To analyze auditory processing test results in children suffering from otitis media in their first five years of age, considering their age. Furthermore, to classify central auditory processing test findings regarding the hearing skills evaluated.
METHODSA total of 109 students between 8 and 12 years old were divided into three groups. The control group consisted of 40 students from public school without a history of otitis media. Experimental group I consisted of 39 students from public schools and experimental group II consisted of 30 students from private schools; students in both groups suffered from secretory otitis media in their first five years of age and underwent surgery for placement of bilateral ventilation tubes. The individuals underwent complete audiological evaluation and assessment by Auditory Processing tests.
RESULTSThe left ear showed significantly worse performance when compared to the right ear in the dichotic digits test and pitch pattern sequence test. The students from the experimental groups showed worse performance when compared to the control group in the dichotic digits test and gaps-in-noise. Children from experimental group I had significantly lower results on the dichotic digits and gaps-in-noise tests compared with experimental group II. The hearing skills that were altered were temporal resolution and figure-ground perception.
CONCLUSIONChildren who suffered from secretory otitis media in their first five years and who underwent surgery for placement of bilateral ventilation tubes showed worse performance in auditory abilities, and children from public schools had worse results on auditory processing tests compared with students from private schools.
The auditory system consists of a set of structures that enables a person to receive and analyze sounds, and this system includes the sensory organ, the nervous system auditory pathways and the brain structures that are responsible for sound reception. While the peripheral auditory system receives and analyzes the acoustic waves emitted by vibrations in the environment, the central auditory system and the brain analyze the internal response for the acoustic stimulus, and a reaction is elicited (1).
The American Speech Hearing Association defined the term (Central) Auditory Processing, (C)AP, as the efficiency and effectiveness with which the central nervous system uses auditory information (2).
Conversely, (Central) Auditory Processing Disorder, (C)APD, refers to difficulties in the perceptual processing of auditory information in the central nervous system and the neurobiologic activity that gives rise to the electrophysiologic auditory potentials that are not related to changes in cognitive speech or other associated factors (2).
A previous study has shown that there is a correlation between otitis media events that occur during childhood and auditory perceptual changes, with increased risks of future speech deficits in children who experience otitis media events (1,3).
Otitis media is defined as inflammation of the middle ear and is often associated with an increase in the volume of infected fluid. This disease has several etiologic factors, such as infection (viral or bacterial), Eustachian tube dysfunction, immune status depression, upper respiratory tract infections, environmental problems and, in some cases, social problems (4). Inflammation is mostly seen in early childhood and decreases with age. About two-thirds of children have at least one episode of secretory otitis media (SOM) between 1 and 5 years of age. This condition is very common in young children due to the flattening of the Eustachian tube, which promotes recurring episodes of otitis media (5).
If medical intervention is not performed early enough, otitis media can cause hearing loss due to the accumulation of fluid in the middle ear, which makes the transmission of sound vibrations through the ossicular chain more difficult due to dissipation of sound energy. As a result, the child experiences mild or moderate conductive hearing loss, which is usually classified as fluctuating character (6).
In otitis media, even though periods of normal hearing may occur, its fluctuating character leads to inconsistent sound stimulation of the auditory central nervous system, thereby distorting sound perception. Speech discrimination, especially in noisy environments, and phonological awareness skills can also be affected and consequently negatively affect school performance (7,8).
Several studies have reported significant differences in phonological disorders in children with and without a history of otitis media. In general, children who suffer from otitis media had worse performance on tests of perception and auditory processing compared with children without otitis media and had a high incidence of academic problems, especially due to changes in reading and writing (9,10).
The standards for ear, nose and throat elective surgery were modified to consider the consequences of otitis media in childhood, especially in relation to the acquisition and development of speech skills. Surgery for ventilation tube placement, known as myringotomy, has become the most common procedure in small children, and in 1994 more than 500,000 children underwent surgery in the USA. This method is used to drain fluid from the middle ear and restore hearing (11,12).
However, a single surgical intervention for SOM is not sufficient to ensure adequate central auditory system stimulation. In addition to genetic factors, social factors, such as interactions between children and their parents, family and school, and behavioral factors, such as reading, listening to songs and attending theaters and parks, are needed to ensure cognitive and lingual development (13).
Several studies have shown that, compared with children who live in high-income households, children who live in low-income households have less cognitive development and lower school performance due to a deficiency of educational materials, appropriate role models and lack of parental help in perceptual, verbal and reading development (14,15).
Curi and Menezes-Filho (16) recognized that the choice of school depends on the family's income and the parents' educational level, as measured by the public's ability to send their children to a desired school. The authors found a correlation between parental education and school choice. In Brazil, 55% of private school students' parents have completed at least high school, compared with less than 20% of parents whose children attend public schools. Consequently, the socioeconomic status of children in private schools is higher compared with public schools.
In this context, socioeconomic status and family educational status are factors that can contribute to delays in the overall development of a child. These effects can be exacerbated, especially in children who have had multiple episodes of sensory deprivation hearing due to middle ear effusion (17).
Therefore, the objectives of this study were to analyze (C)AP test results in children who suffer from otitis media and underwent surgery for insertion of bilateral ventilation tubes considering gender and ear side (right ear (RE) and left ear (LE) and to classify the (C)AP test findings as auditory abilities.
MATERIALS AND METHODSThis experimental study was approved by the Faculty of Medical Sciences Ethics Committee at the University of Campinas (UNICAMP) under protocol number 682/2010.
Data were collected at the Audiology Study Center and Research in Rehabilitation under Professor Gabriel Porto (CEPRE).
SubjectsThe study included 109 elementary school students from public and private schools, consisting of 53 females and 56 males with ages between 8 and 12.
The subjects were divided into three groups: the control group (CG) comprised 40 students without a history of otitis media or school complaints, experimental group I (EGI) consisted of 39 students from public schools who suffered from SOM in their first 5 years and who underwent surgery for placement of bilateral ventilation tubes, and experimental group II (EGII) consisted of 30 students from private schools who suffered from SOM in their first 5 years and who underwent surgery for placement of bilateral ventilation tubes.
The criteria for inclusion in the CG were as follows: age between 8 and 12 years; acceptable results for otoscopy, audiometry and tympanometry tests; and no school complaints.
Inclusion criteria for EGI and EGII were as follows: age between 8 and 12 years; normal otoscopy, audiometry and tympanometry test results; history of SOM with surgical intervention for placement of bilateral ventilation tubes in the first 5 years of age; and absence of middle ear infection for 12 months prior to the date of assessment.
Children who had mental disorders, neurological disorders and/or genetic syndromes; were using psychoactive medications; attended phonotherapy; or did not fulfill the inclusion criteria were excluded from the sample.
ProceduresCG subjects were selected by the school's pedagogical coordinator, who analyzed the academic performance of children, and later by the researcher, who considered their otologic complaints.
EGI and EGII subjects who underwent surgery for placement of bilateral ventilation tubes at the State Hospital of Sumare and private clinics, respectively, were selected by the researcher through analyzing the medical records.
All selected subjects were invited to participate via telephone contact with their guardians, who also signed consent forms allowing their children to participate in the study.
The following procedures were performed: anamnesis (survey of the child's auditory history); basic hearing evaluation by pure tone audiometry and speech audiometry (speech recognition threshold (SRT) and phonemically balanced monosyllabic words (PB words); immittance (tympanometry and acoustic reflexes) and evaluation of the (C)AP; dichotic digits test (DD); pediatric speech intelligibility/synthetic sentence identification with ipsilateral competing message (PSI/SSI); pitch pattern sequence test (PPS); and gaps-in-noise (GIN).
The basic hearing evaluation was the first test to be performed. The criteria for normality were as follows: hearing thresholds up to 20 dB according to the classification of Davis and Silverman (18) and percentage of correct answers between 88 and 100% of PB words (1). Tympanometry was considered at its maximum peak compliance at an atmospheric pressure of 0 dPa, an equivalent volume between 0.3 and 1.3 ml and an acoustic reflex between 70 and 100 dB above the hearing threshold for pure tone, according to Jerger (19) and Carvalho (20).
After basic hearing evaluations, the subjects were submitted to the (C)AP.
The DD test allows us to evaluate the figure-ground ability for verbal sounds through a binaural integration task. The test performance and reference values were adopted according to the criteria proposed by Colella-Santos and Pereira (21).
The figure-ground ability was assessed by the PSI/SSI. The reference values and evaluation procedures were based on the Ziliotto (22) and Kalil (23) protocols. The tests that were applied varied depending on the children's age; the PSI test was used for children aged 8 to 11, and the SSI test was used for children aged 12.
Auditory temporal processing can be divided into four categories: ordination, integration, masking and temporal resolution. Temporal ordering and resolution were evaluated in this study.
The temporal ordering ability was assessed using the PPS described by Musiek (24) and adopting the values of normality published by Schochat and Rabelo (25).
The GIN test proposed by Musiek (26) was performed to evaluate temporal resolution ability by adopting the values of normality published by Perez (27) and Amaral and Colella-Santos (28).
The basic hearing evaluation and (C)AP were performed in a 60-minute session in a soundproof booth. An AC40 audiometer and earphones (model: TDH 39P) were used. Impedance was performed using 235 h immittance audiometry. All equipment was calibrated according to ISO-389 and IEC-645.
For the (C)AP tests, a CD player was linked to the audiometer to allow stimuli to be presented through the CD. The CDs were used according to the instructions on the Central Auditory Processing book - Evaluation Manual, Volume 1 and 2 for the DD tests and PSI/SSI (21–23). For the PPS and GIN tests, the CDs that were used were the versions proposed by Musiek (24,26).
Statistical analysis was performed using nonparametric methods; tables show average values, standard deviations and p-values. The significance level was 5% (p<0.05), and significant data are highlighted in bold.
To analyze student performance on (C)AP tests with respect to the RE and LE, the Wilcoxon signed-rank test was utilized. When p<0.05, the subsequent statistical analysis continued independently for each ear.
Regarding student performance on the (C)AP test, the Kruskal-Wallis test was used to analyze significance. When p<0.05, the Mann-Whitney test was utilized to compare groups in pairs.
To verify student performance in regard to hearing skills, a Chi-squared test was used to determine significance. Hearing abilities were classified as normal or altered according to the benchmarks for each test. When p<0.05, the odds ratio comparing groups was used to analyze differences.
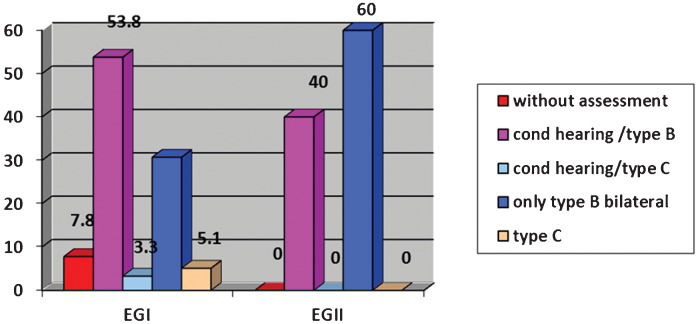
RESULTSFigure 1 shows the pre-surgical evaluations of tympanotomy tube placement for EGI and EGII.
Student performance on the (C)AP tests, for both the RE and the LE, is shown in Table 1. The results of (C)AP tests in regard to groups are shown in Table 2. The results of (C)AP tests of paired groups are shown in Table 3. Tables 4 and 5 show the comparisons between group performances, considering altered auditory skills.
Student performance on the (C)AP tests for the RE and LE.
| Right ear (n = 109) | Left ear (n = 109) | ||||||
|---|---|---|---|---|---|---|---|
| Tests | Average | SD | Median | Average | SD | Median | p-value |
| DD | 95.0 | 7.1 | 97.5 | 92.3 | 10.6 | 95.0 | 0.0001 |
| PPS | 61.6 | 24.6 | 63.3 | 58.7 | 25.6 | 57.0 | 0.0251 |
| GIN | 5.5 | 2.5 | 5.0 | 5.4 | 2.0 | 5.0 | 0.5453 |
| GINP | 70.8 | 14.2 | 73.3 | 70.6 | 12.8 | 72.0 | 0.7371 |
| PSI/SSI | 743.7 | 23.1 | 80.0 | 73.9 | 22.9 | 70.0 | 0.5473 |
n - number of subjects; SD - standard deviation; DD - dichotic digits; PPS – pitch pattern sequence test; GIN – gaps-in-noise; GINP – gaps-in-noise/percent; PSI/SSI - pediatric speech intelligibility/synthetic sentence identification with ipsilateral competing message. The p-value was calculated using the Wilcoxon paired test.
Student performance on (C)AP tests based on group.
| CG | EGI | EGII | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test | n | Average | SD | Median | n | Average | SD | Median | n | Average | SD | Median | p-value |
| DD | |||||||||||||
| RE | 40 | 97.9 | 3.3 | 100.0 | 39 | 91.3 | 9.5 | 95.0 | 30 | 95.8 | 4.9 | 97.5 | 0.0007 |
| LE | 40 | 96.7 | 5.5 | 100.0 | 39 | 86.6 | 14.4 | 90.0 | 30 | 93.9 | 5.6 | 95.0 | <0.0001 |
| PPS | |||||||||||||
| RE | 40 | 66.7 | 22.4 | 70.0 | 39 | 56.8 | 26.1 | 56.7 | 30 | 60.9 | 24.9 | 64.8 | 0.1742 |
| LE | 40 | 64.4 | 24.5 | 80.0 | 39 | 53.9 | 27.3 | 47.0 | 30 | 57.2 | 24.1 | 63.0 | 0.1732 |
| GIN | 80∗ | 5.1 | 2.6 | 5.0 | 78∗ | 6.1 | 2.0 | 6.0 | 60∗ | 5.2 | 1.8 | 5.0 | <0.0001 |
| GINP | 80∗ | 74.7 | 11.4 | 75.5 | 78∗ | 63.3 | 13.4 | 65.0 | 60∗ | 75.1 | 12.1 | 78.0 | <0.0001 |
| PSI/SSI | 80∗ | 78.4 | 19.9 | 80.0 | 78∗ | 73.6 | 23.5 | 70.0 | 60∗ | 69.8 | 25.4 | 75.0 | 0.1425 |
n - number of subjects/∗ number of ears; SD - standard deviation; DD - dichotic digits; RE - right ear; LE - left ear; PPS – pitch pattern sequence test; GIN – gaps-in-noise; GINP – gaps-in-noise/percent; PSI/SSI - pediatric speech intelligibility/synthetic sentence identification with ipsilateral competing message. The p-value was calculated by the Mann-Whitney test.
Student performance on the (C)AP tests between pairs of groups.
| p-value | p-value | p-value | |
|---|---|---|---|
| Tests | CG x EGI | CG x EGII | EGI x EGII |
| DD | |||
| RE | 0.0004 | 0.0567 | 0.0687 |
| LE | <0.0001 | 0.0060 | 0.0177 |
| GIN | <0.0001 | 0.1611 | 0.0068 |
| GINP | <0.0001 | 0.7123 | <0.0001 |
DD - dichotic digits; RE - right ear; LE - left ear; GIN – gaps-in-noise; GINP – gaps-in-noise/percent.
CG and EG performance based on the hearing skills that were evaluated.
| CG | EGI | EGII | p-value | ||||
|---|---|---|---|---|---|---|---|
| Hearing Skills | n | % | n | % | n | % | |
| Figure-ground | |||||||
| Normal | 35 | 87.5 | 19 | 48.7 | 15 | 50.0 | 0.0003 |
| Altered | 5 | 12.5 | 20 | 51.3 | 15 | 50.0 | |
| Temporal Ordering | |||||||
| Normal | 28 | 70.0 | 16 | 41.0 | 17 | 56.7 | 0.0345 |
| Altered | 12 | 30.0 | 23 | 59.0 | 13 | 43.3 | |
| Temporal resolution | |||||||
| Normal | 34 | 85.0 | 13 | 33.3 | 20 | 66.7 | <0.0001 |
| Altered | 6 | 15.0 | 26 | 66.7 | 10 | 33.3 | |
| All normal | 24 | 60.0 | 5 | 12.8 | 10 | 33.3 | <0.0001 |
n - number of subjects; % - percent. The p-value was calculated by the chi-squared test.
The temporary alteration in the peripheral auditory system due to otitis media changes the quality of sound perception once the acoustic signal can be observed in incomplete form (29).
Most subjects went through preoperative audiometric evaluation (Figure 1). For some subjects, only tympanometry was performed due to their age. In EGI, most of the children showed conductive hearing loss and type B tympanometric curves, while in EGII, most subjects showed bilateral type B tympanometric curves. The data corroborate the findings of Oliveira et al. (30), who identified the presence of conductive hearing loss by pre-surgical audiometry for subjects who had implanted ventilation tubes. Franche et al. (31) analyzed tympanometry results in 98 subjects (196 ears) who were subjected to myringotomy surgery and found types B and C tympanometry in 150 ears.
The pre-surgical audiometric evaluation findings in this study demonstrated alterations in all subjects, similar to the literature cited above (11,32,1), which showed that SOM causes significant auditory deprivation characterized by conductive hearing loss and changes based on tympanometry results.
In the analysis of the (C)AP tests, broken down by individual ears (Table 1), there was a significant difference between the RE and the LE. The RE performed better than the LE in DD and PPS across the three groups.
In the analysis of the (C)AP tests, significant results for the DD and GIN tests were found between groups based on the threshold of gap detection and percentage of correct answers. In other tests, PSI/SSI and PPS differences were not significant, but EGI performances were worse than CG and EGII in regard to the PPS test, while EGII showed worse PSI/SSI results compared with EGI and CG.
In a pairwise comparison of groups regarding the DD test, EGI and EGII had worse performances compared to CG, but EGI had changes in both ears, while EGII only had changes in the LE.
This difference between experimental groups can be explained by the fact that public schools in Brazil may be located in an environment that is susceptible to social violence and has few recreational areas, low social cultural education, a lack of books and little access to health resources; that is, this environment does not favor language development and adequate stimulation. However, the group of private school children who have a higher socioeconomic status and therefore more accessible language stimulation also showed alterations in DD test answers. These results are directly related to physiological changes caused by otitis media and not to socioeconomic factors.
Colella-Santos (33) studied the DD test responses of 140 right-handed subjects between the ages of 5 and 25 years during binaural integration and directed attention to the left and right. She concluded that children between 5 and 6 years had significantly better performance in the RE when compared with subjects aged 6 years, showing that test performance improves as children become older.
Better performance in the RE is explained by the structural Kimura theory because all the children in this study are right-handed (34). On the DD test, the better performance in the RE compared with the LE in EGI students is no longer expected because the asymmetry between the ears for this test occurs up to 6 years of age. However, in EGI, there were also lower average responses for the LE in the DD test based on CG values. Thus, these differences between the averages can be explained as a result of a maturational delay, which was most likely caused by stimulation inconsistency that aggravated the conductive hearing loss due to otitis media.
In this study, to evaluate temporal resolution, the GIN test was used. The EGI had a significant difference in relation to the gap detection threshold and percentage of correct answers when compared with the CG and EGII.
Several other studies have applied the GIN test in children and found values between 4.2 ms and 5 ms for the gap detection threshold and values between 73.6% and 78.27% for the percentage of correct answers (27,35,28). These results are similar to our results when the GIN was applied to the CG.
The low GIN scores in the group of children who underwent bilateral ventilation tube insertion suggests that episodes of SOM during the early years can preclude the proper input of auditory information responsible for temporal information sensory encoding. These factors are essential for enhancing temporal resolution because this skill develops at approximately 6 to 7 years and depends on the segregation of different auditory stimuli.
Among the auditory skills evaluated, temporal processing, which includes solving skills and temporal ordering, was the most changed in EGI (Table 4). Thus, EGI children have an 11.33 times higher likelihood of having impaired temporal resolution compared with CG subjects (Table 5).
Statistical analysis comparing student performance based on hearing skills.
| OR (CI 95%) | |||
|---|---|---|---|
| Hearing Skills | EGI x CG | EGII x CG | EGI x EGII |
| Figure-ground | ref 7.37 (2.39 to 22.76) | ref 7.00 (2.15 to 22.76) | ref 1.05 (0.41 to 2.73) |
| Temporal Ordering | ref 3.35 (1.32 to 8.50) | ref 1.78 (0.66 to 4.80) | ref 1.88 (0.72 to 4.93) |
| Temporal Resolution | ref 11.33 (3.80 to 33.83) | ref 2.83 (0.89 to 8.98) | ref 4.00 (1.46 to 10.98) |
| All normal | ref 0.1 (0.03 to 0.30) | ref 0.33 (0.12 to 0.90) | ref 0.29 (0.09 to 0.98) |
OR - Odds Ratio; CI - confidence interval; ref. – Reference.
The temporal resolution auditory ability is an important factor in speech perception because it contributes to the identification of small phonetic elements that are present in speech, and alterations in this ability suggest a lack of perception of normal speech and phoneme recognition.
In the figure-ground evaluation, EGI students had poorer hearing abilities; furthermore, children who underwent bilateral ventilation tube insertion had a 7.37-fold higher likelihood of presenting changes in this ability when compared with the CG.
To have good performance on the figure-ground test and a binaural integration task, the child needs to process different information that is simultaneously presented to both ears. Changes in this ability can be exposed by hearing difficulties in situations of background noise or in the presence of more than one person talking at the same time. These difficulties can compromise performance in school, where there are frequently situations that require the listener to ignore linguistic information from one source to concentrate on a main message.
These data suggest that EGI and EGII students were influenced by otitis media on the auditory skills that were evaluated; therefore, these children would have fewer chances (0.1) of having normal hearing abilities when compared with children without otitis media.
Studies that were conducted with children and adolescents suffering from SOM in their first 5 years of age and that considered (C)AP performance concluded that these subjects had greater difficulty in hearing auditory closure, figure-ground and binaural integration and had deficits in attention and learning difficulties in class (36–38).
The data in this study suggest the importance of early intervention in terms of minimizing the effects caused by otitis media in the development of auditory skills, especially considering the (C)AP evaluation in children who suffered from otitis media in early life to better understand the changes in auditory function development in this population and to develop appropriate therapies.
From the results, we conclude the following:
- Considering the (C)AP test, there were no significant differences between males and females.
- There are significant differences between the RE and the LE in regard to DD and PPS tests.
- Children who underwent surgery to insert ventilation tubes bilaterally in their first 5 years and attended public schools showed much worse performance when compared with children who had the same surgical procedure and attended private schools when considering the LE DD test and GIN.
- Temporal processing and figure-ground skills were the most altered.
AUTHOR CONTRIBUTIONSBorges LT and Colella-Santos MF participated in the planning, research and writing of the manuscript. Paschoal JR provided advice and participated in the planning of the manuscript.
This work was supported by the State of São Paulo Research Foundation (FAPESP).
No potential conflict of interest was reported.