidelines for the diagnosis and treatment of both stable and unstable patients.
El trauma perineal, aunque poco común, no es un evento raro. Puede presentarse con una amplia variedad de patrones de lesión y por esta razón necesita de una precisa evaluación diagnóstica y de tratamientos adecuados. Las lesiones traumáticas del periné pueden presentarse de manera aislada o asociarse a lesiones de otros órganos pélvicos, abdominales o de miembros inferiores. Por esta razón es importante conocer no solo la anatomía del periné y sus órganos sino también la relevancia del estado hemodinámico del paciente en el tratamiento de estas lesiones, de acuerdo con los protocolos de tratamiento del paciente politraumatizado. El propósito de esta revisión es describir las características de las lesiones traumáticas perineales, su presentación clínica y su tratamiento basado en la evidencia más reciente, para intentar definir líneas de diagnóstico y tratamiento específicas tanto en los pacientes en situación de inestabilidad como de estabilidad hemodinámica.
Efficient diagnosis and treatment of perineal trauma injuries require thorough comprehension of the anatomy and functions of the numerous organs present in this complex anatomical region. Perineal trauma, although uncommon, may present with a wide variety of injury patterns, requiring complex diagnostic evaluation and treatment. Nonetheless, very little is known about the epidemiology and results of these injuries. The aim of this review is to describe the characteristics of perineal injuries, their clinical presentation and treatment based on the most recent evidence.
MethodologyWe conducted a search in the PubMed, Embase, and Cochrane online databases. The keyword phrase used was “perineal injuries” and 2704 related articles were found. Included in the study were only those articles published in English and applied to humans, while those articles about cancer, iatrogenic injuries, obstetrics, and pediatrics were excluded; likewise, case reports were also excluded. We also dismissed articles that presented renal involvement or involvement of other organs without a pelvic association. In addition, searches were conducted by affected organ (rectum/anus, genitourinary tract, and pelvis), sex, and injury mechanism (blunt and penetrating). This search turned up a total of 440 articles: 158 were excluded because there was no abstract, 132 did not have the complete text available, and 94 were review articles themselves. This left a final result of 56 relevant publications.
IncidenceThe most extensive retrospective review article in the literature, published by Petrone et al.1 in 2009, covers 13 years (1992–2005) and included 53244 civil trauma victims admitted to a level 1 trauma center in the United States. The incidence of perineal injuries was 0.1% (69/53224), with a male:female ratio of 85:15 and an average age of 30.
Perineal injuries can frequently be associated with open pelvic fractures (1%–4%). The largest military series was written by Mossadegh,2 which included 118 soldiers with perineal lesions (5.4%) secondary to improvised explosive devices.
Mechanisms of InjuryIn the series by Petrone et al.,1 penetrating mechanisms of injury were most frequent at 56%, with a predominance of knife wounds and gunshots. Blunt trauma was observed in 44%, most of which were due to falls, motorcycle accidents, car accidents, car–pedestrian collisions, and foreign bodies.
According to published series1,3–16 about blunt pelvic trauma, automobile-pedestrian collisions are responsible for 41% of perineal injuries, followed by motorcycle accidents (22%), car accidents (20%), falls (16%) and other (1%).
Injuries can range from soft tissue lacerations, low- or high-energy penetrating injuries and impaling, to extensive and devastating injuries associated with complex pelvic fractures due to explosions.
Special mention should be made of animal-related injuries, either in sporting activities in certain countries or related to animal husbandry. Injuries caused by bull goring require particular attention as they not only affect the soft tissue of the perineum but also cause anal, genitourinary and vascular damage.17,18 In severe cases, they can easily cause injury to abdominal organs and even the diaphragm.
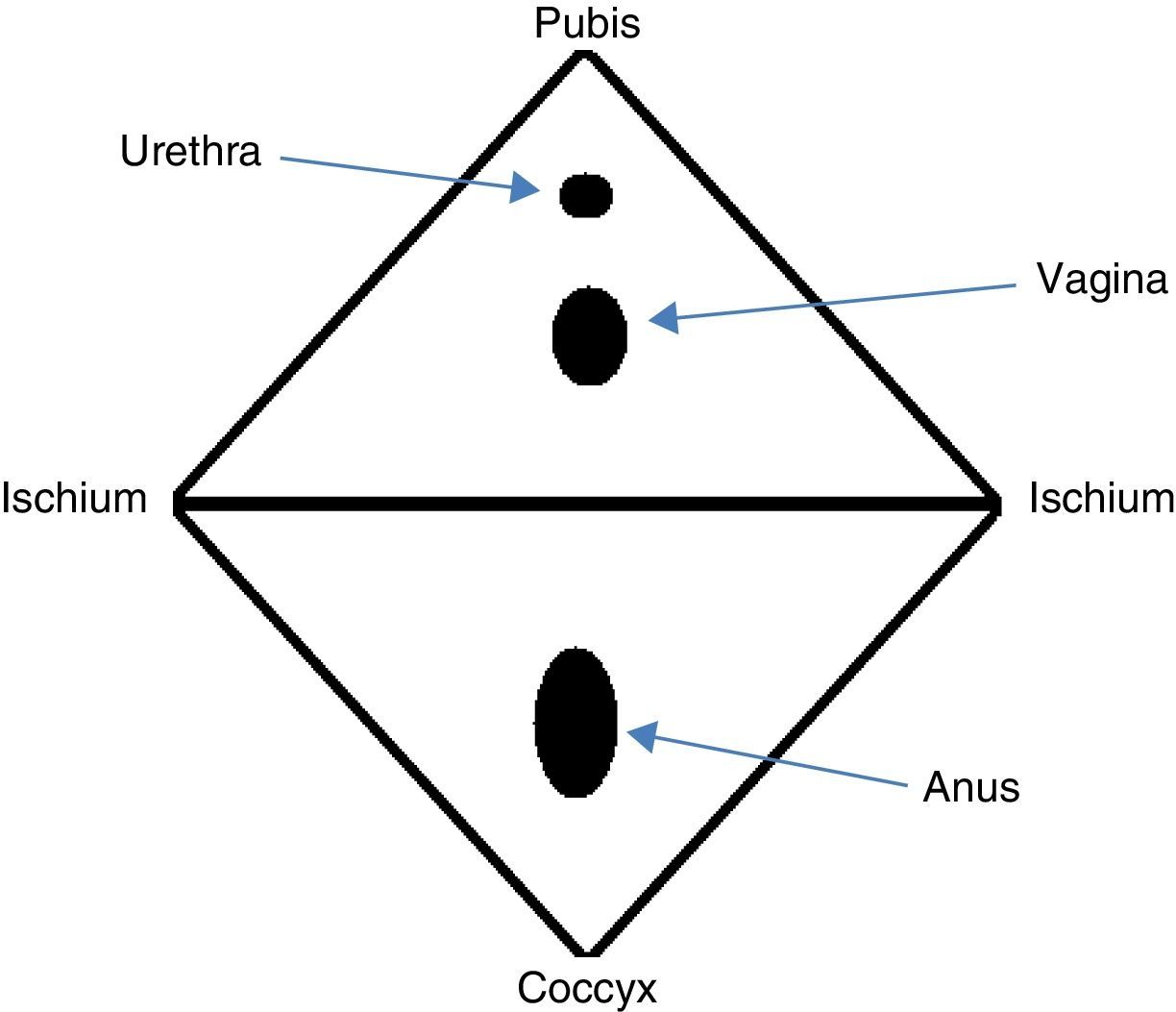
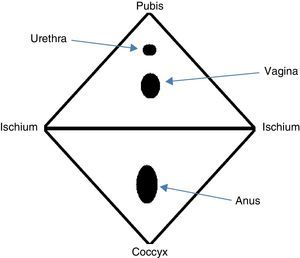
AnatomyThe perineum is a diamond-shaped region comprised of soft tissue that seals the pelvic cavity outlet. The boundaries of this region are the anterior pubic arch, the ischiopubic rami and ischial tuberosities laterally, the posterolateral sacrotuberous ligament and the posterior coccyx (Fig. 1).19,20 In this manner, the perineum is divided into 2 segments: the anterior urogenital triangle and the posterior anal triangle. Both the muscles as well as the fascia of both areas emerge centrally, forming a centrally located fibromuscular mass known as the perineal body.19,20
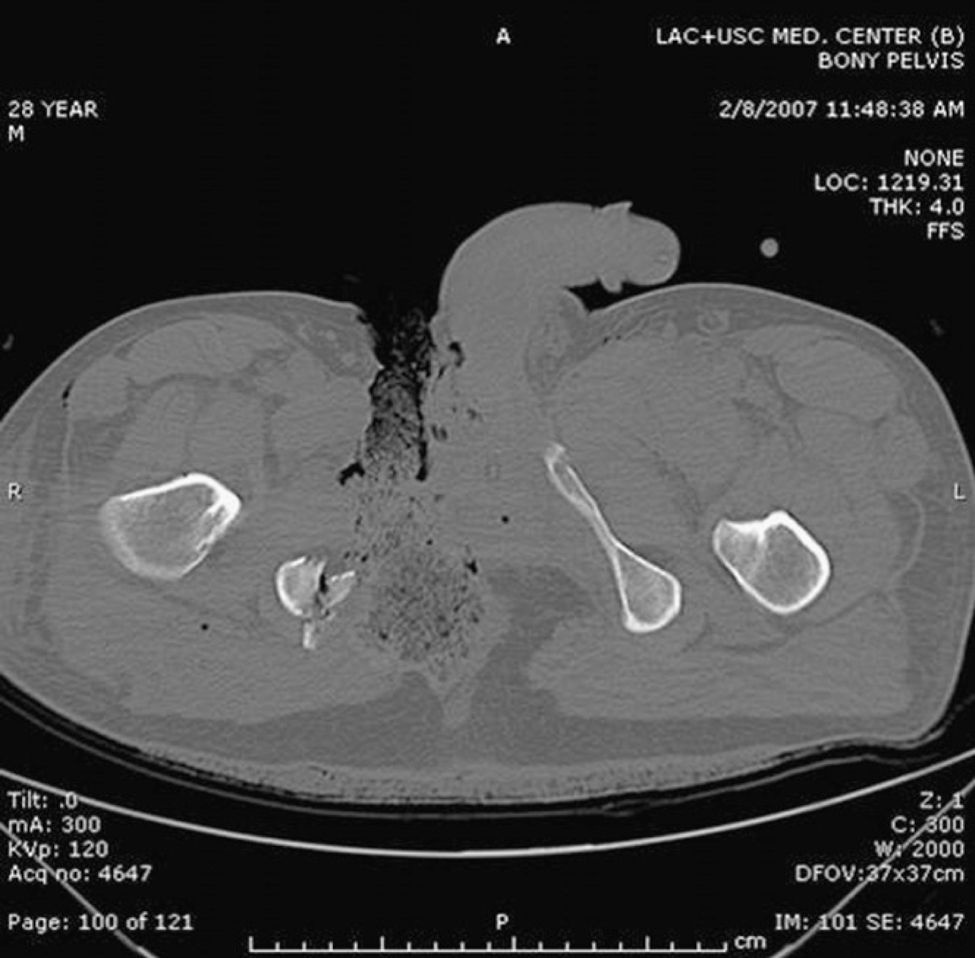
Management PrinciplesPerineal injuries are the result of multiple direct or transmitted forces that act either simultaneously or in sequence. There can be variable effects on the complex interactions of the structures that comprise the perineum, including involvement of the intestines, bladder, and genital organs. Severe perineal injuries (Fig. 2) usually present with a difficult diagnosis and their management is a complex dilemma. The early mortality rate of severe perineal injuries is mainly due to exsanguination as a result of associated lesions, including lacerations of important vascular structures (iliac and femoral vessels), as well as bleeding associated with pelvic and long-bone fractures.12 Some 25% of victims die before reaching the hospital or within a few hours after the incident due to uncontrollable hemorrhage.21 Those who survive massive resuscitation, and even after reaching hemostasis, still face septic complications, which appear in up to 80% of patients with perineal trauma.
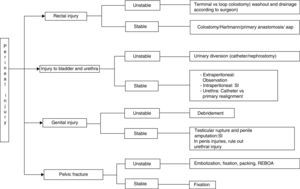
Several authors4,12,21,22 have previously described diagnostic-therapeutic algorithms for proper management of patients with perineal trauma. Trauma patients who are admitted to the Emergency Department should initially be treated in accordance with the Advanced Trauma Life Support23 (ATLS®) protocol of the American College of Surgeons. Life-threatening injuries should be treated before assessing perineal damage which, even if extensive, should not draw our attention away from other possible sources of bleeding.
Associated pelvic injuries should be suspected in patients with scrotal hematomas, perineal hematochezia, hematuria, blood in the urinary meatus, priapism, high prostate or evidence of bleeding during rectal examination.
Management of Unstable PatientsTo interrupt or avoid the patient entering into the vicious circle of the triad of death, which involves the presence of acidosis, hypothermia and coagulopathy, damage control will involve controlling bleeding and contamination, while postponing definitive repairs for a second intervention.
Bleeding control is a priority in the management of these patients. The estimated capacity of the pelvis is 4L, and when this space is opened during surgery its volume can increase by 15%, with a loss of the seal effect of the peritoneum and the abdominal wall. Open wounds of the perineum are the decompression pathway of retroperitoneal hematomas, so bleeding associated with these wounds will be more difficult to control and will more frequently require embolization.
In perineal injuries with compromised hemodynamics, stabilization of the pelvis reduces bleeding, partially due to the approximation of the edges of the fractured bone, diminishing the mobility of the pelvis and allowing for the formation of stable coagulation. Due to the trauma mechanism and the anatomy of the pelvic fracture, Tile types B and C have the greatest risk for patient instability since type B are rotationally unstable while type C are rotationally and vertically unstable. Given the diagnosis of these fractures during the primary assessment, patients benefit from immobilization by the placement of a pelvic binder or sheet at the height of the femoral trochanters until definitive fixation, angioembolization or surgical intervention to stop the bleeding can be done.
85% of pelvic bleeding is usually venous, and preperitoneal packing is effective in this type of hemorrhage. The remaining 15% presents as arterial bleeding, which will require embolization. This can be done as an initial therapeutic option in unstable patients with isolated pelvic–perineal injuries or after ineffective packing.
In extremely unstable patients, Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) can be used in zone III, an area that is outlined by the anterior apex of the bladder, the posterior promontory and the lateral iliac crests. It has recently been described how this device can be inserted with a 6 French sheath into one of the femoral arteries without the need for a guide wire. As it stays under the renal arteries, the REBOA balloon isolates the pelvis and provides temporary patient stabilization.24 When the hemorrhage is under control, the extension of the injuries is determined, as well as the degree of contamination and involvement of the adjacent structures.
Terminal colostomy is effective for adequate fecal diversion. Alternatively, loop colostomy, with closure of the distal lumen by manual as well as mechanical sutures, provides similar results and is less time-consuming for creation as well as reconstruction.25–29
In hemodynamically unstable patients with bladder and urethra injuries, adequate urine drainage is considered a priority. This can be done with a conventional bladder catheter, suprapubic drainage or, in cases of more severe injuries, by means of bilateral nephrostomy.30,31 Genital injuries are usually not life-threatening; therefore, in hemodynamically unstable patients, measures include control of arterial bleeding, profuse irrigation and debridement of the lesions while trying to leave the largest possible surface of viable tissue. Very extensive injuries may benefit from VAC placement, which involves the application of negative pressure on the wound to stimulate healing.
Management of Stable PatientsRectal InjuriesAlthough the use of rectal examination is contemplated to determine possible associated injuries during the primary and secondary reviews of polytrauma patients, some 77% of these injuries go unnoticed. Rectal exams present a specificity of 95% and a sensitivity of 24%, for the case of specific injuries such as medullary (37%), rectal (33%), urological (20%), intestinal (6%), and its utility for the diagnosis of pelvic fractures is minimal.32–34
Rectal integrity can be evaluated by proctosigmoidoscopy and with radiopaque contrast studies (gastrografin), later completing the study under anesthesia. Axial computed tomography can also be of use (Fig. 3), with a sensitivity of 100% and a specificity of 96% when done with triple contrast.29,35
Computed axial tomography of the patient from Fig. 2, which shows fracture of the right pelvic ramus associated with the perineal injury.
For many years, it has been considered that colostomy, presacral drainage, and rectal stump washout were the pillars for treatment of rectal injuries. Current evidence indicates colostomy as the cornerstone of rectal trauma treatment. The study by Berne et al.36 found that colostomies created due to rectal damage have a better prognosis than those that were done due to injury of the colon (12.5% vs 55%), a higher rate of morbidity in terminal colostomies than in the loop-type, and an increase in complications when the closure time exceeds 3 months (44%) and 6 months (53%).
As for presacral drainage and washout, although the studies by Gonzalez et al.37 and Steele et al.29 considered that the evidence of its efficacy is too weak, its use is still indicated in this type of lesions.
Sphincter ComplexThere is a lack of current information about trauma damage to the anal sphincter and its reconstruction; therefore, the possibility to establish clear recommendations is complex. Anal sphincter injuries should be evaluated in the clinical and hemodynamic context of the patient. In those who present hemodynamic instability and who require the evaluation and management of vital organ damage, the indemnity of the sphincter apparatus should be later evaluated.
In hemodynamically stable patients and in patients with limited damage, primary repair can be done with suture of the muscle fibers and skin coverage which, in most cases, is able to fulfill the functional state even if it is not able to maintain the primary esthetic condition. Even though sphincteroplasty may not have been done initially, it can be completed in the following 6 months.
Last of all, in extensive injuries and those with a large loss of tissues, it is recommended to defer reconstruction of the sphincter apparatus by means of an artificial sphincter or graciloplasty.38,39
Indication for ColostomyIn abdominal trauma and since the implementation of damage control surgical techniques in patients in critical condition secondary to trauma, it is considered that in patients with hemodynamic instability, profuse bleeding, damage to different abdominal organs and trauma with colon injury, the first step should be transit diversion, followed by later reconstruction. Primary reconstruction should be considered in patients with non-severe injury and hemodynamic stability, since there has been no evidence that these patients have a greater risk for complications than those with colostomy.40 This point is relevant in injuries of the intraperitoneal rectum, in which primary reconstruction in hemodynamically stable patients is determined by the magnitude of damage and the association of lesions in neighboring organs.
Large perineal injuries with extensive loss of tissue, or associated with sphincter lesions, are considered complex lesions that require initial fecal diversion and, subsequently, complementary studies for probable reconstruction of the affected parts.27,32
With current evidence, there is more controversy about primary repair than colostomy as an initial technique and, although no significant differences have been demonstrated regarding complications between primary repair and colostomy, there still have been no reports of statistical importance to indicate which is the best initial technique in patients with anorectal trauma injuries.
Genitourinary InjuriesIn patients with relevant findings, such as pelvic fractures associated with hematuria, cystography or computed tomography cystography should be done.28,41–43 Today, microhematuria alone is not considered an indication for complementary studies.41,43–45
As for bladder damage, all situations with an intraabdominal component require surgical treatment.28,41–43,45,46 It is currently considered that extraperitoneal bladder damage should be managed conservatively by means of urinary diversion, preferably with a Foley catheter for 10–14 days, and cystography should be done at the end of this period.28,45 There are some complications derived from this conservative management, including delayed healing, the formation of vesicocutaneous fistulas, abscesses, hematomas, and pelvic sepsis. It has been observed that these lesions are associated with more severe injuries, those who required more than 5 units of blood during reanimation, and those who had poor functioning of the bladder catheter. It is for this reason that the Kotkin study45 prioritizes the use of large-caliber catheters and wide-spectrum antibiotics due to possible complications.
Surgical management of extraperitoneal bladder lesions should be contemplated when associated with penetrating trauma to the rectum or genital organs and in situations with pelvic fracture stabilization.43
Urethral canalization should not be attempted if there is evidence of signs of possible injury; it is first recommended to explore the magnitude of the damage using retrograde urethrography (Fig. 4).28,41 The initial management of urethral trauma depends on the type of injury, and its objectives are not only to reestablish the function but to also avoid sequelae, such as stenosis, impotence, retention, and incontinence. Partial injuries can be managed with a catheter for 2–6 weeks, while total disruptions require surgical intervention.43 Thus, posterior urethral lesions can be managed with suprapubic cystostomy and definitive repair can be done up to 12 weeks later, while total anterior urethral damage should be explored and repaired over the catheter using resorbable sutures.
As for genital injuries, such as testicular rupture (evidence of which is observed by the disruption of the tunica albuginea and extrusion of seminiferous tubules), surgical repair should be done as soon as possible as the probability to save the testicle increases to almost 90% if done in the first 72h, while also reducing the risk for infertility and chronic pain.43,47
80% of penis trauma present with associated injuries to other organs and areas like the scrotum, perineum, abdomen, and lower extremities. Both in penile amputations as well as other types of trauma (for example, bites, avulsions) the main objective should be to determine the patient's status and provide appropriate resuscitation. Once stabilized, the penis should be re-implanted as soon as possible to increase the chances for success43,47; meanwhile, the bladder catheter should be maintained until closure of the defect has been confirmed. With regards to avulsion, the main treatment is primary suture by an urologist.48
As for injuries to female genital organs, although it is very rare for vulvar bleeding to be life-threatening, it can be the manifestation of a larger vaginal, uterine or intraabdominal lesion.43
Soft TissueThe most frequent findings are hematomas due to the important vascularization of the perineum itself. When these hematomas expand, there is an indication for incision and subsequent drainage, depending on their size.49 Conservative management of large hematomas has been associated with a high frequency of complications, requiring antibiotics and transfusions, and consequently prolonged hospitalizations.50
Therefore, several steps are required in the effective treatment of perineal injuries. Wound irrigation is extremely important, followed by repeated aggressive surgical debridement and removal of devitalized tissue, and close vigilance of the lesions with evaluations over the first 4 days. Approximation of the wounds is not recommended until the appearance of granulation tissue. Both periodic debridement as well as fecal diversion are crucial to prevent continuous contamination of the perineal wound.6,19 Sepsis is a common late complication that is a cause for concern in perineal injuries. In a study of 25 patients with severe injury to the perineal soft tissue,6 it was found that intermittent irrigation and aggressive daily debridement of all the non-viable soft tissue reduced pelvic septic complications, even if they required the creation of extensive perineal or perianal cavities. Once the patient is stable, with the wound clean and granulating, the resulting soft tissue defects are covered with either grafts, free flaps or pedunculated flaps.6
A possible alternative to irrigation could be the use of VAC, which offers a moist atmosphere with reduced bacterial colonization, increases local vascularization, and achieves good control of extensive perineal wounds.7–9
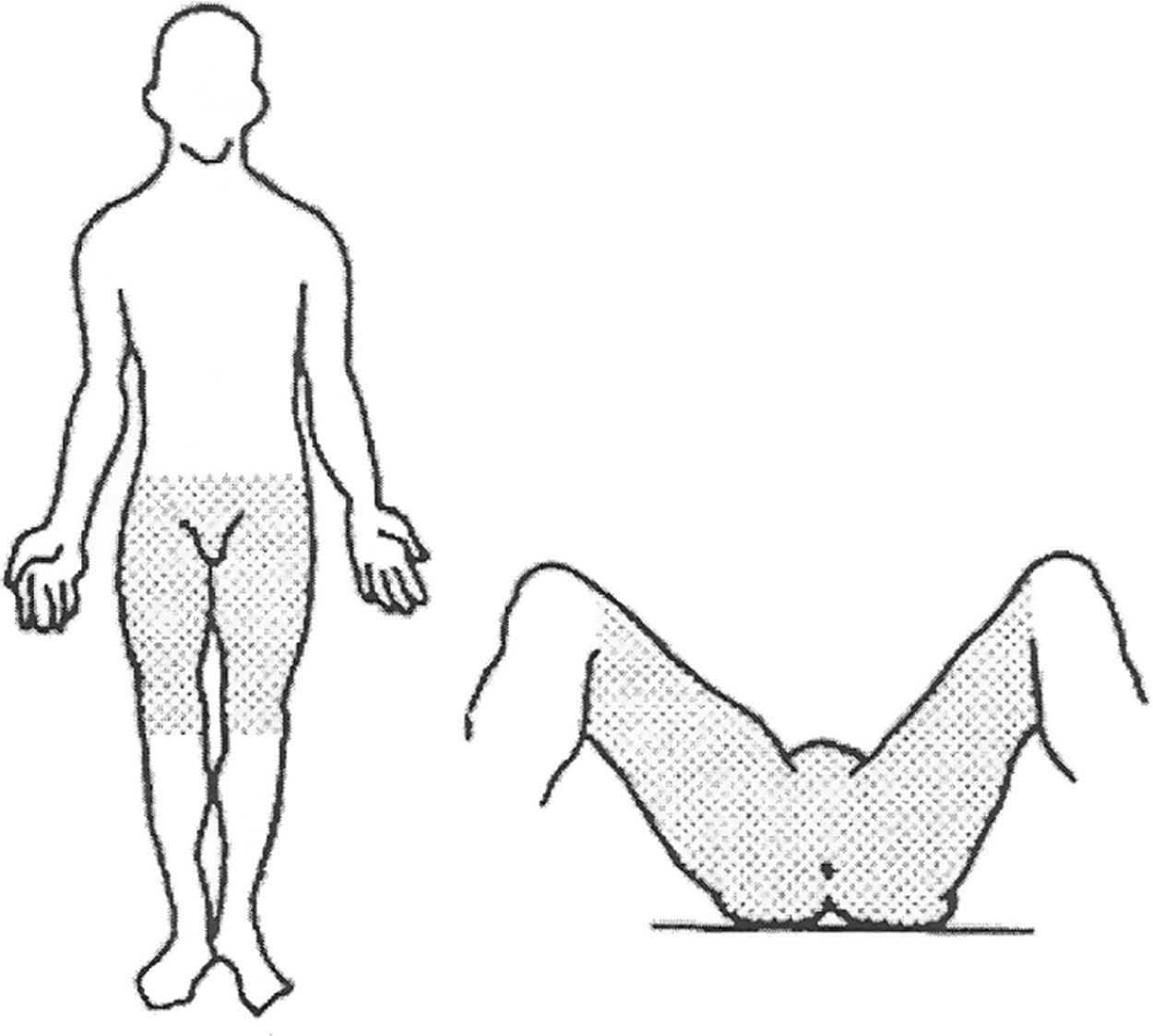
There is usually an important association between fractures and the amount of avulsion tissue that extends distally toward the thighs (Morel-Lavalle injury). The skin flaps and pockets formed in this region should be treated with the same aggressive approach and early debridement in accordance with the concept of the “expanded perineum” by Kusminsky (Fig. 5).12 This concept gives a more precise idea of the extension of the lesion and, in cases in which the actual extension of the damage is not completely defined, simplifies the indications for colostomy and for urinary diversion. This notion of expanded perineum foresees the involvement of the soft tissue in patients with pelvic–perineal injuries, so it can be inferred that it compromises not only the superficial area but also extends beyond the deep fascia.
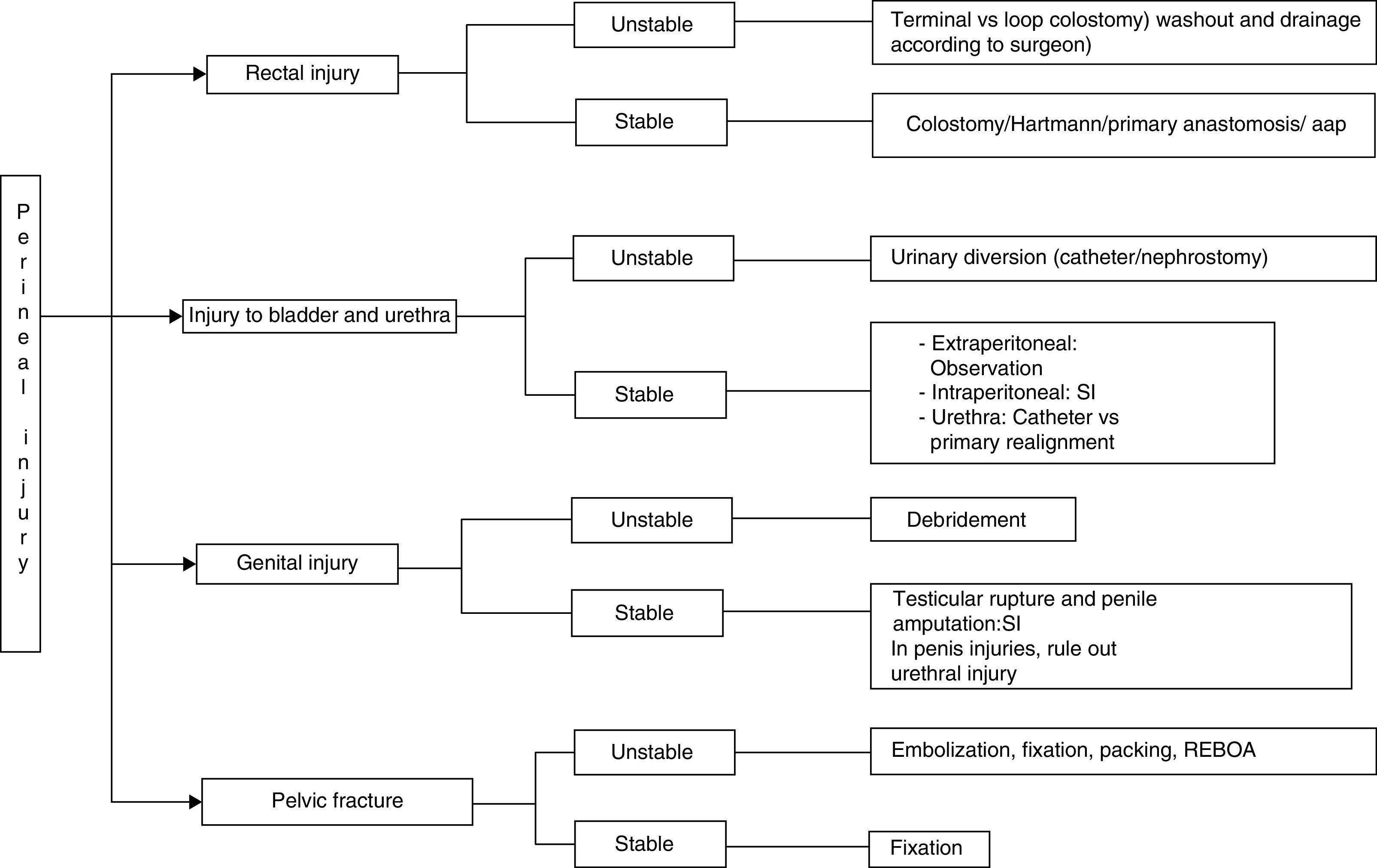
The subsequent use of bowel diversion, bladder catheter or nephrostomy, antibiotic therapy, enteral or parenteral nutrition and the appropriate management of fractures4,20,51–53 is dictated by the extension of the trauma, associated lesions, and patient status (Fig. 6). In cases of extensive injury of the anus and its sphincter, abdominoperineal resection may become necessary. If the general patient condition makes this impossible during the initial intervention, it may be done in a second surgery.6 Genitourinary injury repair and closure of perineal wounds are recommended only after pelvic sepsis has been controlled.19
Antibiotic TreatmentPatients with perineal trauma injuries have a high probability to present infections and secondary sepsis due to the trauma mechanism, introduction of foreign bodies within the organism, and damage inflicted on the organs of this location, mainly the rectum. Thus, the management of perianal injuries contemplates the administration of empirical antibiotic treatment, which should be initiated within the first hour after the trauma and once the hemodynamic status of the patient and nature of the injuries have been determined (recommendation 1B).
The choice of the most appropriate antibiotic treatment and its duration will be determined by the magnitude of the trauma and the possible contamination involved (recommendation 1B). In patients with severe lesions, it is recommended to use one or more antibiotics with appropriate spectrums and penetration in the damaged tissue in order to ensure correct coverage.54 Management guidelines should be established at each reference hospital and should contemplate the different protocols based on microbial resistances and access to different antibiotics.
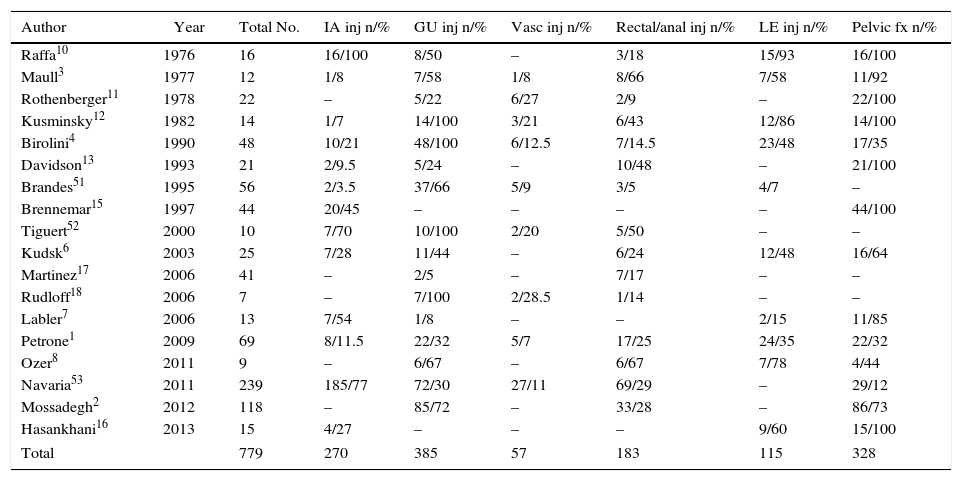
Morbidity and MortalityComplex pelvic trauma usually has an insidious evolution, principally due to the contamination originating from the structures that comprise the perineum and the presence of associated injuries (Table 1). The most frequent complications are wound infections, abdominal abscesses and late hemorrhages, while causes of death include exsanguination, sepsis, and multiple organ failure (Tables 2 and 3).
Perineal Trauma and Frequency of Associated Lesions.
| Author | Year | Total No. | IA inj n/% | GU inj n/% | Vasc inj n/% | Rectal/anal inj n/% | LE inj n/% | Pelvic fx n/% |
|---|---|---|---|---|---|---|---|---|
| Raffa10 | 1976 | 16 | 16/100 | 8/50 | – | 3/18 | 15/93 | 16/100 |
| Maull3 | 1977 | 12 | 1/8 | 7/58 | 1/8 | 8/66 | 7/58 | 11/92 |
| Rothenberger11 | 1978 | 22 | – | 5/22 | 6/27 | 2/9 | – | 22/100 |
| Kusminsky12 | 1982 | 14 | 1/7 | 14/100 | 3/21 | 6/43 | 12/86 | 14/100 |
| Birolini4 | 1990 | 48 | 10/21 | 48/100 | 6/12.5 | 7/14.5 | 23/48 | 17/35 |
| Davidson13 | 1993 | 21 | 2/9.5 | 5/24 | – | 10/48 | – | 21/100 |
| Brandes51 | 1995 | 56 | 2/3.5 | 37/66 | 5/9 | 3/5 | 4/7 | – |
| Brennemar15 | 1997 | 44 | 20/45 | – | – | – | – | 44/100 |
| Tiguert52 | 2000 | 10 | 7/70 | 10/100 | 2/20 | 5/50 | – | – |
| Kudsk6 | 2003 | 25 | 7/28 | 11/44 | – | 6/24 | 12/48 | 16/64 |
| Martinez17 | 2006 | 41 | – | 2/5 | – | 7/17 | – | – |
| Rudloff18 | 2006 | 7 | – | 7/100 | 2/28.5 | 1/14 | – | – |
| Labler7 | 2006 | 13 | 7/54 | 1/8 | – | – | 2/15 | 11/85 |
| Petrone1 | 2009 | 69 | 8/11.5 | 22/32 | 5/7 | 17/25 | 24/35 | 22/32 |
| Ozer8 | 2011 | 9 | – | 6/67 | – | 6/67 | 7/78 | 4/44 |
| Navaria53 | 2011 | 239 | 185/77 | 72/30 | 27/11 | 69/29 | – | 29/12 |
| Mossadegh2 | 2012 | 118 | – | 85/72 | – | 33/28 | – | 86/73 |
| Hasankhani16 | 2013 | 15 | 4/27 | – | – | – | 9/60 | 15/100 |
| Total | 779 | 270 | 385 | 57 | 183 | 115 | 328 | |
Fx, fracture; GU, genitourinary; IA inj, intraabdominal injuries; LE, lower extremities; Vasc, vascular.
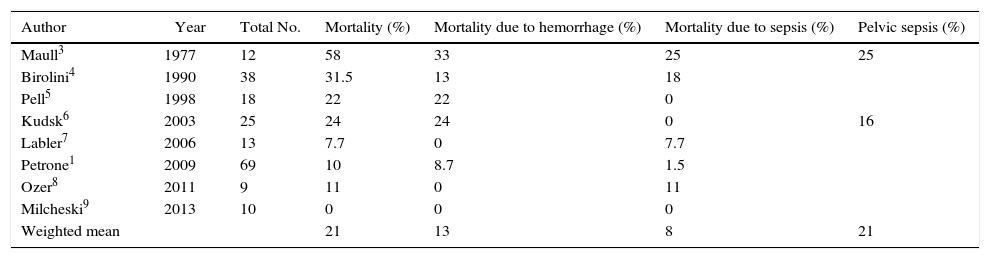
Mortality Associated With Blunt Pelvic Trauma.
| Author | Year | Total No. | Mortality (%) | Mortality due to hemorrhage (%) | Mortality due to sepsis (%) | Pelvic sepsis (%) |
|---|---|---|---|---|---|---|
| Maull3 | 1977 | 12 | 58 | 33 | 25 | 25 |
| Birolini4 | 1990 | 38 | 31.5 | 13 | 18 | |
| Pell5 | 1998 | 18 | 22 | 22 | 0 | |
| Kudsk6 | 2003 | 25 | 24 | 24 | 0 | 16 |
| Labler7 | 2006 | 13 | 7.7 | 0 | 7.7 | |
| Petrone1 | 2009 | 69 | 10 | 8.7 | 1.5 | |
| Ozer8 | 2011 | 9 | 11 | 0 | 11 | |
| Milcheski9 | 2013 | 10 | 0 | 0 | 0 | |
| Weighted mean | 21 | 13 | 8 | 21 |
Mortality Associated With Open Pelvic Fracture.
| Author | Year | Total No. | Mortality (%) | Mortality due to hemorrhage (%) | Mortality due to sepsis (%) | Pelvic sepsis (%) |
|---|---|---|---|---|---|---|
| Raffa10 | 1976 | 16 | 50 | 7 | 43 | 50 |
| Rothenberger11 | 1978 | 22 | 50 | 13.6 | 13.6 | |
| Kusminsky12 | 1982 | 14 | 42 | 21 | 21 | |
| Davidson13 | 1993 | 21 | 5 | 5 | 0 | 14 |
| Faringer14 | 1994 | 33 | 18 | 3 | 0 | 50 |
| Brenneman15 | 1997 | 44 | 25 | 6.8 | ||
| Hasankhani16 | 2013 | 15 | 13.3 | 6.7 | 6.7 | 20 |
| Weighted mean | 29 | 9 | 14 | 32 |
Petrone et al.1 reported a low rate of mortality due to perineal injuries, which occur in most cases as a result of exsanguination due to associated injuries, especially pelvic fractures. Although the required treatments vary considerably, the frequency of colostomy procedures was low. The mortality rate of perineal injuries was primarily associated with low rates of trauma, the Glasgow coma scale and a high rate of damage severity.
Cases of early mortality are mainly due to the difficulty to control bleeding. Abdominal and lower extremity compression systems have not been shown to be effective. Selective angioembolization, however, has been seen to be effective, except in cases in which biosafety levels are surpassed, such as in the case of pregnant women.55–57 These techniques are useful in cases of pelvic or lower limb fractures as an additional method to external fixation systems.
Perineal trauma with massive soft tissue and musculoskeletal injuries contribute to the development of sepsis and kidney failure. The treatment of rhabdomyolysis includes providing adequate intravenous fluids in order to ensure a diuresis of 2mL/h and the administration of osmotic diuretics, if necessary.12
The risk for pelvic sepsis increases with anorectal involvement and, especially, with the delay of colostomy. The combination of pelvic sepsis associated with pelvic fractures is a potentially lethal combination.
From a urological standpoint, the bladder and membranous urethra are the most frequently injured elements: the latter carries a high risk for stenosis (4%–12%) and erectile dysfunction (12%).12,58 Some authors evaluate the possibility of initial endoscopic urethral realignment in cases of injuries that do not affect more than 50% of the circumference of the urethra, but with absence of transection, avoiding suprapubic drainage, and, although this is not contemplated in the initial principles of management of unstable patients, a reduction has been seen in the later rate of stenosis.47,59,60
Along with the increased survival of these patients, there are also increased long-term morbidity rates. These patients usually have altered stability, chronic pain, urinary and sexual dysfunctions, anal incontinence and psychological sequelae that require rehabilitation, and multiple interventions. Although most patients achieve a good level of self-care, they are usually affected by physical limitations, poor social integration, and unemployment.15
ConclusionsThe presence or absence of hemodynamic instability in patients with complex perineal injuries is of utmost importance as this will determine the approach used in their management. In more severe cases and following the protocols for damage-control surgery, the procedures should be defined as quickly as possible, and patients should be transferred rapidly from the operating room in order to continue with the process of reanimation. Therefore, and based on the algorithm of Fig. 6, treatment should be based on the following pillars:
- -
Loop colostomy (over rod), with closure of the terminal loop using mechanical or manual suture; the Hartmann procedure is not recommended since it requires an unnecessarily long time, in addition to the complications of delayed closures.
- -
Urinary diversion with bladder catheter or suprapubic cystostomy; nephrostomy is reserved for when the patient has been stabilized.
- -
Pelvic fixation and angioembolization in cases of pelvic fractures; when this is not possible, fixation, and packing are used. REBOA is limited to hospitals where it is available.
- -
Soft tissue: daily debridement and washout, with drain placement
- -
Genital injury repair should be postponed until the condition of the patient allows for it, although within 72h of the trauma.
Along the same lines of damage control, extraperitoneal packing is gaining popularity. The procedure entails a low median incision or a Pfannenstiel; the muscles are separated and the pelvic hematoma is suctioned. Afterwards, the pelvic packing is inserted and applied against the peritoneum, and the retroperitoneal fascia is closed, exerting a plugging effect. Two premises should be followed when performing this technique: (1) always remain within the extraperitoneal space; and (2) if laparotomy is necessary, the two incisions should not coincide, or the tamponade effect will be lost.
Injuries of the perineum are a considerable challenge for diagnosis and management. Several systems are frequently affected by this type of injury due to the close relationship between the genitourinary and intestinal tracts, the pelvis and the soft tissue of this area. For this particular type of lesions, a multidisciplinary approach is required involving different surgical specialties, including trauma surgeons, coloproctologists, plastic surgeons, orthopedists and traumatologists, urologists, gynecologists, pediatric surgeons, and interventional radiologists.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Petrone P, Rodríguez Velandia W, Dziaková J, Marini CP. Tratamiento del trauma perineal complejo. Revisión de la literatura. Cir Esp. 2016;94:313–322.