Milligan–Morgan and Ferguson haemorrhoidectomy has been the gold standard treatment for symptomatic haemorrhoids for many years. However, escisional techniques are associated with a significant morbidity rate. In recent years, diverse techniques have been described in an attempt to decrease these complications. The guided transanal haemorrhoidal dearterialization THD) doppler is one of these techniques. We report our experience with this new technique.
MethodsWe performed a prospective study of 475 patients from 5 hospitals from the National Health System, in Spain. The majority of these patients suffered from third grade haemorrhoids (256 [56%]) and underwent THD. We analyse and compare preoperative and postoperative results as well as the homogeneity of the technique between hospitals.
ResultsSpinal anaesthesia was the most elected procedure by the anaesthetist (81.0%). Statistically significant differences were found between pre and postoperative symptoms (P=.03), with an overall improvement after surgery. The average hospitalisation was 0.4±0.3 days. The mean number of days of oral analgesics was 8.8±2.7 days. The cumulative complication rate is 16%.
ConclusionTHD is a safe and easily reproducible procedure. Postoperative outcomes demonstrated a low rate of morbidity and recurrence together with early discharge; therefore, a rapid incorporation to daily activities was noted.
Durante varias décadas, las hemorroidectomías de Milligan-Morgan y Ferguson han sido la referencia en el tratamiento de la enfermedad hemorroidal sintomática. Sin embargo las técnicas escisionales llevan asociadas una morbilidad no despreciable. En los últimos años han surgido una serie de técnicas dedicadas a disminuir estos problemas. La desarterialización hemorroidal transanal (THD) guiada por doppler es una de estas técnicas. El objetivo de este estudio es analizar sus resultados según la experiencia de varias unidades especializadas.
MétodosEl estudio se realizó en 5 hospitales de la red pública de España. Se analizan y comparan los resultados pre- y posquirúrgicos, así como la homogeneidad interhospitalaria de dicha técnica.
Se recogieron de forma prospectiva consecutiva datos de un total de 475 pacientes intervenidos mediante THD, la mayoría con hemorroides grado III (267 casos [56%]).
ResultadosLa técnica anestésica preferida fue la anestesia raquídea, en un total de 398 casos (81%). Encontramos mejoría global tras la intervención ya que existen diferencias estadísticamente significativas entre síntomas pre- y postoperatorios (p=0,03). La estancia media fue de 0,4±0,3 días. Los días de analgesia media fueron 8,8±2,7 días (paracetamol y AINE). La tasa acumulada de complicaciones fue del 16%.
ConclusionesLa THD es una técnica segura y fácilmente reproducible. Los resultados posquirúrgicos generan una escasa morbilidad, con una estancia hospitalaria muy reducida que permite una rápida reincorporación a la vida laboral, y una tasa de recurrencia baja.
Milligan–Morgan1 or Ferguson2 haemorrhoidectomies have been considered the gold standard for the surgical treatment of symptomatic haemorrhoidal disease assuming the complications and morbidities inherent to this kind of interventions: prolonged postoperative pain, delayed healing, persistent bleeding, urinary retention, infection, and even various degrees of incontinence. In an attempt to improve these problems, other nonexcisional methods intended to provide the same favourable outcomes while minimising the unfavourable consequences have been developed. Examples of this approach are sclerotherapy, photocoagulation, cryotherapy,3 or Barron's rubber band ligation.4 However, these interventions are indicated in selected patients and often require several sessions of treatment, but they are known to cause less postoperative pain and may be performed as an outpatient procedure. Since 1995 there have been further options available, such as stapled anopexy5,6 and another procedures based on the ligation of the terminal branches of the superior rectal artery (haemorrhoid artery ligation, HAL) with a proctoscope equipped with a Doppler probe, as described by Morinaga et al.7 Another technique, called transanal haemorrhoid dearterialisation (THD) by Shon,8 consists of the application of several continuous longitudinal sutures from a point of maximum flow, located with the Doppler probe up to several millimetres above the dentate line, with the purpose of occluding circulation in the terminal branches of the superior rectal artery. The sensitive anoderm distal to the dentate line is avoided, minimising postoperative pain and providing a shortened recovery time.9–11
The purpose of this paper is to evaluate the efficacy of dearterialisation and haemorrhoidopexy in terms of improvement in postoperative symptoms such as pain, bleeding, recurrence and hospital stay.
Materials and MethodsPatientsA multicentre, observational study with prospective data collection was conducted including a total of 475 patients enrolled consecutively from January 2011 to January 2013, corresponding to five surgical teams from five Spanish public hospitals where the THD technique is performed. The inclusion criteria were: age over 18 years and a previous diagnosis of surgical treatment-naive symptomatic haemorrhoidal disease, as well as refused medical treatment or when medical treatment (diosmin, fluocinolone acetonide, analgesics/anti-inflammatory drugs by systemic or local route) turned out to be ineffective. The predominant symptoms were persistent rectal bleeding or proctalgia with the marked cyclic nature of haemorrhoidal disease. Other causes of rectal bleeding were ruled out by physical examination and rectosigmoidoscopy. Data on additional concurrent symptoms or conditions were also collected: pruritus, mucosal prolapse and fissure. The following variables were collected for data analysis: age, sex and grade of haemorrhoids based on the typical classification: grade I haemorrhoids that bleed but do not prolapse through the anus; grade II haemorrhoids that prolapse through the anus during defecation but reduce spontaneously; grade III prolapsed haemorrhoids that require manual reduction; grade IV haemorrhoids that cannot be reduced manually.
With respect to surgery, patients were anaesthetised by spinal anaesthesia or laryngeal mask. Additional parameters were taken into account, such as surgery time in minutes, whether dearterialisation was performed alone or in association with mucopexy or any other kind of intervention for an added condition (sphincterotomy, skin tag excision), and whether the so-called “marked point” was used to end the mucopexy suture.
After surgery, days of hospitalisation, postoperative pain assessed by visual analogue scale (VAS), symptoms subsequent to the first examination (usually within the first week), days of oral analgesics (pain duration), days off from work, recurrence as from the first month (recurrence should be understood as the reappearance of the condition at an equal or lower grade than before) were collected after the surgery. Other symptoms such as presence and duration of postoperative bleeding, rectal tenesmus and any further complication were equally assessed, as well as the occurrence of repeated surgeries and months of follow-up.
All the patients were duly informed about the procedure and signed the respective informed consent.
TechniqueIn all cases patients were operated on with the same THD technique in an outpatient major surgery programme. Despite the fact that surgeries were performed at different hospitals, the technique is standardised and the teams of specialists are specifically trained. Antibiotics were not administered before, during or after the surgery. A THD device (modified and distributed by THD S.p.A., Correggio®, Italy) was used. It consists of an anoscope with an elliptical cross section specially designed to mount a Doppler probe oriented to the rectal mucosa, which allows identification of the point of maximum flow of the superior rectal artery in its submucosal course immediately above the sphincter. The device also has a source of light and a window through which sutures can be placed. The six spots of maximum acoustic signal corresponding to the six main trunks of the haemorrhoidal arteries, located constantly at 1, 3, 5, 7, 9 and 11 o’clock positions, are identified. A transfixion stitch is applied in the mucosa and submucosa at each location (2/0 polyglycolic acid suture with 5/8inch needle) for artery ligation. The anoscope is equipped with a pivot hole to support the needle holder; thus, both depth and thickness of the wall are secured and homogenised for the entire transfixion suture. A mucopexy is required for haemorrhoids with mucosal prolapse; for such purpose, we continue with four or five stitches of continuous suture distally, never surpassing the dentate line. The sliding part of the anoscope is useful for this procedure. In some cases of prolapse (grade IV), it may be necessary to repeat this continuous suture under the first stitch of the dearterialisation.
Statistical AnalysisThe IBM SPSS Statistics programme was used for data analysis. The results from the five hospitals were analysed in an overall manner homogenising the sample and analysing standard deviations and intra-hospital differences with respect to epidemiological data, technical aspects and results.
The statistics and analyses of preoperative and postoperative symptoms were performed by Student's t-distribution for paired data.
ResultsA total of 475 patients were included in the study. They had a mean age of 50 years and inter-hospital deviation of ±1.9 years. Out of them, 52.5% were males versus 47.5% females. A total of 267 cases corresponded to grade III haemorrhoids (56.2%), 134 cases were grade IV (28.2%), 72 were grade II (15.2%) and only 2 of them were grade I (0.4%). The primary symptom was bleeding in 351 patients (73.9%), proctalgia in 174 (36.6%) and haemorrhoidal prolapse in 106 (22.3%) patients.
The most commonly used anaesthetic technique was regional or spinal anaesthesia in 398 (83.7%) cases. The mean intervention time was 47±13.3min. Sixty-nine (14.5%) surgeries consisted in dearterialisation only. That was the case of patients with grade I and II haemorrhoids, which had rectal bleeding as a very predominant symptom. In the remaining 406 (85.4%) patients, an associated mucopexy was performed with six continued sutures, as explained above. Another technique was associated due to a concurrent disease, fissure or skin tag removal in 28 (5.9%) patients. A marker point was used in 163 (34.3%) cases.
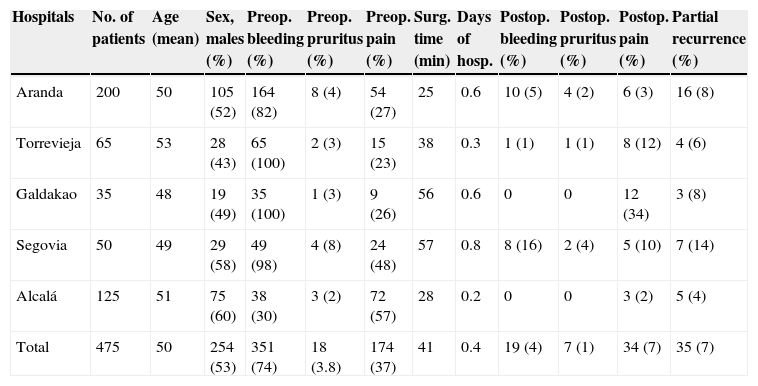
The overall data are shown in Table 1. The analysis of preoperative and postoperative symptoms showed statistically significant differences. Thus, there was an improvement in bleeding (P<.03) and pruritus (P<.04). Seventeen (4%) patients experienced postoperative pain for more than eight days. Analgesia was required for a total of 8.8±2.7 days and it corresponded to class I according to the WHO scale (acetaminophen and NSAIDs). The VAS for postoperative pain was 3.9±1.1 in a scale from 1 to 10. There was a recurrence rate of 7.4% (35 patients); recurrences were partial in all cases and related to grade III and IV haemorrhoids, without significant predominance throughout the follow-up period. The mean follow-up was 23.7±12.9 months. The mean hospital stay was 0.4±0.3 days. The use of laxatives was not recommended per protocol. Days off from work were 11.8±5.2 days.
Overall Results by Hospital.
| Hospitals | No. of patients | Age (mean) | Sex, males (%) | Preop. bleeding (%) | Preop. pruritus (%) | Preop. pain (%) | Surg. time (min) | Days of hosp. | Postop. bleeding (%) | Postop. pruritus (%) | Postop. pain (%) | Partial recurrence (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aranda | 200 | 50 | 105 (52) | 164 (82) | 8 (4) | 54 (27) | 25 | 0.6 | 10 (5) | 4 (2) | 6 (3) | 16 (8) |
| Torrevieja | 65 | 53 | 28 (43) | 65 (100) | 2 (3) | 15 (23) | 38 | 0.3 | 1 (1) | 1 (1) | 8 (12) | 4 (6) |
| Galdakao | 35 | 48 | 19 (49) | 35 (100) | 1 (3) | 9 (26) | 56 | 0.6 | 0 | 0 | 12 (34) | 3 (8) |
| Segovia | 50 | 49 | 29 (58) | 49 (98) | 4 (8) | 24 (48) | 57 | 0.8 | 8 (16) | 2 (4) | 5 (10) | 7 (14) |
| Alcalá | 125 | 51 | 75 (60) | 38 (30) | 3 (2) | 72 (57) | 28 | 0.2 | 0 | 0 | 3 (2) | 5 (4) |
| Total | 475 | 50 | 254 (53) | 351 (74) | 18 (3.8) | 174 (37) | 41 | 0.4 | 19 (4) | 7 (1) | 34 (7) | 35 (7) |
Alcalá: Hospital Universitario Príncipe de Asturias [Príncipe de Asturias University Hospital] (Alcalá de Henares, Madrid); Aranda: Hospital Santos Reyes [Santos Reyes Hospital] (Aranda de Duero, Burgos); Galdakao: Hospital de Galdakao [Galdakao Hospital] (Biscay); Segovia: Complejo Asistencial de Segovia [Segovia Healthcare Complex]; Torrevieja: Hospital de Torrevieja [Torrevieja Hospital] (Alicante).
The data from this multicentre study based on 475 patients highlights a significant improvement in the overall postoperative versus pre-operative clinical outcomes. Beyond the improvement in bleeding and pain following surgery, special emphasis should be given to outcomes such as a short mean length of stay (0.4±0.3 days), good tolerance to this technique in terms of low rate of use of analgesics (around 8 days), as well as a rapid return to work (less than 12 days on average), all of them very important aspects nowadays.
Thomson's12 studies show that the superior haemorrhoidal (rectal) artery splits up into five branches to reach the haemorrhoidal bundles. Aigner13 has shown with Doppler ultrasound tests that the increased calibre and the arterial blood flow in the terminal branches are related to haemorrhoidal prolapse.
After Ratto et al14 demonstrated, using colour Doppler techniques, that the superior haemorrhoidal artery has six terminal branches located constantly at 1, 3, 5, 7, 9 and 11 o’clock in the lithotomy position, techniques used to occlude the arterial flow to the haemorrhoidal plexuses have been described, such as THD, associated, or not, with haemorrhoidopexy.3,15 The haemorrhoidal prolapse remains folded inside the anorectal canal and connective tissue is regenerated until it completely reduces the haemorrhoidal prolapse.16–18
We would like to highlight the minimum rate of complications with the THD technique in our experience; such complications are actually more related to the surgical team's experience. Even though the THD procedure could affect the anorectal function due to an altered rectal wall or anal stenosis, no abnormalities have been detected by manometry or ultrasound in published trials.11 All the patients in this series had normal defecation, in agreement with data published by other authors.19–21
A certain rate of failure with the dearterialisation technique alone has been published22 for grade IV haemorrhoids; therefore, a mucopexy of the prolapsed tissue was added in those cases. Some authors have seen good outcomes even in patients with Crohn's disease and grade III haemorrhoids.23,24
This study is not intended to compare excisional versus nonexcisional techniques, but the experience from independent trials favours the THD technique based on advantages in terms of postoperative pain, hospital stay, time off from work and postoperative complications.10,11,18
Due to the high incidence of haemorrhoidal disease in our setting, we are to treat each patient with the least aggressive while most effective method, bearing in mind the surgeon's experience. Although medical treatment and other non-aggressive techniques, such as Barron's rubber bands, should be the initial methods of treatment for most selected symptomatic patients with mild haemorrhoids, the haemorrhoidopexy and dearterialisation technique may be used in a high number of patients with elevated rates of permanent healing of haemorrhoidal disease.
Even though this study includes a large sample size and was conducted by medical teams from different hospitals, outcomes were sufficiently homogeneous. Nevertheless, randomised trials are required to confirm and improve the efficacy and safety of the THD technique as an alternative to excisional techniques.
In summary, Doppler-guided THD associated with haemorrhoidopexy is a readily reproducible and safe technique that is widely accepted by patients due to its very low morbidity rate, low postoperative pain, rapid return to work, and low recurrence rate, as recorded in this multicentre study.
Conflict of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Noguerales F, Díaz R, Salim B, Piniella F, Landaluce A, Garcea A, et al. Tratamiento de la enfermedad hemorroidal mediante desarterialización y hemorroidopexia. Experiencia de varias unidades especializadas. Cir Esp. 2015;93:236–240.
A preliminary study corresponding to the experience at the Hospital Universitario Príncipe de Asturias (Prince of Asturias University Hospital) was presented at the XIV National Meeting of Coloproctology (Badajoz, 2010) and the XI National Congress of the Cuban Society of Surgery (Havana, 2010).