Endometriosis is a chronic inflammatory disease that has been associated with an increased risk of ovarian cancer, especially epithelial tumors. Transvaginal ultrasound is a first-line diagnostic method for the assessment of endometriosis, and of endometriomas, the ovarian cystic form of endometriosis. Endometriomas usually have typical ultrasound features that allow them to be easily diagnosed. When atypical images are observed, such as solid areas with vascular flow, their malignancy should be ruled out, especially in peri-menopausal women. Early diagnosis of these tumors is essential because immediate surgical treatment is crucial for prognosis. Malignant neoplasms associated with endometriomas are, in the vast majority of cases, clear cell and endometrioid adenocarcinomas. In some cases seromucinous tumors have been described, but mainly in their borderline stage. A case is presented in which a patient developed an invasive seromucinous ovarian neoplasm on an endometrioma.
La endometriosis es una enfermedad inflamatoria crónica que se ha asociado con un mayor riesgo de cáncer de ovario, especialmente tumores epiteliales. La ecografía transvaginal es un método de diagnóstico de primera línea para la evaluación de la endometriosis y de los endometriomas, la forma quística ovárica de la endometriosis. Los endometriomas generalmente tienen características típicas ecográficas que permiten que se diagnostiquen fácilmente. Cuando presentan imágenes atípicas como áreas sólidas con flujo vascular, se debe descartar una neoplasia maligna, especialmente en mujeres perimenopáusicas. El diagnóstico precoz de estos tumores es esencial, porque el tratamiento quirúrgico inmediato es crucial para el pronóstico. Las neoplasias malignas asociadas con endometriomas son en la gran mayoría de los casos adenocarcinomas de células claras y endometrioides. En algunos casos se han descrito tumores seromucinosos, siendo principalmente tumores borderline, no invasivos. Presentamos un caso en el que una paciente desarrolló una neoplasia ovárica seromucinosa invasiva en un endometrioma.
Endometriosis is a chronic inflammatory disease defined by the presence of functional endometrial tissue outside of the uterus. It affects 10–15% of women in the reproductive age and usually appears along with painful symptoms, such as dysmenorrhoea, chronic abdominal and pelvic pain, and dyspareunia. Moreover, endometriosis can be a cause of infertility.1 Despite being a benign disease, it has been associated with a two to threefold increase in the risk of ovarian cancer.2 Endometriosis-associated ovarian cancer (EAOC) is mainly epithelial, especially clear cell carcinoma and endometrioid carcinoma and these are more likely to arise in ovarian than in extraovarian endometriosis. Other more uncommon neoplasms are mainly borderline but also invasive seromucinous tumors.3,4
Transvaginal ultrasound is the first-line approach for the evaluation and diagnosis of endometriosis. The most frequent ultrasound finding in endometriosis is ovarian cysts or endometriomas. Ultrasound appearance of a typical endometrioma presents like a thin-walled unilocular cystic lesion with homogeneous low-level echogenicity (ground glass feature). Sometimes endometriomas show atypical characteristics, with presence of solid components, solid papillary projections or mural nodules and specially the presence of color in the solid portion of the cyst and a color score 3 or 4. Despite the intrinsic difficulty of the visualization of these atypical characteristics, its identification is key because it could indicate the possible malignant transformation of the lesion. Performing an early diagnosis of high risk of malignancy is critical for a strict follow-up or, if appropriate, surgical intervention.5
We present a case in which a patient developed an invasive seromucinous tumor within an otherwise normal endometrioma. As far as we know only 10 cases are described based on the literature.5
Case reportA 45-year-old woman consulted in our department due to six months of cyclic abdominopelvic pain without dysmenorrhea or dyspareunia. Her clinical history was free of any gynecological pathology and the initial gynecological examination showed no significant alteration nor did the previous examinations.
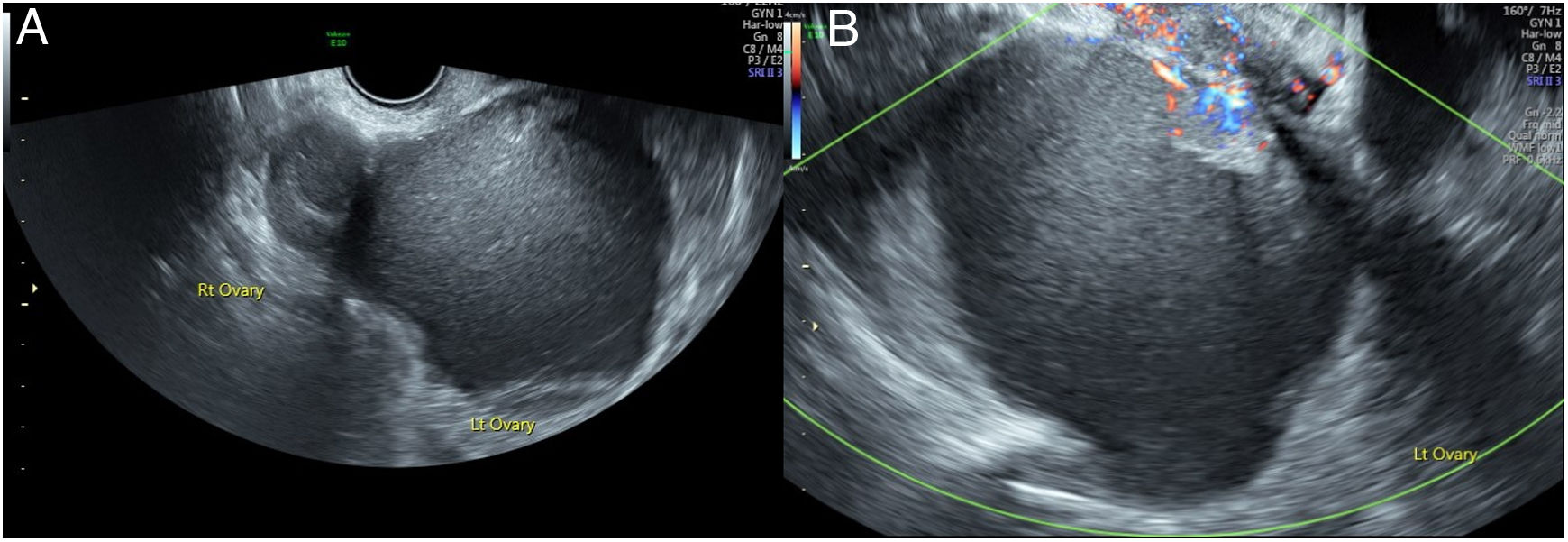
Vaginal ultrasound showed the right ovary of 37mm×23mm with a 24mm×17mm unilocular cystic image indicative of a typical endometrioma. The left ovary presented a retrouterine location and it was firmly attached to the contralateral ovary and to the posterior wall of the uterus, appearing the kissing ovaries sign. This ovary was occupied by a formation of 83mm×77mm×73mm with irregular border and ground glass content similar to an endometrioma. An area of greater echogenicity similar to a solid portion of 43mm×13mm with marked central vascular flow (Score 4 of the International Ovary Tumor Analysis -IOTA- group classification)6 was observed in the upper pole of the cyst. The formation did not show acoustic shadow and there was no free liquid in the Douglas pouch (Fig. 1A and B). Malignancy was suspected and the suspicion reinforced after the application of predictive models (54% malignancy risk with the logistic regression model LR2 of the IOTA group).7 A pelvic magnetic resonance reported the presence of bilateral endometriomas. Moreover, the report described a solid endocyst formation of 25mm×16mm, which seemed to infiltrate the adjacent cervix, at the base of the left endometrioma. Serum levels of biomarkers were slightly increased (CA 125: 52U/ml, CA 19.9: 45U/ml, HE-4: 138.8pmol/l).
(A) Transvaginal ultrasound showing a right ovary with a 24mm×17mm unilocular cystic image indicative of an endometriotic cyst. The left ovary is occupied by a formation of 83mm×77mm×73mm with irregular border, ground glass content and a solid portion at the upper pole. (B) Transvaginal ultrasound: central vascular flow (SCORE 3) in the solid portion of the cyst.
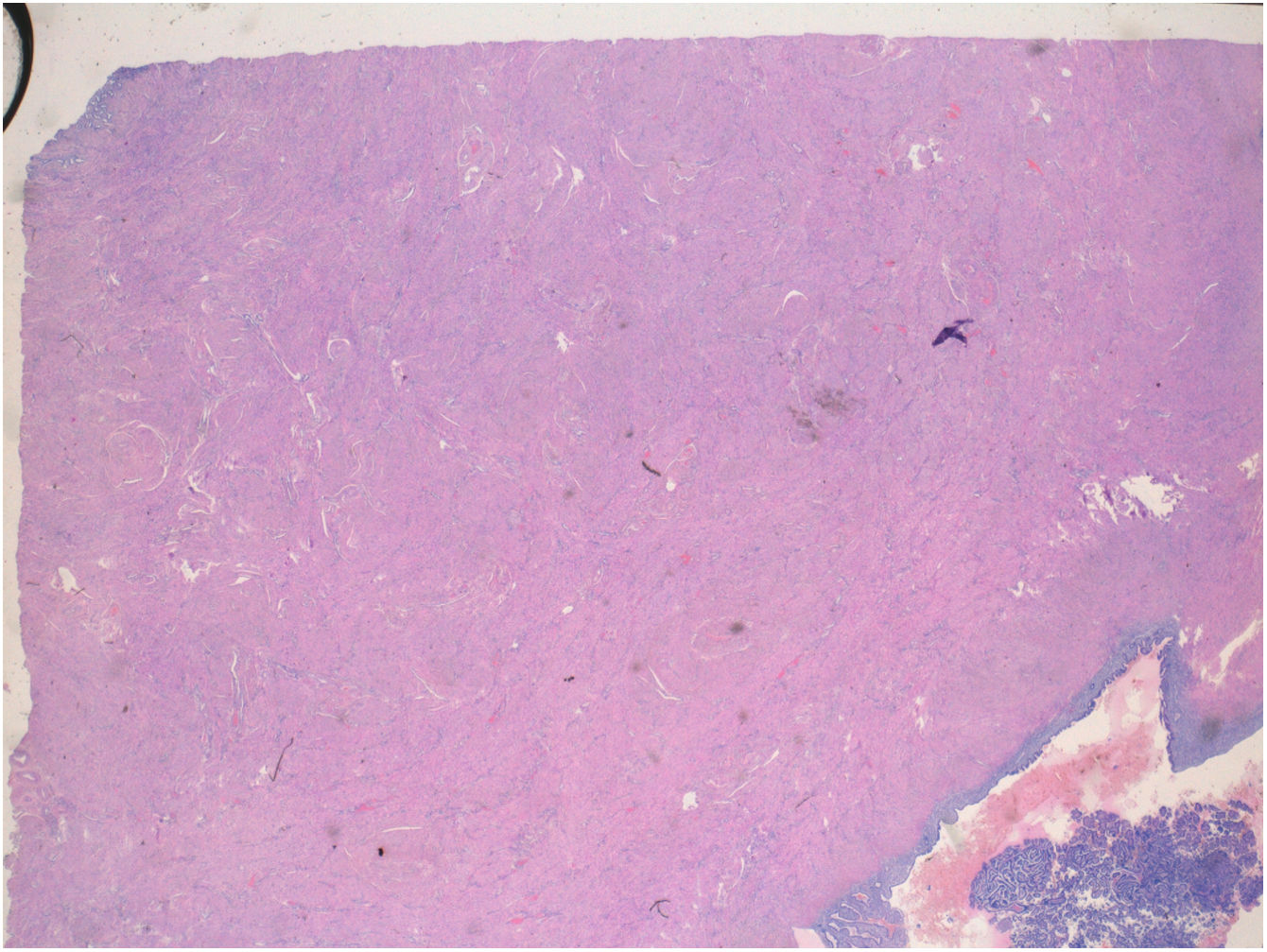
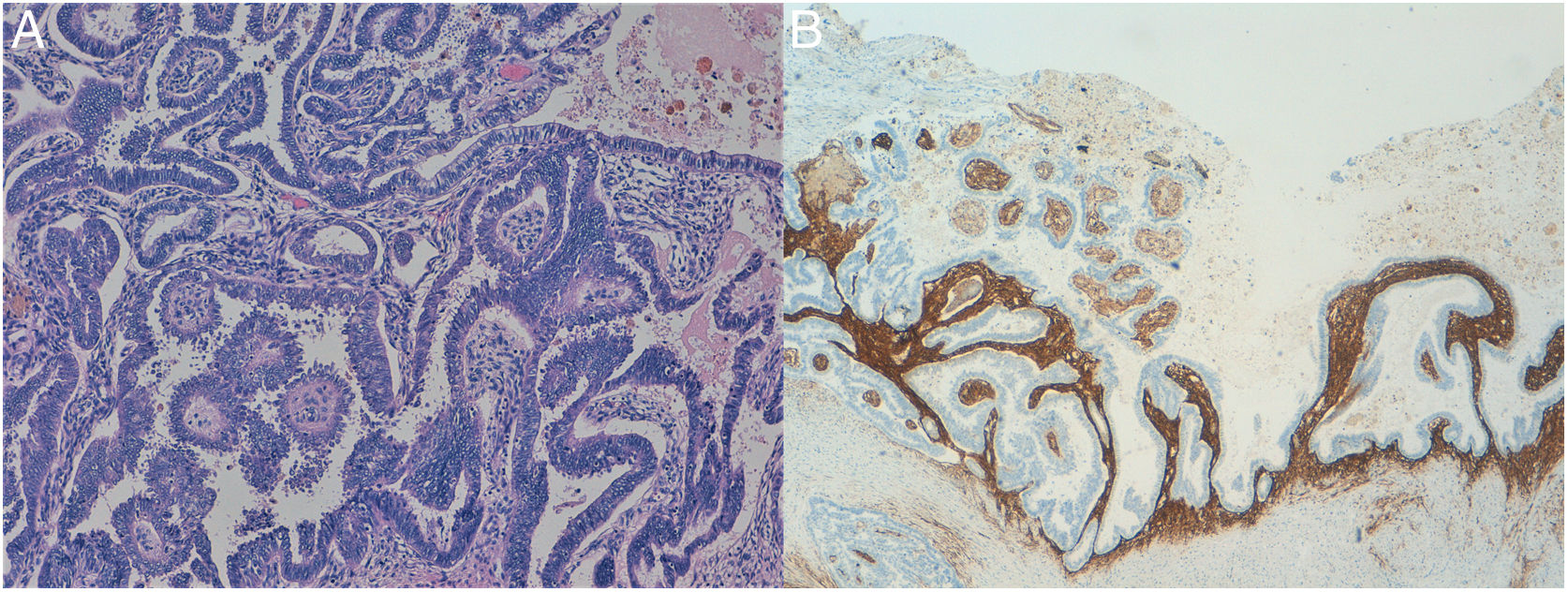
Considering the high probability of ovarian neoplasia, the patient underwent a hysterectomy along with bilateral adnexectomy by laparotomy. During the surgery, an endometrioma was observed in the right ovary and in the left one, a large complex cyst adhered to the posterior wall of the uterus. The content of these cyst was chocolate brown. Histological study reported a low-grade invasive müllerian seromucinous carcinoma developed on the left endometriotic cyst (Figs. 2 and 3A and B).
Ovarian cancer is the sixth most frequent cancer in European women. Both a high biological aggressivity and a considerable difficulty to diagnose in early stages condition a poor overall survival, which does not reach 40% at 5 years. These features convert ovarian cancer in the fifth cause of cancer death and the first among gynecological malignancies in European women.8
Endometriosis increases the risk for ovarian cancer in 0.5–1% and the standardized incidence ratio of ovarian cancer in women with endometriosis is 1.43–8.95.8,9 Of the EAOC, 80% are of epithelial origin, including clear cells carcinoma and endometrioid carcinoma and, exceptionally, seromucinous tumors.2 EOAC usually occurs in women over 40, in the form of tumors larger than 9cm. The prognosis is usually better than epithelial carcinoma not associated with endometriosis because 80% of cases are in stage I or II at the time of diagnosis.10 Seromucinous neoplasms are very rare within EOAC and so far they have been described only in their borderline stage (also called müllerian or endocervical-type mucinous borderline tumor), but not as invasive carcinomas as in this patient.11
Typical endometriomas features are easily detected by ultrasound, but endometriomas may also have atypical characteristics and they should be examined very closely due to its significant risk of malignancy, particularly if they appear in postmenopausal women. A unilocular-solid lesion with irregular wall and solid papillary projections with central vascular flow is highly suspicious.12 In our case, a perimenopausal woman presented an endometrioma of 83mm with atypical features consisting of a solid vascularized portion within the cyst with marked central blood flow (Score 4), so malignancy was suspected and immediate surgical treatment was performed.
Although atypical endometriosis should be suspected by ultrasound evaluation, it is definitely diagnosed on the basis of histological criteria. Considered as an intermediate step in the development of an ovarian neoplasm, atypical endometriosis shows molecular and inmunohistochemical alterations similar to those present in the ovarian tumors related to endometriosis.9 Seromucinous ovarian tumors resemble histologically to low-grade serous tumors. with a mucinous component (endocervical-like) associated to an important neutrophilic infiltrate and with areas similar to a cervical microglandular hyperplasia.13 Inmunohistochemical features include positivity to cytokeratin 7, “wild-type” p53 and hormonal receptors and negativity to cytokeratin 20 and cyclin-dependent kinase 2.14 In our case, the tumor exhibited epithelial changes of low-grade serous tumors and epithelial cells with cytoplasm occupied by large vacuole of the mucinous component. Immunohistochemistry confirmed positivity for estrogen-receptors and for p53. The pathologist concluded that it was a neoplasm with a papillary architecture whose histologycal characteristics were compatible with a seromucinous carcinoma developed on an endometriotic ovarian cyst.
This case highlights the importance of keeping in mind the risk of malignancy of usually benign ovarian masses such as endometriomas, and the need to perform an adequate diagnostic assessment. In this regard, clinical factors, like the age of the patient, together with a good ultrasound study of the lesion, should never be missed. The potential presence of a malignant neoplasm, therefore, should be always ruled out in women with endometriosis, and special attention should be paid to lesions with atypical ultrasound criteria. There is no recommendation to intervene prophylactically to women with ovarian endometriomas, but surgical treatment should be carried out in cases of suspected malignancy. These interventions cannot be delayed and should be performed by a team specialized in gynecological oncology.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Authors’ contributorsData collection, literature review and drafting of the manuscript, MG; Literature review and English translation, AG; Diagnosis and analysis of pathology, DM; Original proposer and proof, AC and JH. All authors read and approved the final manuscript.
Ethical considerationsThis study has not required approval from the Ethical Committee for Clinical Research as it does not involve the use of human subjects. Patient anonymity is maintained at all times without disclosing data about the patient.
FinancingNo funding was received from public agencies or other funding organisms.
Conflict of interestNone.