Dyslipidemia is a significant contributor to the elevated CVD risk observed in type 2 diabetes mellitus. We assessed the prevalence of dyslipidemia and its association with glucose metabolism status in a representative sample of the adult population in Spain and the percentage of subjects at guideline-recommended LDL-C goals.
Material and methodsThe di@bet.es study is a national, cross-sectional population-based survey of 5728 adults.
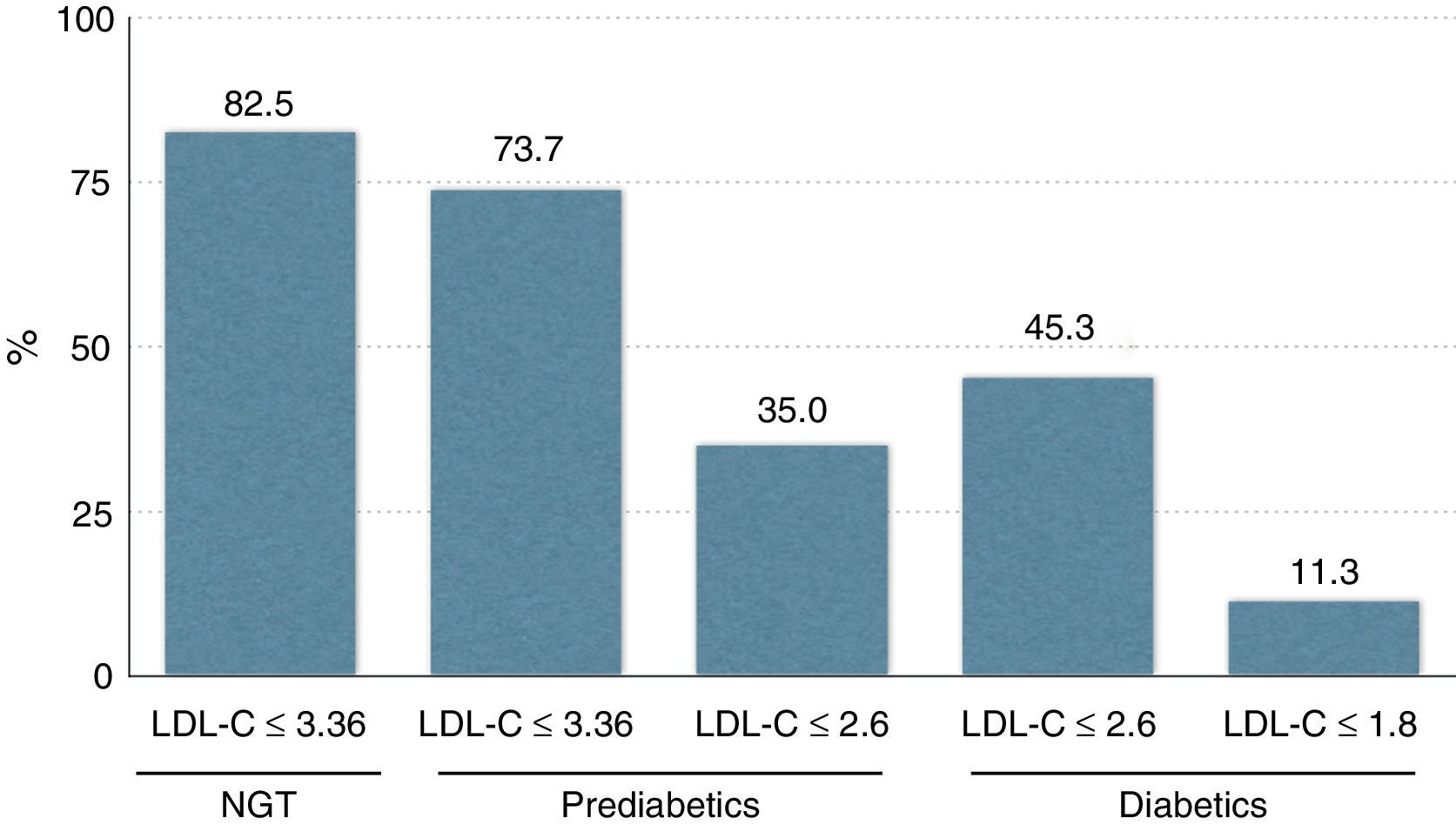
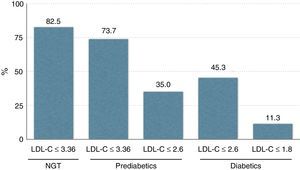
ResultsA total of 4776 subjects were studied. Dyslipidemia was diagnosed in 56.8% of subjects; only 13.2% of subjects were treated with lipid lowering drugs. Lipid abnormalities were found in 56.8% of Spanish adults: 23.3% with high LDL-C, 21.5% high TG, 35.8% high non-HDL-C, and 17.2% low HDL-C. Most normal subjects showed an LDL-C≤3.36mmol/l. Pre-diabetics presented similar proportion when considering a goal of 3.36mmol/l, but only 35% of them reached an LDL-C goal≤2.6mmol/l. Finally, 45.3% of diabetics had an LDL-C≤2.6mmol/l, and only 11.3% achieved an LDL-C≤1.8mmol/l.
ConclusionsOur study demonstrates a high prevalence of dyslipidemia in the adult Spanish population, and a low use of lipid-lowering drugs. Moreover, the number of subjects achieving their corresponding LDL-C goal is small, particularly in subjects at high cardiovascular risk, such as diabetics.
La dislipidemia es uno de los factores más importantes implicados en el riesgo de desarrollar enfermedad cardiovascular en la diabetes tipo 2. En el presente estudio evaluamos la prevalencia de dislipidemia y su asociación con el metabolismo hidrocarbonado en una muestra representativa de población adulta española y el porcentaje de sujetos que alcanzaron el objetivo de cLDL.
Material y métodosEl estudio Di@bet.es está basado en los datos obtenidos de una encuesta nacional transversal en 5.728 adultos.
ResultadosSe estudiaron 4.776 sujetos. La dislipidemia fue diagnosticada en el 56,8% de los sujetos; solo el 13,2% de los individuos estaban en tratamiento con fármacos hipolipemiantes. Las alteraciones lipídicas se distribuyeron del siguiente modo: 23,3% tenían cLDL elevado, el 21,5% TG elevados, el 35,8% elevación de colesterol no HDL, y el 17,2% cHDL bajo. La mayor parte de los sujetos sanos tenían cLDL≤3,36mmol/l. Los individuos prediabéticos presentaron una proporción similar si consideramos como objetivo cLDL≤3,36mmol/l, pero solo el 35% de ellos alcanzaron un objetivo de cLDL≤2,6mmol/l. Finalmente, el 45,3% de los diabéticos tenían cLDL≤2,6mmol/l, y solo el 11,3% alcanzaron cLDL-C≤1,8mmol/l.
ConclusionesNuestro estudio demuestra una elevada prevalencia de dislipidemia en población adulta española, y un escaso uso de fármacos hipolipemiantes. Además, el número de sujetos que alcanzaron el objetivo de cLDL fue muy pequeño, especialmente en sujetos con elevado riesgo cardiovascular como los diabéticos.
Atherosclerosis and its clinical complication, cardiovascular disease (CVD), is one of the most important causes of death in developed and industrialized countries. Different parameters have been identified as risk factors for CVD, plasma lipid abnormalities being one of them.
The causal relationship between elevated plasma low density lipoproteins-cholesterol (LDL-C) levels and the risk of CVD is well established in diabetic and non-diabetic subjects.1 In the UK Prospective Diabetes Study (UKPDS23) the LDL-C concentration was the best predictor of myocardial infarction in diabetic subjects.2 The dyslipidemia of type 2 diabetes is characterized by low levels of high density lipoproteins-cholesterol (HDL-C), moderately raised triglycerides (TG) and the accumulation of cholesterol enriched remnant lipoprotein particles, while total and LDL-C concentrations generally reflect those of the background population.3,4 This type of dyslipidemia is a significant contributor to the elevated CVD risk observed in type 2 diabetes mellitus. Intervention studies with lipid-lowering agents have shown significant reductions in CVD morbidity and mortality in primary and secondary prevention in diabetic subjects.5 Thus, detection and control of dyslipidemia is of particular interest for preventive cardiovascular measures.6
The aim of this study was to assess the prevalence of dyslipidemia and its association with glucose metabolism in a representative sample of the adult population in Spain. In addition, we have evaluated what percentage of them was at guideline-recommended LDL-C goals.
MethodsPopulationThe di@bet.es study is a national, cross-sectional population-based survey of 5728 adults (41.6% men) aged ≥18 years old conducted in 2009–10 from all Autonomous Communities. The characteristics and the design of the study have been previously reported in detail.7
A cluster sampling design was used to select participants, forming a representative random sample of the Spanish population. Of the eligible adults, 55.8% attended examination; 9.9% were excluded by protocol (institutionalized, severe disease, pregnancy or recent delivery), giving a final sample of 5072 individuals. The present study was restricted to the 4776 persons (42.7% men) with complete lipid data.
Variables and proceduresParticipants were invited by mail and/or telephone call to attend an examination visit at their health centre. Information was collected using an interviewer-administered structured questionnaire, followed by a physical examination by a nurse, who prior to the study had undergone a specific training course in order to standardize procedures. Socio-demographical data were collected as was information on smoking, level of daily physical activity, and alcohol intake. Records on current medication were obtained, and drugs were identified by registered trade name. Weight, height, waist and abdomen circumferences, were all measured by standardized methods. Body mass index (BMI) was calculated as weight/height.2 BMI equal or higher than 30kg/m2 was considered obesity. Blood pressure was measured using a blood pressure monitor (Hem-703C, Omron, Barcelona, Spain) following instructions of manufacturer. Hypertension was defined as ongoing antihypertensive treatment or systolic BP ≥140 and/or diastolic BP ≥90mmHg. Two blood pressure readings were obtained and the average of them was used in the analyses.
In all participants, a fasting blood sample was withdrawn. Serum glucose, triglycerides, and cholesterol were measured enzymatically, and HDL-C by direct method on an Artchitect C8000 Analyzer (Abott Laboratories SA, Madrid, Spain). Samples were immediately centrifuged and stored at −18°C (15 days maximum) until shipment to the centralized biobank to be stored at −80°C for later analysis. Subjects with baseline capillary blood glucose levels lower than 7.8mmol/l (140mg/dl) and those not currently receiving treatment for diabetes underwent a standard OGTT.
The diagnosis of diabetes and of impaired glucose regulation (IGR) was based on plasma glucose results, using the 1999 World Health Organization criteria.8 IGR included: impaired fasting glucose (IFG), impaired glucose tolerance (IGT) and IFG+IGT, and known and unknown diabetes mellitus.
The diagnosis of dyslipidemia was based on the presence of at least one of the following criteria: LDL-C≥2.6mmol/l in diabetics or ≥3.36mmol/l in non-diabetics; HDL-C≤1.0mmol/l; TG≥1.7mmol/l; non-HDL-C≥3.36mmol/l in diabetics or ≥4.14mmol/l in non-diabetics; use of lipid-lowering drugs.9 Only some subjects were aware of the presence of dyslipidemia (33%).
The study was approved by the Ethics and Clinical Investigation Committee of Carlos Haya Hospital (Málaga, Spain) in addition to other regional ethics and clinical investigation committees all over Spain and written informed consent was obtained from all participants.
Statistical analysisAll analyses were conducted using the SPSS 14 version (SPSS Inc.) and the results expressed as the mean±standard deviation (S.D.). We used parametric tests for the statistical analyses. For the comparison of means, we used the t-Student test to compare two variables or the ANOVA test for three or more variables. For the comparison of proportions, we used the Chi test. Correction for potential confounding variables was done. Significance was set at p<0.05 for two-tails.
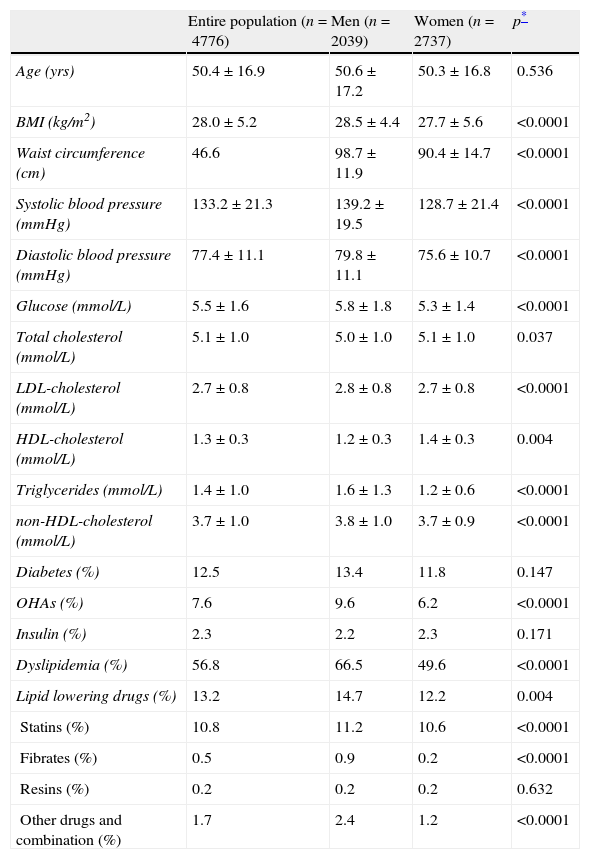
ResultsTable 1 shows the characteristics of the 4776 subjects (42.7% men) studied. There were no significant differences for age or diabetes prevalence between genders. Dyslipidemia was diagnosed in 56.8% of subjects; 13.2% of subjects (n=638) were treated with lipid lowering drugs, mostly statins, and have been analyzed separately from the 4138 individuals untreated with lipid-lowering agents.
Clinical characteristics of the di@bet.es study population included in this study.
| Entire population (n=4776) | Men (n=2039) | Women (n=2737) | p* | |
| Age (yrs) | 50.4±16.9 | 50.6±17.2 | 50.3±16.8 | 0.536 |
| BMI (kg/m2) | 28.0±5.2 | 28.5±4.4 | 27.7±5.6 | <0.0001 |
| Waist circumference (cm) | 46.6 | 98.7±11.9 | 90.4±14.7 | <0.0001 |
| Systolic blood pressure (mmHg) | 133.2±21.3 | 139.2±19.5 | 128.7±21.4 | <0.0001 |
| Diastolic blood pressure (mmHg) | 77.4±11.1 | 79.8±11.1 | 75.6±10.7 | <0.0001 |
| Glucose (mmol/L) | 5.5±1.6 | 5.8±1.8 | 5.3±1.4 | <0.0001 |
| Total cholesterol (mmol/L) | 5.1±1.0 | 5.0±1.0 | 5.1±1.0 | 0.037 |
| LDL-cholesterol (mmol/L) | 2.7±0.8 | 2.8±0.8 | 2.7±0.8 | <0.0001 |
| HDL-cholesterol (mmol/L) | 1.3±0.3 | 1.2±0.3 | 1.4±0.3 | 0.004 |
| Triglycerides (mmol/L) | 1.4±1.0 | 1.6±1.3 | 1.2±0.6 | <0.0001 |
| non-HDL-cholesterol (mmol/L) | 3.7±1.0 | 3.8±1.0 | 3.7±0.9 | <0.0001 |
| Diabetes (%) | 12.5 | 13.4 | 11.8 | 0.147 |
| OHAs (%) | 7.6 | 9.6 | 6.2 | <0.0001 |
| Insulin (%) | 2.3 | 2.2 | 2.3 | 0.171 |
| Dyslipidemia (%) | 56.8 | 66.5 | 49.6 | <0.0001 |
| Lipid lowering drugs (%) | 13.2 | 14.7 | 12.2 | 0.004 |
| Statins (%) | 10.8 | 11.2 | 10.6 | <0.0001 |
| Fibrates (%) | 0.5 | 0.9 | 0.2 | <0.0001 |
| Resins (%) | 0.2 | 0.2 | 0.2 | 0.632 |
| Other drugs and combination (%) | 1.7 | 2.4 | 1.2 | <0.0001 |
Untreated subjects n=4138 (1733 men/2405 women).
Data are expressed as mean±standard deviation.
OHAs: oral hypoglycemic agents.
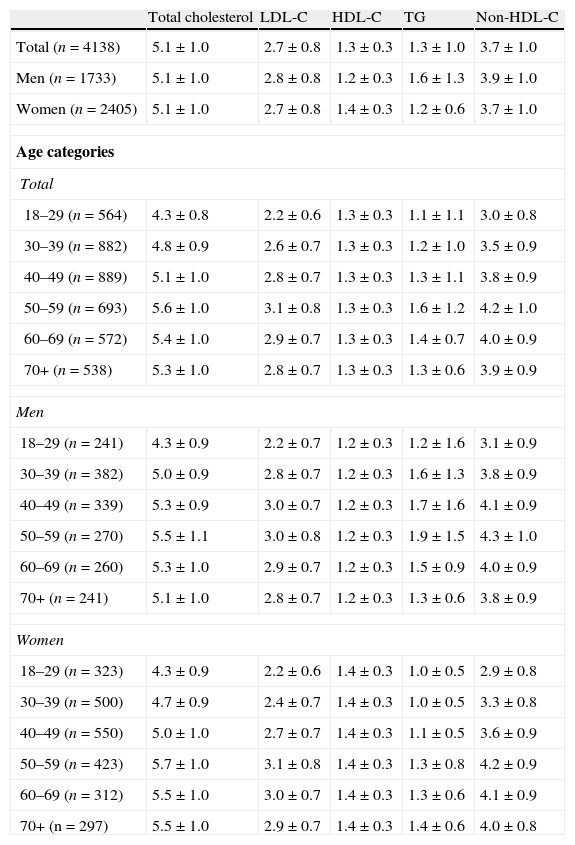
Lipid values in untreated subjects, according to age and gender, are shown in Table 2. Mean total plasma cholesterol, LDL-C, TG and non-HDL-C levels increased with age through middle age, reaching a peak at ages 50–59 years, and then decreasing in both genders. Men presented higher total cholesterol levels than women for ages 30–49 years but these levels were lower after age 50. A similar trend was found for LDL-C, TG, and non-HDL-C. On the contrary, at all ages men had lower levels of HDL-C compared to women, the values staying stable at all ages. The percentiles of lipid levels in untreated subjects, according to age and gender are shown online in Table 1.
Lipid values in untreated subjects (diabetics and non-diabetics) according to age and gender.
| Total cholesterol | LDL-C | HDL-C | TG | Non-HDL-C | |
| Total (n=4138) | 5.1±1.0 | 2.7±0.8 | 1.3±0.3 | 1.3±1.0 | 3.7±1.0 |
| Men (n=1733) | 5.1±1.0 | 2.8±0.8 | 1.2±0.3 | 1.6±1.3 | 3.9±1.0 |
| Women (n=2405) | 5.1±1.0 | 2.7±0.8 | 1.4±0.3 | 1.2±0.6 | 3.7±1.0 |
| Age categories | |||||
| Total | |||||
| 18–29 (n=564) | 4.3±0.8 | 2.2±0.6 | 1.3±0.3 | 1.1±1.1 | 3.0±0.8 |
| 30–39 (n=882) | 4.8±0.9 | 2.6±0.7 | 1.3±0.3 | 1.2±1.0 | 3.5±0.9 |
| 40–49 (n=889) | 5.1±1.0 | 2.8±0.7 | 1.3±0.3 | 1.3±1.1 | 3.8±0.9 |
| 50–59 (n=693) | 5.6±1.0 | 3.1±0.8 | 1.3±0.3 | 1.6±1.2 | 4.2±1.0 |
| 60–69 (n=572) | 5.4±1.0 | 2.9±0.7 | 1.3±0.3 | 1.4±0.7 | 4.0±0.9 |
| 70+ (n=538) | 5.3±1.0 | 2.8±0.7 | 1.3±0.3 | 1.3±0.6 | 3.9±0.9 |
| Men | |||||
| 18–29 (n=241) | 4.3±0.9 | 2.2±0.7 | 1.2±0.3 | 1.2±1.6 | 3.1±0.9 |
| 30–39 (n=382) | 5.0±0.9 | 2.8±0.7 | 1.2±0.3 | 1.6±1.3 | 3.8±0.9 |
| 40–49 (n=339) | 5.3±0.9 | 3.0±0.7 | 1.2±0.3 | 1.7±1.6 | 4.1±0.9 |
| 50–59 (n=270) | 5.5±1.1 | 3.0±0.8 | 1.2±0.3 | 1.9±1.5 | 4.3±1.0 |
| 60–69 (n=260) | 5.3±1.0 | 2.9±0.7 | 1.2±0.3 | 1.5±0.9 | 4.0±0.9 |
| 70+ (n=241) | 5.1±1.0 | 2.8±0.7 | 1.2±0.3 | 1.3±0.6 | 3.8±0.9 |
| Women | |||||
| 18–29 (n=323) | 4.3±0.9 | 2.2±0.6 | 1.4±0.3 | 1.0±0.5 | 2.9±0.8 |
| 30–39 (n=500) | 4.7±0.9 | 2.4±0.7 | 1.4±0.3 | 1.0±0.5 | 3.3±0.8 |
| 40–49 (n=550) | 5.0±1.0 | 2.7±0.7 | 1.4±0.3 | 1.1±0.5 | 3.6±0.9 |
| 50–59 (n=423) | 5.7±1.0 | 3.1±0.8 | 1.4±0.3 | 1.3±0.8 | 4.2±0.9 |
| 60–69 (n=312) | 5.5±1.0 | 3.0±0.7 | 1.4±0.3 | 1.3±0.6 | 4.1±0.9 |
| 70+ (n=297) | 5.5±1.0 | 2.9±0.7 | 1.4±0.3 | 1.4±0.6 | 4.0±0.8 |
Data are expressed as mean±standard deviation.
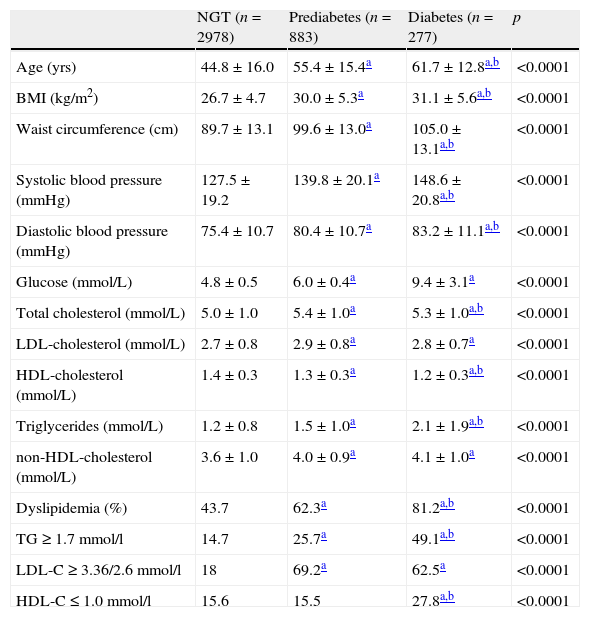
We have evaluated the relationship between glucose metabolism status and lipid values in untreated subjects (Table 3), separating them in three groups: normal glucose tolerance (NGT), prediabetes and diabetes. The prevalence of glucose impairment increased with age, and TG and non-HDL-C levels rose according to IGR, while HDL-C values decreased. Pre-diabetic and diabetic individuals had significantly higher levels of TC, LDL-C, TG and non-HDL compared to non-diabetic subjects. Moreover, diabetics had significantly higher levels of TG than pre-diabetics, and significantly lower levels of HDL-C. The prevalence of dyslipidemia increased progressively with rising glucose levels.
Clinical characteristics of the di@bet.es study population included in this study according to the glucose levels (untreated subjects).
| NGT (n=2978) | Prediabetes (n=883) | Diabetes (n=277) | p | |
| Age (yrs) | 44.8±16.0 | 55.4±15.4a | 61.7±12.8a,b | <0.0001 |
| BMI (kg/m2) | 26.7±4.7 | 30.0±5.3a | 31.1±5.6a,b | <0.0001 |
| Waist circumference (cm) | 89.7±13.1 | 99.6±13.0a | 105.0±13.1a,b | <0.0001 |
| Systolic blood pressure (mmHg) | 127.5±19.2 | 139.8±20.1a | 148.6±20.8a,b | <0.0001 |
| Diastolic blood pressure (mmHg) | 75.4±10.7 | 80.4±10.7a | 83.2±11.1a,b | <0.0001 |
| Glucose (mmol/L) | 4.8±0.5 | 6.0±0.4a | 9.4±3.1a | <0.0001 |
| Total cholesterol (mmol/L) | 5.0±1.0 | 5.4±1.0a | 5.3±1.0a,b | <0.0001 |
| LDL-cholesterol (mmol/L) | 2.7±0.8 | 2.9±0.8a | 2.8±0.7a | <0.0001 |
| HDL-cholesterol (mmol/L) | 1.4±0.3 | 1.3±0.3a | 1.2±0.3a,b | <0.0001 |
| Triglycerides (mmol/L) | 1.2±0.8 | 1.5±1.0a | 2.1±1.9a,b | <0.0001 |
| non-HDL-cholesterol (mmol/L) | 3.6±1.0 | 4.0±0.9a | 4.1±1.0a | <0.0001 |
| Dyslipidemia (%) | 43.7 | 62.3a | 81.2a,b | <0.0001 |
| TG≥1.7mmol/l | 14.7 | 25.7a | 49.1a,b | <0.0001 |
| LDL-C≥3.36/2.6mmol/l | 18 | 69.2a | 62.5a | <0.0001 |
| HDL-C≤1.0mmol/l | 15.6 | 15.5 | 27.8a,b | <0.0001 |
Data are expressed as mean±standard deviation.
Significant differences were maintained after adjustment by age.
LDL-C≥3.36mmol/l was considered for NGT; LDL-C≥2.6mmol/l was considered for prediabetes and diabetes.
The prevalence of dyslipidemia including the subjects using lipid-lowering drugs (n=4776) was: NGT (n=3273) 48.8%, prediabetes (n=1094) 69.5%, diabetes (n=409) 87.3%.
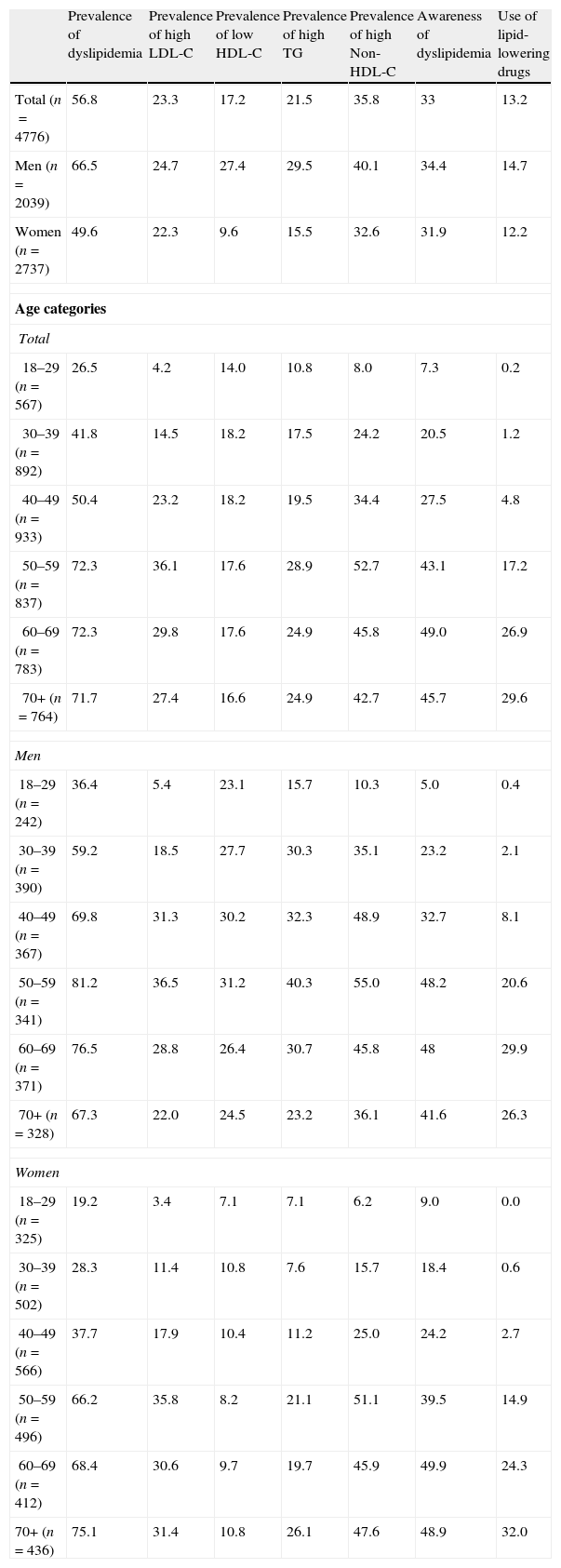
Table 4 shows the prevalence of dyslipidemia in the total group (treated and untreated subjects), the awareness of dyslipidemia and the percentage of subjects treated with lipid-lowering drugs. Lipid abnormalities were found in 56.8% of Spanish adults: 23.3% with high LDL-C; 21.5% high TG; 35.8% high non-HDL-C, and 17.2% had low HDL-C. The prevalence of dyslipidemia showed a tendency to rise with age, as well as the awareness and the percentage of subjects treated with lipid-lowering drugs. However, most of the subjects were unaware of the presence of dyslipidemia, and only a small proportion of those with known dyslipidemia were treated.
Prevalence of dyslipidemia, awareness and use of lipid-lowering drugs according to gender and age in the total population.
| Prevalence of dyslipidemia | Prevalence of high LDL-C | Prevalence of low HDL-C | Prevalence of high TG | Prevalence of high Non-HDL-C | Awareness of dyslipidemia | Use of lipid-lowering drugs | |
| Total (n=4776) | 56.8 | 23.3 | 17.2 | 21.5 | 35.8 | 33 | 13.2 |
| Men (n=2039) | 66.5 | 24.7 | 27.4 | 29.5 | 40.1 | 34.4 | 14.7 |
| Women (n=2737) | 49.6 | 22.3 | 9.6 | 15.5 | 32.6 | 31.9 | 12.2 |
| Age categories | |||||||
| Total | |||||||
| 18–29 (n=567) | 26.5 | 4.2 | 14.0 | 10.8 | 8.0 | 7.3 | 0.2 |
| 30–39 (n=892) | 41.8 | 14.5 | 18.2 | 17.5 | 24.2 | 20.5 | 1.2 |
| 40–49 (n=933) | 50.4 | 23.2 | 18.2 | 19.5 | 34.4 | 27.5 | 4.8 |
| 50–59 (n=837) | 72.3 | 36.1 | 17.6 | 28.9 | 52.7 | 43.1 | 17.2 |
| 60–69 (n=783) | 72.3 | 29.8 | 17.6 | 24.9 | 45.8 | 49.0 | 26.9 |
| 70+ (n=764) | 71.7 | 27.4 | 16.6 | 24.9 | 42.7 | 45.7 | 29.6 |
| Men | |||||||
| 18–29 (n=242) | 36.4 | 5.4 | 23.1 | 15.7 | 10.3 | 5.0 | 0.4 |
| 30–39 (n=390) | 59.2 | 18.5 | 27.7 | 30.3 | 35.1 | 23.2 | 2.1 |
| 40–49 (n=367) | 69.8 | 31.3 | 30.2 | 32.3 | 48.9 | 32.7 | 8.1 |
| 50–59 (n=341) | 81.2 | 36.5 | 31.2 | 40.3 | 55.0 | 48.2 | 20.6 |
| 60–69 (n=371) | 76.5 | 28.8 | 26.4 | 30.7 | 45.8 | 48 | 29.9 |
| 70+ (n=328) | 67.3 | 22.0 | 24.5 | 23.2 | 36.1 | 41.6 | 26.3 |
| Women | |||||||
| 18–29 (n=325) | 19.2 | 3.4 | 7.1 | 7.1 | 6.2 | 9.0 | 0.0 |
| 30–39 (n=502) | 28.3 | 11.4 | 10.8 | 7.6 | 15.7 | 18.4 | 0.6 |
| 40–49 (n=566) | 37.7 | 17.9 | 10.4 | 11.2 | 25.0 | 24.2 | 2.7 |
| 50–59 (n=496) | 66.2 | 35.8 | 8.2 | 21.1 | 51.1 | 39.5 | 14.9 |
| 60–69 (n=412) | 68.4 | 30.6 | 9.7 | 19.7 | 45.9 | 49.9 | 24.3 |
| 70+ (n=436) | 75.1 | 31.4 | 10.8 | 26.1 | 47.6 | 48.9 | 32.0 |
Data are expressed as percentage.
Fig. 1 shows the percentage of subjects in the total group reaching LDL-C goals according to their cardiovascular risk. Most of the NGT subjects achieved an LDL-C goal ≤3.36mmol/l. Prediabetics presented a similar proportion when considering a goal of 3.36mmol/l, but only 35% of them reached an LDL-C goal ≤2.6mmol/l. Finally, 45.3% of diabetics achieved an LDL-C ≤2.6mmol/l, but only 11.3% of them achieved an LDL-C goal ≤1.8mmol/l.
DiscussionIn a previous study, using a representative sample of the whole national population, the prevalence of diabetes mellitus in Spain was established at 13.8%, with 6.8% having undiagnosed diabetes that was discovered during the study.7 Diabetes is characterized by a clustering of cardiovascular risk factors. Of these, diabetic dyslipidaemia (increased levels of plasma triglycerides, low plasma levels of HDL-C, and elevated plasma levels of small dense LDL particles) is recognized as the most important modifiable risk factor for CVD in patients with diabetes.3,4 However, because of its asymptomatic nature the majority of individuals are unaware of it. Thus, early diagnosis and treatment of dyslipidemia is an important public health problem, particularly relevant in diabetic persons.
In the present study we have investigated the prevalence of lipid metabolism abnormalities detected in a sample representative of the adult population in Spain. Dyslipidemia was observed in 56.8% of the entire cohort, being more prevalent (66.6%) among men than in women (49.6%). Although both genders showed similar total cholesterol levels, men had higher LDL-C and TG levels, while women showed higher HDL-C. In both genders, total cholesterol and LDL-C levels increased with age, reaching a peak at ages 50–59 years. Men presented higher LDL-C levels than women up to 50 years, but their levels became lower than in women after 60 years of age. This finding could be ascribed, among other causes, to lower lipid levels in pre-menopausal females.10 Similar results were found for TG. On the contrary, HDL-C levels were higher in women at all ages. Our results are similar to that previously found by others in Spanish population.11 Moreover, although plasma lipid levels may vary in different cultures, our results are consistent with those found in other populations.10,12–14
Hyperglycemia and dyslipidemia are two of the most important risk factors for cardiovascular disease. Our study, in accordance with others15 showed that when untreated subjects were separated according to their glucose metabolism status, those with NGT showed the lowest prevalence (48.8%) of dyslipidemia, compared with the 69.5% found in prediabetes and the 87.3% found in diabetes. As expected, our study confirms the strong association of diabetes with elevated triglyceride levels, 49.1% of diabetic subjects had plasma TG levels ≥1.7mmol/L compared with 25.7% and 14.7% in the prediabetics and NGT groups, respectively. Moreover, the lipid profile in prediabetics included more abnormalities than in NGT subjects, as has been shown by other authors.15
Concerning LDL-C concentrations, the mean value in diabetic and prediabetic subjects was 2.8 and 2.9mmol/L, respectively, significantly higher than the 2.7mmol/L observed in NGT subjects. Although plasma LDL-C levels in IGR subjects are either normal or only modestly elevated, the LDL particle is smaller, carries less cholesterol and is denser. This profile of lipid abnormalities is referred to as diabetic dyslipidemia and contributes to the increased risk of atherosclerotic cardiovascular disease characteristic of type 2 diabetes.3,5 Our results are in accordance with those reported by Vinagre et al.16 in type 2 diabetes patients in Catalonia (Spain), with a mean LDL-C value of 2.9mmol/L, and the results of the DECODE Study15 which included subjects from 8 European communities.
With respect to HDL-C levels, plasma values are lower when glucose rises. Moreover, the prevalence of low-HDL-C was significantly higher in diabetics than prediabetics and NGT groups. However, there were no differences between the last two groups. A similar pattern was found in the DECODE study.15
We also evaluated the LDL-C goal attainment and the use of lipid-lowering drugs. Although epidemiological and interventional studies have shown a robust association between lipids and CVD, only 13.2% of subjects in our study were receiving treatment and only 33% of subjects were aware that they had dyslipidemia. These findings are similar to those reported in the 1999 to 2000 NHANES.17 Among treated subjects, statins were the lipid-lowering drugs most widely used (81.8%), with a therapeutic focus limited to LDL-C lowering. Lipid-lowering drugs prescriptions increased with age.
The percentage of subjects achieving LDL-C goals according to their cardiovascular risk varied according to the study groups. Most of the subjects with NGT, at low CVD risk, achieved an LDL-C goal ≤3.36mmol/l. However, in the two IGR groups, with higher CVD risk, the percentage of subjects who reached the LDL-C goal was lower. Although 73.7% of prediabetics attained an LDL-C goal ≤3.36mmol/l, only 35% of them achieved an LDL-C ≤2.6mmol/l. In spite of the elevated prevalence of dyslipidemia found in the diabetic group (87.3%) and the known high CVD risk in diabetics, only 32% of them were being treated with lipid-lowering agents. Consequently, the treatment targets were not reached in the majority of them. While 45.3% of diabetics reached an LDL-C ≤2.6mmol/l, only 11.3% were at the recommended ≤1.8mmol/l LDL-C goal. The degree of LDL-C goal achievement in diabetics was also low in other studies in Spanish population. In the DYSIS study, including individuals treated with statins at different doses, only 40.8% of diabetics achieved an LDL-C ≤2.6mmol/l.18 In the CODIMET study, diabetic individuals did not reach the recommended LDL-C target either. Only 37.6% presented an LDL-C ≤2.6mmol/l, and 13% achieved the LDL-C goal ≤1.8mmol/l.19
Although the di@bet.es study is a national, population-based survey, there are some limitations inherent to the design. It is a cross-sectional study and therefore it is not possible to evaluate factors affecting the prevalence and management of dyslipidemia. Moreover, the proportion of participants using lipid-lowering drugs could have been underestimated if participants failed to report their use. The proportion of subjects in secondary prevention was unknown. Thus the percentage of subjects achieving LDL-goals could be different. Finally, only the 55.8% attended examination.
Dyslipidemia is the most modifiable risk factor for atherosclerosis. Although diverse studies have shown that the prevalence of dyslipidemia has decreased in the last decades,12 our study demonstrates a high prevalence of dyslipidemia in the adult Spanish population, with a low use of lipid-lowering drugs. Moreover, the number of subjects achieving their corresponding LDL-C goal is small, particularly in subjects at high cardiovascular risk such as diabetics. Important efforts are necessary to implement control dyslipidemia and prevent CVD in our population.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors declare no conflict of interest.
This work was supported by CIBER de Diabetes y Enfermedades Metabolicas Asociadas (CIBERDEM). CIBERDEM is an Instituto de Salud Carlos III initiative.