To analyse the heart failure situation in a health area, as well quality criteria.
MethodCross-sectional observational study of patients diagnosed with heart failure by collecting data from their clinical history in the “Turriano” computer program. The variables analysed were, comorbidities, control of cardiovascular risk factors, treatments, number of chronic diseases, and admissions. The level of adherence to drugs in relation to heart failure by determining the ratio between the percentage of prescribed drugs and drugs withdrawn from pharmacy is also analysed using the Turriano prescription program. The study consisted of an improvement cycle or evaluative cycle, following the methodology proposed by Palmer to evaluate the quality of ambulatory care.
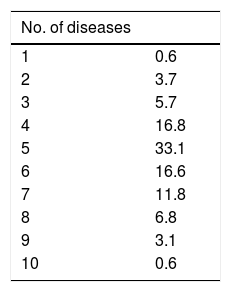
ResultsA total of 161 patients were included, with a mean age of 81.24 years, and 54.6% were women. Almost all of them (95%) had disease associated high blood pressure, including diabetes 42.2%, dyslipidaemia 8.9%, obesity 49.1%, and cancer 13.7% Some type of heart disease was diagnosed in 62.2% of patients with 29.2% ischaemic heart disease, 46.6% cardiac arrhythmias, and 20.5% valve diseases. More than 60% had between 4 and 6 concomitant diseases. An acceptable control is observed as regards the cardiovascular risk factors. Diuretic treatment was taken by 70%, with 32% and 35% taking angiotensin converting enzyme inhibitors and angiotensin II receptor antagonists. More than 20% have had 1–2 admissions in the last year, with cardiac decompensation being the main cause. There was 16% mortality.
ConclusionsPatients with heart failure have a significant number of chronic concomitant diseases, although there is an acceptable cardiovascular risk factors control. There are quality criteria that can be improved.
Análisis de situación de la insuficiencia cardiaca en una zona de salud y evaluación de criterios de calidad.
MétodoEstudio observacional transversal de los pacientes diagnosticados de insuficiencia cardiaca mediante historia clínica en el programa informático «Turriano». Se analizan las variables: comorbilidades, control de factores de riesgo cardiovascular, tratamientos, número de enfermedades crónicas e ingresos. También se analiza el grado de adherencia terapéutica para fármacos en relación con la insuficiencia cardiaca mediante la determinación del cociente entre el porcentaje de fármacos prescritos y el de fármacos retirados de farmacia, según el programa de prescripción de Turriano. El estudio consiste en un ciclo de mejora o ciclo evaluativo, siguiendo la metodología propuesta por Palmer para evaluar la calidad de la asistencia ambulatoria.
ResultadosSe incluyó a 161 pacientes, con una edad media de 81,24 años; un 54,6% eran mujeres. Las dolencias asociadas eran hipertensión arterial (95%), diabetes (42,2%), dislipidemias (8,9%), obesidad (49,1%) y neoplasias (13,7%). Un 62,2% tenían diagnosticado algún tipo de cardiopatía: el 29,2% cardiopatía isquémica, el 46,6% arritmias cardiacas y el 20,5% valvulopatías. Mas del 60% tenían entre 4 y 6 enfermedades concomitantes. En cuanto a los factores de riesgo cardiovascular, se observa un aceptable control. Un 70% tomaban tratamiento de diuréticos, un 32 y un 35% inhibidores de la enzima conversora de la angiotensina y antagonistas del receptor de la angiotensina II. Más del 20% han tenido 1-2 ingresos en el último año, con descompensación cardiaca como principal causa. Hubo un 16% de mortalidad.
ConclusionesLos pacientes con insuficiencia cardiaca tienen importante número de enfermedades crónicas concomitantes, si bien hay un aceptable control de los factores de riesgo cardiovascular.
Cardiovascular disease is still the leading cause of death in Spain, despite the constant development of new therapies and even improvements in the management of cardiovascular risk factors (CVRF). The fact is that both coronary heart disease mortality rates and chronic heart disease-related hospital admissions are unacceptably high.1 Although the patients themselves may be partly responsible for these figures (lack of adherence to treatment, unhealthy lifestyles, etc.), the truth is that the healthcare staff are largely responsible for this situation, and not because there is not enough information on the best course of action in each clinical situation (clinical practice guidelines, action protocols, etc.) or because doctors are not aware of such information, but because there are structural or physical deficiencies when it comes to enforcing such guidelines. Such deficiencies include the lack of efficient continuity of care. We can generally say that communication between the different levels of care (primary-hospital) could frankly be improved.1–4
It is widely accepted that heart failure (HF) is a common, fatal condition that is becoming more prevalent.4,5 Proof of this is the fact that it is the number one cause of hospital admissions among the elderly population, its incidence and prevalence increase with age,6–9 it is the third leading cause of cardiovascular death (accounting for 40% of remaining cardiovascular deaths after ischaemic heart disease and cerebrovascular accidents),7,8 and its 5-year mortality is 50%.6,9,10 Hospital readmission rates are high and are estimated to be around 30% within the first 6 months.11–13
HF causes considerable morbidity, with its associated costs, since many patients need frequent, long-term hospitalisation.14–16 In one study conducted in a Primary Care (PC) setting,17 HF was observed to have a more detrimental effect on quality of life than any other chronic disease. It therefore has such a poor prognosis that mortality rates in cases of severe HF are higher than for the most common types of cancer.6,7,18
Involving PC doctors in the management of HF, after consulting a specialist, is therefore of particular interest given their knowledge of the population concerned and of their cultural, social and economic differences. This population can also be actively involved in planning and managing the healthcare system to ensure better efficiency.19–22 It must also be considered that prevention is an essential part of the PC doctor's role,23 and the doctor must therefore be aware of those social factors that predetermine the disease. Such conceptualisations cause us once again to consider the PC professional as the main healthcare agent involved in the management of HF, which, given its chronic nature, requires ongoing care, which must be supported by relevant consultations and appropriate guidance from the Cardiology specialist. This is also the current situation in other countries, such as the United Kingdom, where most patients with HF are treated by their general practitioner (GP).24
HF patients have a higher risk of death and hospital admission and also experience significant deteriorations in quality of life, and their management is complex since they require constant treatment changes and dose adjustments and close monitoring. HF therefore requires management and follow-up and, consequently, coordination between PC and Cardiology.25–27
The objectives of this study are to analyse the HF management situation in our area in order to prepare an integrated hospital-PC quality continuous improvement programme to manage HF in a real-world practice setting in an urban integrated health area and to determine the impact of its implementation on mortality and readmissions among patients with HF.
MethodThe initial proposal was to conduct an observational, crossover study analysing the medical records of all patients over the age of 18 diagnosed with HF on the Turriano consultation software program used by PC within the Castille-La Mancha Health Service (SESCAM), which has access to the Cardiology medical records included on the Mambrino software via the clinical viewer.
A total of 161 cases of HF were detected among a population of 17,126 people over the age of 18 included within the primary health area.
Anthropometric variables (age, gender, weight, height, body mass index [BMI]), clinical variables (hypertension [HTN], diabetes, hyperlipidaemia, obesity, smoking, alcohol use, treatments, concomitant chronic diseases, diagnostic tests) and outcome variables (complications, number of admissions and even mortality) were analysed.
The study consisted of one improvement cycle or evaluation cycle, according to the methodology proposed by Palmer to evaluate the quality of outpatient care.
It was conducted during 2017 within the framework of PC, with the participation of ten doctors, three Family and Community Medicine residents from the PC team and one cardiologist from the area.
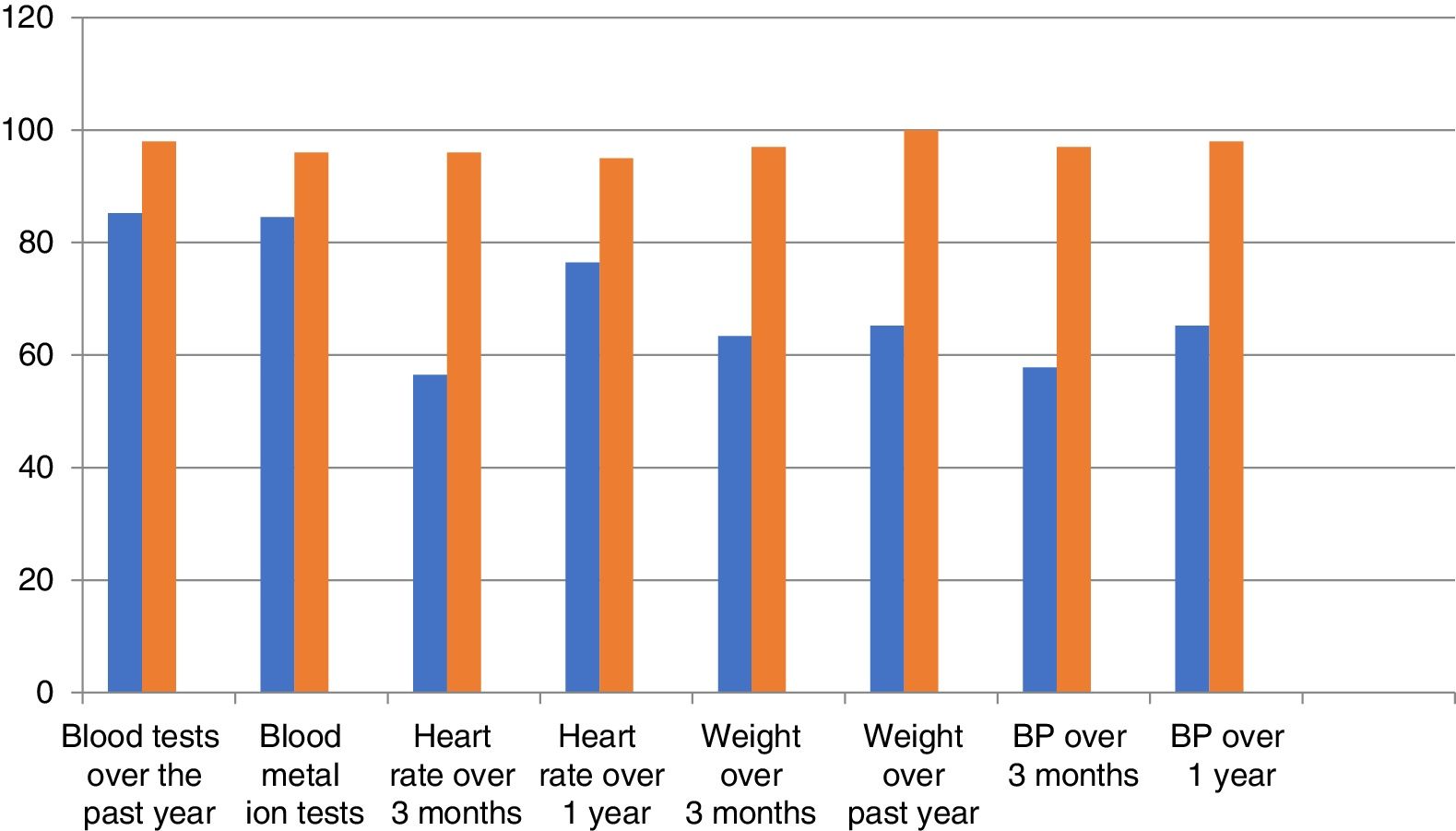
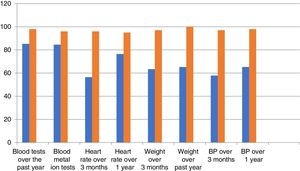
A total of 20 quality criteria were selected for the management of HF and their validity and reliability were confirmed using simple analyses of agreement and kappa indices, which were never less than 0.6. The following criteria were selected:
- 1.
The correct diagnosis and its cause according to the medical record.
- 2.
Concomitant chronic diseases.
- 3.
Diet recommendations.
- 4.
Exercise recommendations.
- 5.
Weight measurements over the past 3 months.
- 6.
Weight measurements over the past year.
- 7.
Blood pressure measurements over the past 3 months.
- 8.
Blood pressure measurements over the past year.
- 9.
Blood tests over at least the past year.
- 10.
Blood metal ion tests over the past year.
- 11.
Heart rate over the past 3 months.
- 12.
Heart rate over the past year.
- 13.
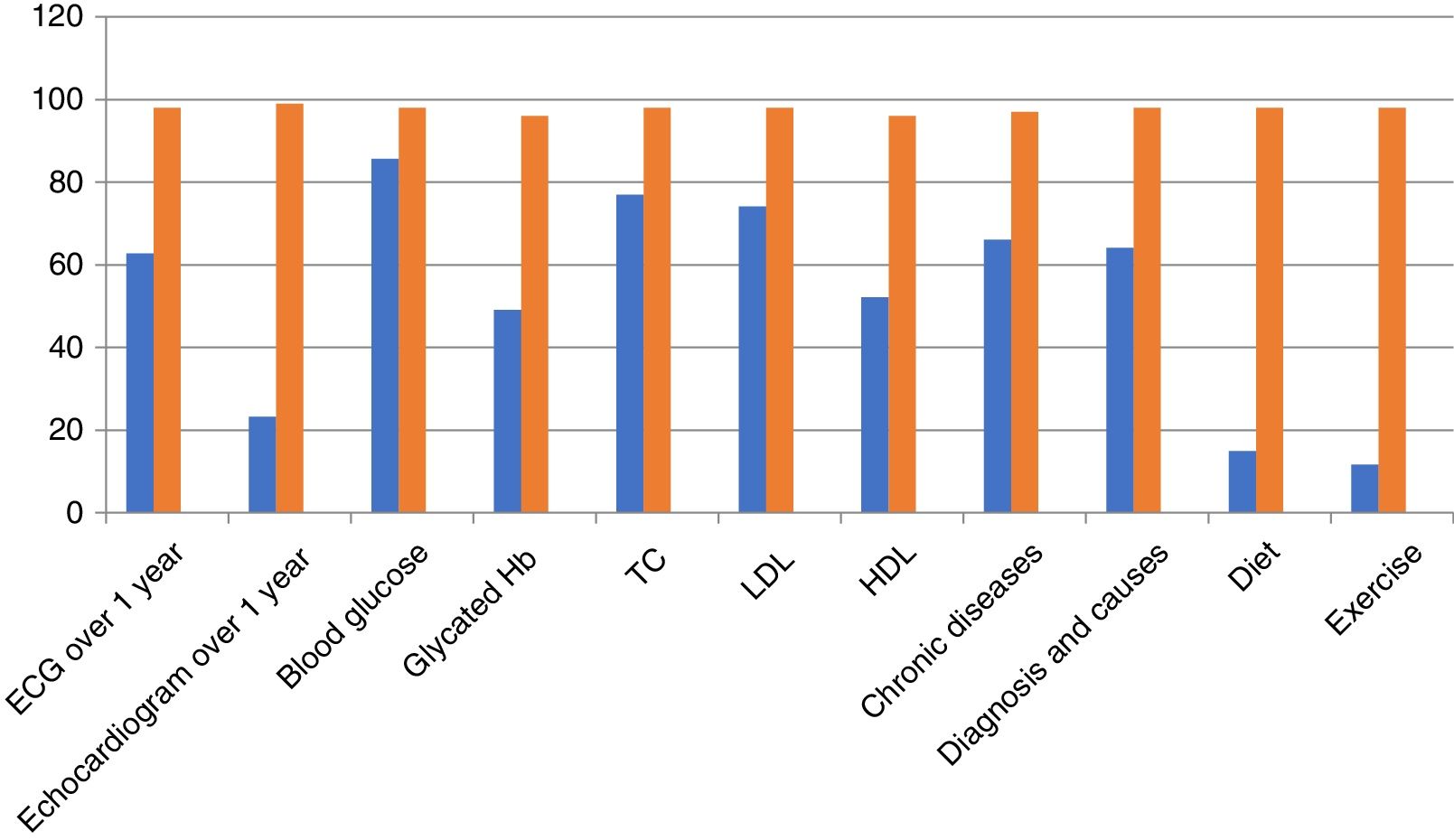
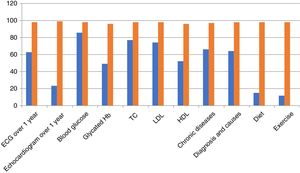
ECG over the past year.
- 14.
Echocardiogram over the past year.
- 15.
Control of cardiovascular risk factors: blood pressure.
- 16.
Control of cardiovascular risk factors: blood glucose.
- 17.
Control of cardiovascular risk factors: glycated haemoglobin.
- 18.
Control of cardiovascular risk factors: total cholesterol.
- 19.
Control of cardiovascular risk factors: triglycerides.
- 20.
Control of cardiovascular risk factors: LDL-C.
Adherence to HF-related medications was also analysed by determining the percentage of drugs prescribed to percentage of drugs dispensed ratio, according to the Turriano prescription software program.
Inclusion criteria: patients of both genders over the age of 18 with a diagnosis of HF in their clinical documentation between 01/01/2016 and 31/12/2017. Outpatients.
Exclusion criteria: patients under the age of 18. Pregnant women.
Sociodemographic and clinical variable data were collected for all patients on the case report form. A descriptive analysis of the sociodemographic and clinical characteristics of the study population was performed.
The results of the first evaluation were presented as rate of compliance with the different criteria, with a 95% confidence interval, and were plotted as bar charts.
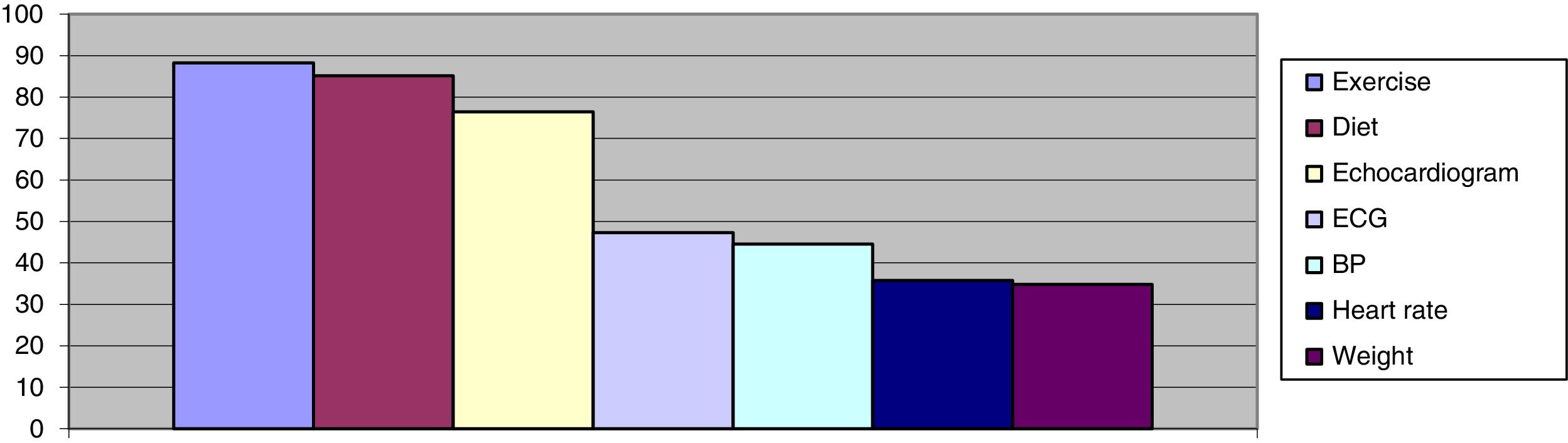
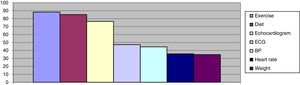
A Pareto chart, showing the degree of non-compliance with each of the criteria evaluated, and their cumulative relative frequency, was plotted.
Based on the data analysis obtained, an improvement intervention was designed as an affinity diagram, which was developed with the investigators at specific sessions scheduled for this purpose.
The data analysis was performed using the SPSS 21 statistical program.
ResultsA total of 161 patients diagnosed with HF in our health area took part in the study. The mean age was 81.24±9.59 years (maximum 100 and minimum 48) and 54% were women.
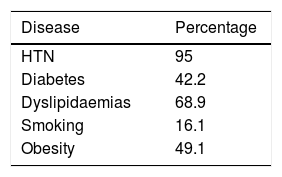
With regards to the prevalence of CVRF, the most common were hypertension followed by dyslipidaemias (Table 1).
Of the 62.2% of patients diagnosed with some kind of heart disease, 29.2% had coronary heart disease, 46.6% heart arrhythmias and 20.5% heart valve disease.
Patients with HF had a high number of concomitant chronic diseases, ranging between four and six in more than 60% of cases (Table 2).
Approximately 14% also had some kind of cancer.
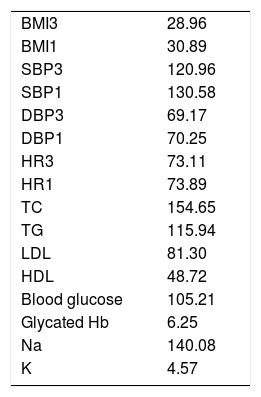
According to data obtained from examinations and blood tests, the main variables were acceptably controlled (Table 3).
Data from last consultation.
| BMI3 | 28.96 |
| BMI1 | 30.89 |
| SBP3 | 120.96 |
| SBP1 | 130.58 |
| DBP3 | 69.17 |
| DBP1 | 70.25 |
| HR3 | 73.11 |
| HR1 | 73.89 |
| TC | 154.65 |
| TG | 115.94 |
| LDL | 81.30 |
| HDL | 48.72 |
| Blood glucose | 105.21 |
| Glycated Hb | 6.25 |
| Na | 140.08 |
| K | 4.57 |
BMI1: body mass index over the past year; BMI3: BMI over the past 3 months; DBP1: diastolic blood pressure over the past year; DBP3: diastolic blood pressure over the past 3 months; Hb: haemoglobin; HDL: HDL cholesterol; HR1: heart rate over past year; HR3: heart rate over the past 3 months; LDL: LDL cholesterol; SBP1: systolic blood pressure over the past year; SBP3: systolic blood pressure over the past 3 months; TC: total cholesterol; TG: triglycerides.
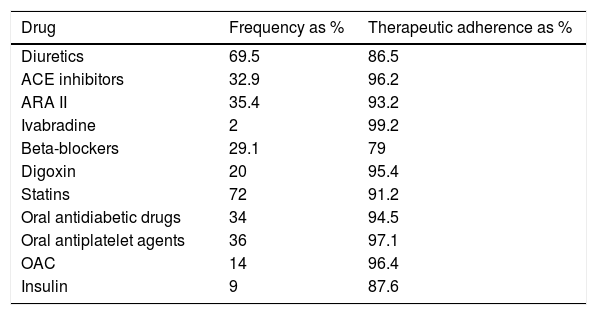
With regards to the treatments being taken, diuretics and statins were seen to be the most common, followed by ACE inhibitors and angiotensin-II receptor antagonists (ARA II). The results showed good adherence to treatment, with diuretics and insulin showing the worse level of adherence (Table 4).
Main treatments.
| Drug | Frequency as % | Therapeutic adherence as % |
|---|---|---|
| Diuretics | 69.5 | 86.5 |
| ACE inhibitors | 32.9 | 96.2 |
| ARA II | 35.4 | 93.2 |
| Ivabradine | 2 | 99.2 |
| Beta-blockers | 29.1 | 79 |
| Digoxin | 20 | 95.4 |
| Statins | 72 | 91.2 |
| Oral antidiabetic drugs | 34 | 94.5 |
| Oral antiplatelet agents | 36 | 97.1 |
| OAC | 14 | 96.4 |
| Insulin | 9 | 87.6 |
ACE inhibitors: angiotensin-converting enzyme inhibitors; ARA II: angiotensin-II receptor antagonists; OAC: oral anticoagulants.
A total of 34.25% of patients were admitted to hospital due to HF and, of these, 16.8% were admitted once, 7.5% were admitted twice, 3.7% were admitted three times and 5% were admitted 4–7 times.
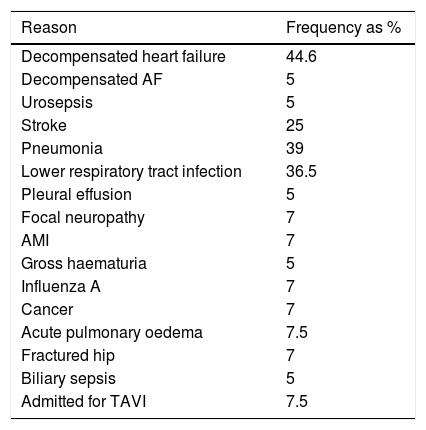
The main reasons for admission or readmission were decompensated heart failure, followed by pneumonia or lower respiratory tract infection (Table 5).
Reasons for admission.
| Reason | Frequency as % |
|---|---|
| Decompensated heart failure | 44.6 |
| Decompensated AF | 5 |
| Urosepsis | 5 |
| Stroke | 25 |
| Pneumonia | 39 |
| Lower respiratory tract infection | 36.5 |
| Pleural effusion | 5 |
| Focal neuropathy | 7 |
| AMI | 7 |
| Gross haematuria | 5 |
| Influenza A | 7 |
| Cancer | 7 |
| Acute pulmonary oedema | 7.5 |
| Fractured hip | 7 |
| Biliary sepsis | 5 |
| Admitted for TAVI | 7.5 |
ACE inhibitors: angiotensin-converting enzyme inhibitors; ARA II: angiotensin-II receptor antagonists; OAC: oral anticoagulants.
When testing the statistical association between variables, we can see a statistically significant relationship between age, gender and number of chronic diseases associated with a higher number of admissions and mortality (p<0.005).
With regards to compliance with the quality criteria selected:
Figs. 1 and 2, which show the degree of compliance with the criteria, reveal that the annual echocardiogram and diet and exercise recommendations are the criteria with the worst levels of compliance. It is also notable that the annual ECG or weight measurement, heart rate and even blood pressure measurements have relatively low compliance.
DiscussionHF is a common clinical syndrome involving various heart or systemic diseases. It is a complex clinical syndrome in which patients have typical symptoms (dyspnoea, ankle swelling, etc.) and signs (pulmonary rales, raised jugular venous pressure, etc.) as a result of structural or functional defects in the heart. It affects 1–2% of the adult population in developed countries. This percentage increases dramatically with age, reaching up to 10–20% among patients aged 70–80. This increase is related directly to longer life expectancy and improved survival of patients with heart disease. It is the leading cause of hospital admissions among individuals over the age of 65 and accounts for just over 2% of national healthcare expenditure.
This study shows an HF incidence of 1%, which, although in agreement with other published studies, is lower than that obtained in other national studies, which suggest incidence rates of 5%. This difference may be explained by underdiagnosis or poor diagnostic coding in medical records.1–3
These patients have a high incidence of HTN (95%) and heart disease (65%), which corresponds with existing pathophysiological theories which suggest that these two conditions damage the heart muscle, leading to HF.27,28
There is a statistically significant relationship between the number of chronic diseases and hospital admissions or mortality, which supports other studies showing high mortality rates and complex management of HF due to the frequency of comorbidities.
A total of 65% have between four and six associated chronic diseases: HTN (95%), diabetes (42.2%), dyslipidaemias (68.9%), smoking (16.1%), obesity (49.1%) and neoplasms (13.7%). These data confirm the study by Nagarajan,29 in which 40% of patients had five or more associated health issues that negatively affected their prognosis, the most important being: HTN (55%), diabetes (31%) and chronic obstructive pulmonary disease (26%). The following are also common: hypercholesterolaemia, atrial fibrillation, kidney failure, cerebrovascular disease and dementia.
While this study shows that 62.2% of patients have a diagnosis of heart disease (coronary heart disease (29.2%), heart arrhythmias (46.6%) and heart valve disease (20.5%)), other studies30,31 suggest that, in addition to heart disease and HTN, valve or congenital defects (10%) and cardiomyopathy (10%) are also causes of coronary heart disease. The remaining 10% corresponds to arrhythmias, conduction disturbances, high-cardiac output states (anaemia, sepsis, thyrotoxicosis, Paget's disease), drugs (some chemotherapy agents), toxins (alcohol, cocaine), infiltrative cardiac diseases (sarcoidosis, amyloidosis) and diabetes.
Acceptable control of CVRF was observed during the study: SBP (120.96), DBP (69.17), TC (154.65), TG (115.94), LDL (86), blood glucose (105.21), glycated Hb (6.25). Other studies, however, have shown worse control of HTN (59.7% have over 140/90) with 49% with LDL>130, 31.4% with HDL>31.4%, 12.3% smoking and 30.58% with BMI>30.
HF is a progressive, fatal disease, comparable to many neoplastic diseases, with decreased survival that is directly correlated with the degree of functional damage to the heart. Death is due to pump failure or ventricular arrhythmias. Nevertheless, scientific evidence has shown that disease progression can be delayed using therapeutic approaches based on the pathophysiology of HF. Consequently, effective treatment has achieved a relative reduction of 30–50% in hospital admissions over the past few years and a lower, but significant, reduction in mortality rates.
The treatments used depend on the pathophysiology of HF: diuretics (69.5%), ACE inhibitors (32.9%), ARA II (35.4%), ivabradine (2%), beta-blockers (29.1%) and digoxin (20%). High therapeutic adherence is also observed: 91.2% overall.
Relatively low compliance with the quality criteria is observed, with less than 20% compliance with diet or physical exercise recommendations. Compliance with weight measurements, heart rate and even blood pressure measurements is less than 60% and compliance with one echocardiogram per year is 22%.
HF programmes may vary both in terms of organisation and content. Instruments that allow the quality of such programmes to be evaluated and compared are therefore useful.31 The organisational models for the management of HF that have been most successful in improving results are those that focus on high-risk patients and include multidisciplinary interventions and integration between hospital and PC-based HF units, with specialised and community nursing playing a prominent role during the patient management and coordination process.
Once results have been analysed by the PC specialist and the cardiologist (Fig. 3), improvement lines for HF management are designed:
- –
More weight, height, BMI, heart rate and blood pressure measurements in the patient's medical records.
- –
More diet and physical exercise recommendations and improved logging in the patient's medical records.
- –
Increased use of flu and pneumococcal vaccines among this population.
- –
Improved PC-Cardiology Department relations by increasing means of communication:
- ∘
Direct contact by official email is established for sending data and queries regarding patients.
- ∘
Fast, online method of consultation with images.
- ∘
Communication via the department's internal phone network.
- ∘
Clinical sessions for prevention and early detection of decompensated HF in order to reduce admissions and mortality rates.
- ∘
HF is an entity with high morbidity and mortality rates and high hospital admission rates in our area. The quality of care for HF in our area has margin for improvement that would reduce admissions and mortality rates.
Conflicts of interestThe authors have no conflicts of interest.
Please cite this article as: Tárraga López PJ, Villar Inarejos MJ, Sadek IM, Madrona Marcos F, Tárraga Marcos L, Simón García MÁ. Calidad asistencial en el manejo de la insuficiencia cardiaca en una zona básica de salud. Clin Invest Arterioscler. 2018;30:258–264.