Obesity (OB), considered as one of the Non-Transmissible Chronic Diseases, has as its fundamental characteristics that of being prevalent at a global level, increasing in number, affecting developed and developing countries, affecting both genders, and all ages and social groups.
ObjectiveTo identify if high birth weight is a predictive factor (risk factor) for abdominal obesity in children 7–11 years old, and its relationship to gender and age.
MethodA case-control descriptive study was carried out with children born between January 1992 and December 1995, in order to identify early risk factors (atherosclerotic accelerators) such as abdominal obesity in children aged 7–11, and who have a history of macrosomia or high birth weight, as well as their relationship with gender and age.
ResultsIt was observed that the waist/height value was normal in 60.8% of the study group and in 64.00% in the control group. The difference between groups, gender, and age was not significant (p=0.6859). As regards the diet in the study group (macrosomic), there was no significant association between the type of diet and waist circumference/height values, with an χ2=0.223 and p=0.6373 (not significant). In the control group (with normal weight at birth), it was found that there is a significant statistical association between the type of diet and waist circumference/height values. This means that it can be stated, with 95% reliability, that the type of diet is associated with waist/height values.
ConclusionsHigh birth weight is not a predictive factor (risk factor) for abdominal obesity (increased waist/height index). Gender and age are independent for abdominal obesity (macrosomic and normal weight at birth). The diet in high birth weight children is not related to the index waist–height index, which is not the case in those born with normal weight under the same conditions. The marked increase in abdominal obesity (waist/height index) in children between 7 and 11 years old in both groups is worrying.
La obesidad (OB), considerada como una de las enfermedades crónicas no trasmisibles, tiene como características fundamentales la de ser frecuente a nivel global, ser cada vez más creciente, afectar a países desarrollados y en vías de desarrollo, afectar a ambos sexos, y a todas las edades y grupos sociales.
ObjetivoIdentificar si el alto peso al nacer constituye un factor predictor (factor de riesgo) para la OB abdominal en niños de 7 a 11 años, y su relación con el sexo y la edad.
MétodoSe realizó un estudio descriptivo con un diseño de tipo caso-control con los niños nacidos entre enero de 1992 y diciembre de 1995, con el fin de identificar de forma temprana factores de riesgo (aceleradores ateroscleróticos) como la OB abdominal en niños de 7 a 11 años, que tienen antecedentes de macrosomía o alto peso al nacer y su relación con el sexo y la edad.
ResultadosObservamos que en el grupo de estudio y en el grupo control el valor de cintura/estatura es normal, con un 60,80 y un 64,00%, respectivamente, estando alterado el 39,20% en el grupo de estudio y el 36,00% en el grupo de control, además de presentar una p=0,6859, no siendo estadísticamente significativo, comportándose de igual manera en ambos grupos, ocurriendo lo mismo con el sexo y la edad. En cuanto a la dieta en el grupo de estudio (macrosómico), no existe asociación significativa entre el tipo de dieta y los valores de circunferencia cintura/estatura, con un χ2=0,2223 y una p=0,6373 (no significativo). En el grupo control (con peso normal al nacer) encontramos que existe asociación estadística significativa entre el tipo de dieta y los valores de circunferencia cintura/estatura. Esto quiere decir que se puede afirmar con un 95% de confiabilidad que el tipo de dieta está asociado con los valores de cintura/estatura.
ConclusionesEl alto peso al nacer no constituye un factor predictor (factor de riesgo) para la OB abdominal (aumento del índice cintura/estatura). El sexo y la edad es independiente para la OB abdominal (macrosómico y peso normal al nacer). La dieta en el alto peso al nacer no está relacionada con el índice cintura/estatura, no ocurriendo así con los nacidos con peso normal en iguales condiciones. Preocupante el marcado aumento de la OB abdominal (índice cintura/estatura) en niños entre 7 y 11 años en ambos grupos.
The fundamental characteristics of obesity, considered as one of the chronic non-communicable diseases, are the fact that it is becoming increasingly more common worldwide, affecting developed and developing countries, both genders, and all ages and social groups.1–3 It is a global public health problem which respects only regions of extreme poverty with chronic food shortages, such as sub-Saharan Africa and Haiti. It is reported that, in 2005, more than 1600 million people >15-years-old were overweight or obese, according to the World Health Organization (WHO).
Traditionally, body mass index (BMI) is used to determine the nutritional status of a person or population. Although the criteria for adults are well-defined by the WHO, the diagnostic validity of BMI for the infant and adolescent population is surrounded by controversy.
In cases of overweight and obese individuals, BMI identifies excess weight, i.e. the excess weight for height, but it does not distinguish between the excess of fat-free mass (muscle and bone) and fat mass, which is what defines obesity.4
In the paediatric age group, waist circumference is a less-studied variable, although it has been demonstrated that it correlates significantly with BMI and fat percentage. It is clear that, during childhood, waist circumference increases naturally due to the growth process. However, the waist-to-height ratio remains stable. This eliminates the need to use standards with reference values for each age (as occurs in the case of BMI) and allows for the determination of a single cut-off point for each gender applicable to all ages.4
The waist-to-height ratio, which incorporates the measurement of the abdominal circumference and corrects it for height, would have a greater capacity for predicting cardiovascular risk factors related to body fat distribution, replacing BMI, both in adults and in children.5,6
Abdominal obesity is said to occur when intra-abdominal fat is equal to or greater than 130cm2. However, in clinical practice, the definition of central obesity is based on waist circumference, as there is a good correlation between waist circumference and intra-abdominal fat. Although there is no definitive consensus on the cut-off points, the values used most often are those proposed by the National Cholesterol Education Program (NCEP)-ATP-III.
Central obesity is of greater clinical significance than peripheral obesity, as intra-abdominal adipose tissue is metabolically more active than peripheral adipose tissue. Central obesity is an essential component of metabolic syndrome (MS) and a risk factor for the development of type 2 diabetes mellitus and cardiovascular disease.7
ObjectiveTo determine if macrosomia, or high birth weight, is a predictive factor (risk factor) for abdominal obesity (increased height-to-weight ratio) in children aged 7–11, and its relationship with gender, age and diet.
Methodological designMaterial and methodA case-control descriptive study was carried out with children born between January 1992 and December 1995, in order to identify at an early stage that they were affected with risk factors for atherosclerosis (accelerators of atherosclerosis), such as abdominal obesity in children aged 7–11, with a history of high birth weight (macrosomia) and its relationship with gender, age and diet. Variables such as birth weight, gender, age, abdominal circumference, height, waist-to-height ratio and diet (which we classified as balanced diet and unbalanced diet), were studied.
Population and sample sizeThe population was composed of all children born at the Hospital Ginecobstétrico Ramón González Coro from January 1992 to December 1995, belonging to the municipality Plaza de la Revolución, with a history of macrosomia, or high birth weight, and a sample was taken from this population. Probability techniques were not followed. They were therefore considered as an intention sample, and they were made up of a total of 140 children. Simultaneously, 100 children with a normal birth weight were studied, from the same municipality and born at the same hospital in the same time period. This group of children was considered as the control group. Each one of these children (macrosomic group and control group) were visited at their home to provide them with an appointment for a consultation in the Health Area (Policlínico Universitario 19 de Abril), where a thorough physical examination was performed which included a physical examination using a device, weight, height, abdominal circumference and diet, among others. The authorisation of the family members responsible for all the children investigated was sought (informed consent) for the conduct of this study, taking into account the following inclusion criteria:
- •
Resident in the municipality Plaza de la Revolución at the time of birth.
- •
Current resident in this municipality.
- •
Consent of a family member (responsible for the child) to participate in the study.
Waist-to-height ratio: continuous numeric variable, when its value is equal to or greater than 0.5cm it is estimated that abdominal obesity exists. It is independent of age and gender.
Variable diet: nominal category which is referred and accepted as synonymous with the dietary regime, which refers to the “group and quantities of food or mixtures of food products which are normally consumed” and we classify it as a balanced diet or unbalanced diet.
Balanced diet: this is when, for better digestion and metabolism, there should be a recommended proportion of food products which will simultaneously supply their nutrients. It is also mentioned that it should be in line with the age of the individual, habits, etc.
Techniques and procedures for data collection- •
Primary and secondary sources were used for the data collection.
- •
The interview and the observation were used as fundamental techniques in the data collection from primary sources.
- •
The book recording births at the Hospital Ginecobstetra Ramón González Coro, the hospital's medical history, the baby's birth card and card of the pregnant woman were the secondary data sources used.
- •
Each child was visited beforehand to provide him/her with an appointment time. A medical history with personal data, personal and family pathological history, dietary aspects, data related to the birth and a thorough physical examination, including an anthropometric study, was compiled at this visit.
School children aged 7–11 who were in primary education were studied in this investigation. Children with a birth weight of more than 3000g and less than 4000g made up the control group, and the macrosomic group was composed of children with a birth weight of 4000g or more.
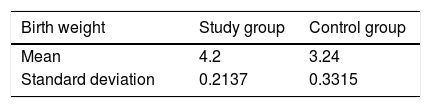
It can be observed in Table 1, regarding the mean and standard deviation of the birth weight in both groups, that there are highly significant differences between the average weights of the two groups. The average weights for the study group and the control group were 4.2 and 3.24, respectively.
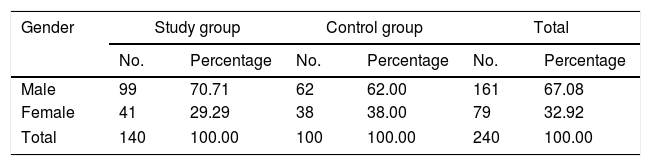
In Table 2, the population studied was represented by 140 macrosomic children, and the control group was represented by 100 children with normal birth weight, of whom 70.71 and 62.00% were male, 29.29 and 38.00% were female, respectively. There were no significant differences, i.e. the gender distribution behaved in a similar fashion in both groups (p=0.1660).
Distribution of the sample according to gender in the study group and in the control group.
| Gender | Study group | Control group | Total | |||
|---|---|---|---|---|---|---|
| No. | Percentage | No. | Percentage | No. | Percentage | |
| Male | 99 | 70.71 | 62 | 62.00 | 161 | 67.08 |
| Female | 41 | 29.29 | 38 | 38.00 | 79 | 32.92 |
| Total | 140 | 100.00 | 100 | 100.00 | 240 | 100.00 |
p-value=0.1660.
Source: MH at consultation.
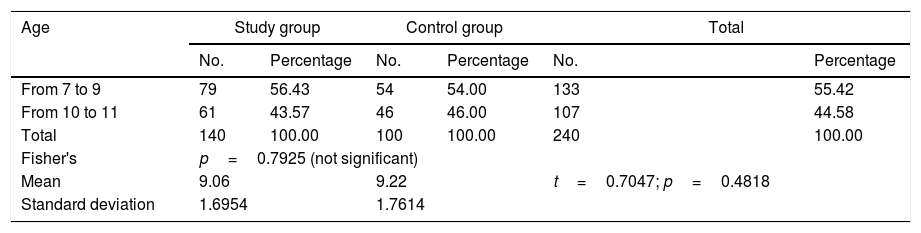
Table 3 presents the distribution of the sample and the control group according to age, finding between 7 and 9 years-old, 56.43% in the study group, 54.00% in the control group, and, in the age group from 10 to 11 years-old, 43.57% in the study group and 46.00% in the control group. There were no statistically significant differences between the two groups, as with the average age which is 9.06 for the sample and 9.22 for the control group.
Distribution of sample according to age in the study group and in the control group.
| Age | Study group | Control group | Total | |||
|---|---|---|---|---|---|---|
| No. | Percentage | No. | Percentage | No. | Percentage | |
| From 7 to 9 | 79 | 56.43 | 54 | 54.00 | 133 | 55.42 |
| From 10 to 11 | 61 | 43.57 | 46 | 46.00 | 107 | 44.58 |
| Total | 140 | 100.00 | 100 | 100.00 | 240 | 100.00 |
| Fisher's | p=0.7925 (not significant) | |||||
| Mean | 9.06 | 9.22 | t=0.7047; p=0.4818 | |||
| Standard deviation | 1.6954 | 1.7614 | ||||
Source: MH at consultation.
As can be observed in Tables 2 and 3, both gender and age in both groups is the same. There were no statistically significant differences, which shows uniformity between the two groups (study and control).
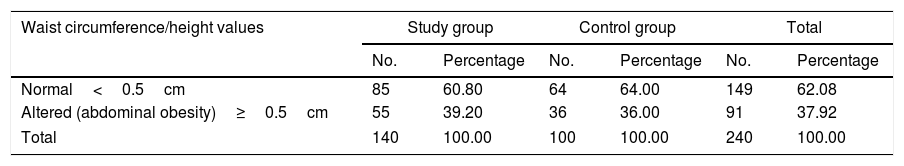
It can be seen in Table 4 that the waist-to-height ratio was normal in 60.80% in the study group and 64.00% in the control group, respectively. It was altered in 39.20% in the study group and in 36.00% in the control group, where a p-value of 0.6859 was observed, which was not statistically significant. It behaved in the same way in both the study group and the control group (high birth weight and normal birth weight), in terms of abdominal obesity (waist-to-height ratio).
Waist circumference/height values of the study group and the control group.
| Waist circumference/height values | Study group | Control group | Total | |||
|---|---|---|---|---|---|---|
| No. | Percentage | No. | Percentage | No. | Percentage | |
| Normal<0.5cm | 85 | 60.80 | 64 | 64.00 | 149 | 62.08 |
| Altered (abdominal obesity)≥0.5cm | 55 | 39.20 | 36 | 36.00 | 91 | 37.92 |
| Total | 140 | 100.00 | 100 | 100.00 | 240 | 100.00 |
p-value=0.6859 (not significant).
Source: MH at consultation.
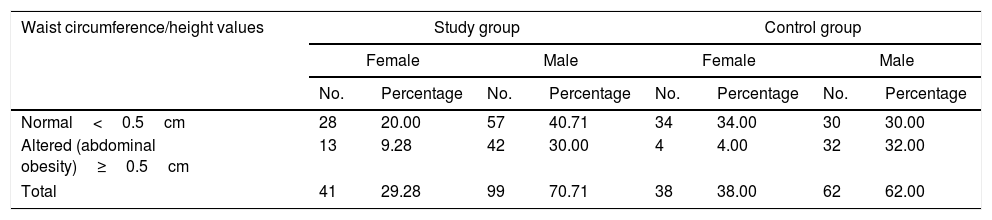
In Table 5, 9.28% of females and 30.00% of males in the study group had abdominal obesity. In the control group, 4.00% of females and 32.00% of males had abdominal obesity. There were no statistically significant differences in terms of gender in both groups, with a p-value of 1.5752.
Waist circumference/height and its relationship with gender in the study group and in the control group.
| Waist circumference/height values | Study group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||
| No. | Percentage | No. | Percentage | No. | Percentage | No. | Percentage | |
| Normal<0.5cm | 28 | 20.00 | 57 | 40.71 | 34 | 34.00 | 30 | 30.00 |
| Altered (abdominal obesity)≥0.5cm | 13 | 9.28 | 42 | 30.00 | 4 | 4.00 | 32 | 32.00 |
| Total | 41 | 29.28 | 99 | 70.71 | 38 | 38.00 | 62 | 62.00 |
p-value=1.5752 (not significant).
Source: MH at consultation.
In Table 6, regarding age, 25.00% of children aged 7–9 had abdominal obesity (waist-to-height ratio) in the study group and 21.00% in the control group. In children aged 10–11, 14.28% had abdominal obesity in the study group and 15.00% in the control group. It was not significant between both groups with a p-value of 0.7224.
Waist circumference/height and its relationship with age in the study group and in the control group.
| Waist circumference/height values | Study group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| From 7 to 9 | From 10 to 11 | From 7 to 9 | From 10 to 11 | |||||
| No. | Percentage | No. | Percentage | No. | Percentage | No. | Percentage | |
| Normal<0.5cm | 44 | 31.42 | 41 | 29.28 | 33 | 33.00 | 31 | 31.00 |
| Altered (abdominal obesity)≥0.5cm | 35 | 25.00 | 20 | 14.28 | 21 | 21.00 | 15 | 15.00 |
| Total | 79 | 56.42 | 61 | 43.57 | 54 | 54.00 | 46 | 46.00 |
p-value=0.7224 (not significant).
Source: MH at consultation.
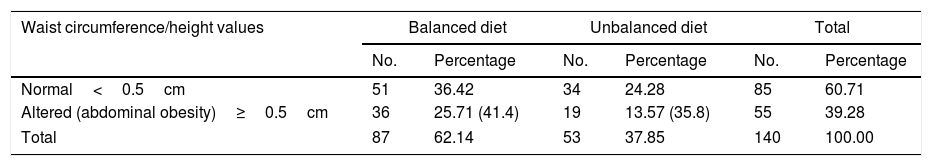
In Table 7, regarding diet in the study group (macrosomic), we found that the estimated prevalence of the condition (abdominal obesity, waist-to-height ratio) among those at risk (unbalanced diet) was 35.8%, and among those not at risk (balanced diet) it was 41.4%. There was no significant association between the type of diet and the waist circumference/height values, with a χ2 value of 0.2223 and a p-value of 0.6373 (not significant).
Waist circumference/height values and their relationship with diet in the study group.
| Waist circumference/height values | Balanced diet | Unbalanced diet | Total | |||
|---|---|---|---|---|---|---|
| No. | Percentage | No. | Percentage | No. | Percentage | |
| Normal<0.5cm | 51 | 36.42 | 34 | 24.28 | 85 | 60.71 |
| Altered (abdominal obesity)≥0.5cm | 36 | 25.71 (41.4) | 19 | 13.57 (35.8) | 55 | 39.28 |
| Total | 87 | 62.14 | 53 | 37.85 | 140 | 100.00 |
The estimated prevalence of the condition (abdominal obesity) among those at risk (unbalanced diet) is 35.8%, and among those not at risk (balanced diet) is 41.4%.
χ2=0.2223; p-value=0.6373 (not significant).
Source: MH at consultation.
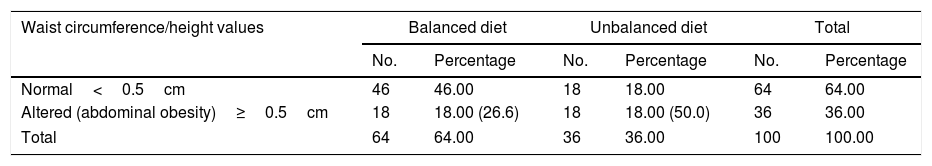
In Table 8 we found that there was a significant statistical association between the type of diet and the waist circumference/height values. This means that it can be stated, with 95% reliability, that the type of diet is associated with waist/height values in the control group (children with normal birth weight). The odds ratio (OR) was estimated at 2.76 with a 95% CI (Woolf's method) which goes from 1.17 (lower limit) to 6.51 (upper limit). The OR was statistically significant. It is interpreted as children with an unbalanced diet have a 2.76 times greater risk of having abdominal obesity than children with a balanced diet.
Waist circumference/height values and their relationship with diet in the control group.
| Waist circumference/height values | Balanced diet | Unbalanced diet | Total | |||
|---|---|---|---|---|---|---|
| No. | Percentage | No. | Percentage | No. | Percentage | |
| Normal<0.5cm | 46 | 46.00 | 18 | 18.00 | 64 | 64.00 |
| Altered (abdominal obesity)≥0.5cm | 18 | 18.00 (26.6) | 18 | 18.00 (50.0) | 36 | 36.00 |
| Total | 64 | 64.00 | 36 | 36.00 | 100 | 100.00 |
The estimated prevalence of the condition (abdominal obesity) among those at risk (unbalanced diet) is 50.0%, and among those not at risk (balanced diet) is 26.6%.
χ2=4.5807; p=0.0323 (statistically significant).
Source: MH at consultation.
The estimated prevalence of the condition (abdominal obesity) among those at risk (unbalanced diet) was 50.0%, and among those not at risk (balanced diet) it was 26.6%, with a χ2 value of 4.5807 and a p-value of 0.0323 (statistically significant).
DiscussionSchool children aged 7–11 who were in primary education were studied in this investigation, in which we observed that in their distribution both in their average age and in gender in both groups: macrosomic (high birth weight) and control (normal birth weight), there were no statistically significant differences.
It can be seen that, regarding the mean and standard deviation of birth weight in both groups, there are highly significant differences between the average weights of the two groups: study and control; with this being the study's objective.
Similar studies linked to the topic addressed in the investigation have been carried out in various parts of the world.
Childhood obesity is a significant public health problem, as has been mentioned, due to its prevalence and its consequences on life expectancy and quality of life in any country.8,9 One example is that a marked increase in the prevalence of obesity and in its comorbidity was observed in Chile between 1986 and 1998. There was an increase in obesity from 4.6 to 24.0% in prepubescent children and from 2.3 to 17% in pubescent children.10,11 A more atherogenic lipid profile was observed in both groups.
In the United Kingdom, in 2000, doctor Margaret Ashwell carried out a review of the evidence and recommended the use of a single cut-off point of 0.5 for males and females, regardless of their ethnic origin.12
Another study conducted in Chile on abdominal obesity (waist circumference >p90) was present in 76.3% of children and adolescents. We observed that its results were higher than those found in our study, which was 39.20% in the study group (macrosomic) and 36.00% in the control group. High birth weight was not taken into account in that study.
Data obtained in investigations carried out in the Universidad Autónoma de Baja California, Tijuana, Mexico in 2006 with a sample of 267 state schools for the study of obesity specifically in children between the ages of 6 and 12, showed that 45% of children (47% boys and 45% girls) were in the overweight (21.1%), obese (23.5%) and extremely obese (5%) categories, and 15% were in the abdominal obesity category,13 as we observed these results regarding abdominal obesity (waist-to-height ratio). In our study it was higher, although it was not indicated that these results were in high birth weight.
In Spain, in 2015 21.3% of children aged 6–11 and 14.3% of adolescents aged 12–17 had abdominal obesity, according to specialists at the Medical Research Institute (IMIM) of the Hospital del Mar. This study was the first to analyse abdominal obesity in Spanish children.14 These results do not match ours. Their results were higher in both groups (macrosomic and normal birth weight), which were 39.00 and 36.00%, respectively. In addition, they did not refer to high birth weight.
As we have already mentioned, central obesity has greater clinical significance than peripheral obesity, and we are always referring to this when we discuss obesity as intra-abdominal adipose tissue is metabolically more active than peripheral adipose tissue. Therefore, central obesity is an essential component of MS and, therefore, a risk factor for the development of type 2 diabetes mellitus and cardiovascular disease.7
For all these reasons, we believe that checking for these conditions is paramount in the paediatric age group to prevent the risk of developing type 2 diabetes mellitus, cardiovascular diseases and dyslipidaemia, among others, later in life.
The study that we present was the first on abdominal obesity in children aged 7–11 with a history of high birth weight.
We used the waist-to-height ratio as a measurement of abdominal obesity. This ratio is currently used in adults.
It was suggested that the risk of MS increases 17-fold in the presence of abdominal obesity. Several epidemiological studies show the link between abdominal adiposity and the greater risk of MS in childhood and in adolescence, and possibly of cardiovascular disease, dyslipidaemia and type 2 diabetes mellitus.15–18
The Heads of State and Government of the United Nations issued a statement at the meeting held on 19 and 20 September 2011 in which they indicated that chronic non-communicable diseases (CNCD) are one of the main obstacles to development in the 21st century. They agreed that CNCDs could undermine social and economic development worldwide, and that they did in fact put the achievement of internationally agreed development goals at risk.2
We should bear in mind that central obesity is more significant, as it releases fatty acids and cytosines which cause alterations in the lipid metabolism of carbohydrates. This facilitates insulin resistance. Central obesity is an essential component of MS and a risk factor for the development of type 2 diabetes mellitus and cardiovascular disease.7
Regarding the relationship of abdominal obesity with gender and age, we observed that its behaviour in both groups (macrosomic and control) is independent of gender and age. There were no differences between them, as has been suggested in studies carried out in India, which showed the superiority of the waist-to-height ratio in assessing individuals with cardiovascular risk factors and diabetes, regardless of gender, age and ethnic origin,19 although they did not collect data that were collected in this study in children with a high birth weight.
A child's diet at pre-school and school age is of vital importance as this is how adequate growth and development are ensured, bearing in mind the promotion of healthy eating habits to prevent nutrition disorders in the short and long term.
For this reason, it is important to maintain a balanced diet, to emphasise that all foods are necessary and to avoid sweets and junk food. Malnutrition, either due to insufficient intake or due to increased needs, may result in poor growth of a child. It is therefore important to monitor and control malnutrition.
Both the role of parents and the influence of teachers and of school canteens, which play a decisive role in the acquisition of healthy eating habits, is important.
All researchers on a balanced diet agree on the adequate results of this diet, once growth and development of the child has been achieved in line with each age.
The Recommended Dietary Allowances (RDA) were defined by the Food and Nutrition Board in 1941. The result of this work was the first edition of the RDAs which were published in 1943 and which attempted to determine “the nutritional standards to ensure a good state of health”. Given that the RDAs claim to be the foundation for assessing the correct diet of different population groups, it was necessary to review them periodically.20
Recently, the importance of the influence of the diet during the first years of life in the development and growth of a child, and its link to the prevention of chronic diseases in childhood and in adult life, has been highlighted.21
As is well-known, obesity in particular is one of the most significant emerging public health problems due to the fact it is a metabolic disorder which results in many risk factors (accelerators) for atherosclerosis and its epidemiological pattern is related most of the time to changes in eating habits and lifestyle, although other factors such as injuries in embryonic stages, etc. are cited.
However, in our research study, there was no relationship between high birth weight and the waist-to-height ratio with diet. This means that it can be stated reliably that the type of diet is not associated with waist/height values in the study group (macrosomics). This is contrary to the control group in which the diet was fundamental. It can therefore be stated, with 95% reliability, that the type of diet is associated with waist/height values in the control group.
We should point out that, so far, there are no known investigations on the waist-to-height ratio in high birth weight and its link to diet. This is an investigation which addresses one part of a major study on high birth weight and whether or not it can predict certain risk factors (accelerators) for atherosclerosis.
Conclusions- 1.
High birth weight is not a predictive factor (risk factor) for abdominal obesity (waist-to-height ratio), in children aged 7–11, as, according to the study conducted, statistically similar values were collected in both groups, with no significant differences.
- 2.
Gender and age are independent for abdominal obesity in both groups.
- 3.
Diet in high birth weight children is not related to the waist-to-height ratio, which is not the case in those born with normal weight (control group) under the same conditions.
- 4.
The marked increase in abdominal obesity (waist-to-height ratio) in children between 7 and 11-years old in both groups is worrying.
- 1.
It is necessary to take urgent measures against abdominal obesity regarding promotion and prevention at ages as young as childhood (>waist/height).
- 2.
The use of the waist-to-height ratio is important for the nutritional assessment in childhood, with the advantage of being independent of gender and age.
The authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez Vargas N, Fernandez-Britto JE, Martinez Perez TP, Martinez Garcia R, Castañeda Garcia CM, Garriga Reyes M, et al. Índice cintura/estatura en niños de 7 a 11 años con alto peso al nacer y su relación con el sexo, la edad y la dieta. Clin Invest Arterioscler. 2018;30:155–162.