To analyze the anatomical variations of sinuatrial nodal branch(es) of the coronary artery mainly regarding their number; a recent report from Japan claims the presence of 2 branches in up to 50% of cases, an occurrence that would permit adequate flow compensation in case of occlusion or section of 1 of these branches.
METHODS:The sinuatrial nodal branch(es) of 50 human hearts fixed in formol solution were dissected with the aid of a Normo Health 3.0 degree visor magnifying lens, measured, and classified as to the origin, route, and number of branches.
RESULTS:In 94% (n = 47) of cases, a single sinuatrial nodal branch was found. classified: (A) two right side types, R1 (in 46% of cases, n = 23), situated medial to the right auricle and R2 (in 4% of cases, n = 2), situated on the posterior surface of the right atrium; (B) three left side types, L1 (in 24% of cases, n = 12), situated medial to the left auricle, L2 (in 16% of cases, n = 8), situated posterior to the left auricle, and L3 (in 4% of cases, n = 2), situated on the posterior surface of the left atrium. Except for R2, each type was subdivided into ‘a‘ or ‘b‘ types, according to whether the sinuatrial nodal branch(es) occurred in a clockwise or counterclockwise orientation around the base of the superior cava vena. In 4% of cases (n = 2), 2 sinuatrial nodal branch(es) were observed with 1 branch originating from each of the coronary arteries. In 1 case (2%), 3 sinuatrial nodal branch(es) were found, 2 from the right coronary artery and the third probably from the bronchial branch of the thoracic aorta. In 30% of the cases, the sinuatrial nodal branch(es) formed a ring around the base of the superior cava vena. In all cases, the sinuatrial nodal branch(es) supplied collateral branches to the atrium and/or the auricle of the same side as its origin and/or to the opposite side.
CONCLUSION:The low frequency of 2 sinuatrial nodal branch(es) in Brazilian individuals, compared to the higher frequency found among the Japanese, is probably due to a variation associated with ethnic group origin.
Analisar as variações anatômicas do ramo do nó sinoatrial, principalmente quanto ao número, visto que a escola japonesa relatou a presença de dois ramos em até 50% dos casos, fato que permitiria a compensação, em caso de oclusão ou secção de um dos ramos.
MÉTODOS:O ramo do nó sinoatrial foi dissecado com o auxílio de lente de aumento com pala Normo Health, de 3,0 graus, em 50 corações fixados em solução de formol.
RESULTADOS:Em 94% dos casos, havia um ramo do nó sinoatrial, classificado em dois tipos do lado direito: D1 (46%) - ramo do nó sinoatrial situado medialmente à aurícula direita; D2 (4%) - ramo do nó sinoatrial na face posterior do átrio direito; e três tipos do lado esquerdo: E1 (24%) - ramo do nó sinoatrial medial à aurícula esquerda; E2 (16%) - posterior à aurícula esquerda; E3 (4%) - na face posterior do átrio esquerdo. Cada tipo, exceto D2, era subdividido em a ou b, conforme o sentido do RNSA fosse, respectivamente horário ou anti-horário ao redor da base da veia cava superior. Em 4% dos casos, havia dois ramos do nó sinoatrial, originados de ambas as artérias coronárias. Em 2% dos casos, havia três ramos do nó sinoatrial originados, dois da artéria coronária direita e o terceiro, provavelmente de artéria brônquica. Em 30% dos casos, o ramo do nó sinoatrial formava um anel ao redor da base da veia cava superior. Em todos os casos, o ramo do nó sinoatrial forneceu ramos colaterais para o átrio e/ou a aurícula do mesmo lado e/ou do lado oposto à sua origem.
CONCLUSÃO:A baixa freqüência de dois ramos do nó sinoatrial em indivíduos brasileiros, comparada à alta encontrada em japoneses, provavelmente seja variação associada com as diferentes origens étnicas.
Besides being an excellent guide to the location of the sinuatrial node, detailed anatomical knowledge of the blood supply to the sinuatrial node region, an investigated topic, demands further study due to its application in cardiac surgery and in cardiology, in order to more clearly understand disturbances in its function caused by coronary disease.1–7
In the last decade, with the advent of new surgical techniques used in the treatment of arrhythmias, more specifically of atrial fibrillation, knowledge of the characteristics and trajectory of the atrial branches, particularly the sinuatrial nodal branches of the coronary artery (SANB), have assumed great importance.8–11
With respect to the origin of arterial irrigation to the sinuatrial node, some authors have described it as a single branch, originating from the right coronary artery, from the circumflex branch of the left coronary artery and/or from the trunk of the left coronary artery,1,2,5,7,9,12–14 or even of the left bronchial artery.15 Other authors have reported the possible presence of 2 branches in up to 11% of cases.3,4,8,16–18 Recently, Futami et al10 and Kawashima and Sasaki11 found several branches at much higher frequencies—in up to 54% of cases among Japanese individuals.
Due to the variations found in the literature, we decided to investigate the anatomy of arterial irrigation to the sinuatrial node region regarding the origin, route, and number of branches, with the aim of contributing to the detailed knowledge applied to atrial arrhythmia diagnosis and atrial surgical intervention.
MATERIALS AND METHODSThe 50 human adult hearts studied in the present investigation, obtained from the Instituto de Medicina Legal de Campinas were fixed in 10% formol solution, preserved in 5% formol solution, and belong to the series used by Ortale19,20 in his description of the branches of the coronary arteries. The dissection was authorized by the Centro de Ciências da Vida, Pontifícia Universidade Católica de Campinas, as part of an approved project.
After removal of the epicardium, the surface branching of the left and right coronary arteries was dissected. To dissect the SANB, a Normo Health Care NH-01 3.0 dioptrics (degree) visor magnifying lens was used.
The length and diameter of each SANB was measured, together with its origin and in which sinuatrial node region it was positioned. Each SANB was classified as follows: left or right (L/R) types, according to its respective origin from the left/right coronary artery; subtypes L1/L2/L3, according to its respective route medial/posterior to the left auricle or on the posterior surface of the left atrium; and R1/R2, according to its respective route medial to the right auricle or on the posterior surface of the right atrium.5,9 The latter subtypes were classified into a or b type, according to its respective orientation, clockwise or counter-clockwise, and analyzed for the possibility of complete/incomplete ring formation around the base of the superior vena cava.2
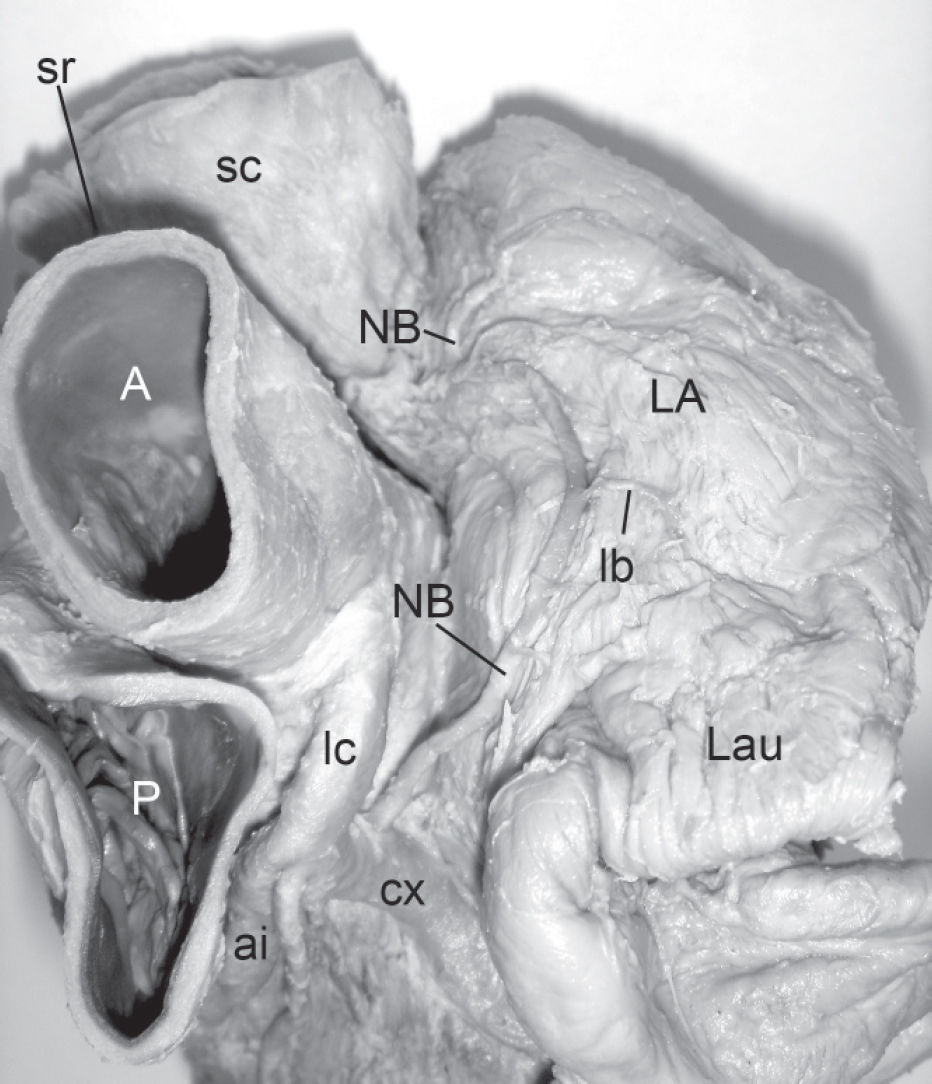
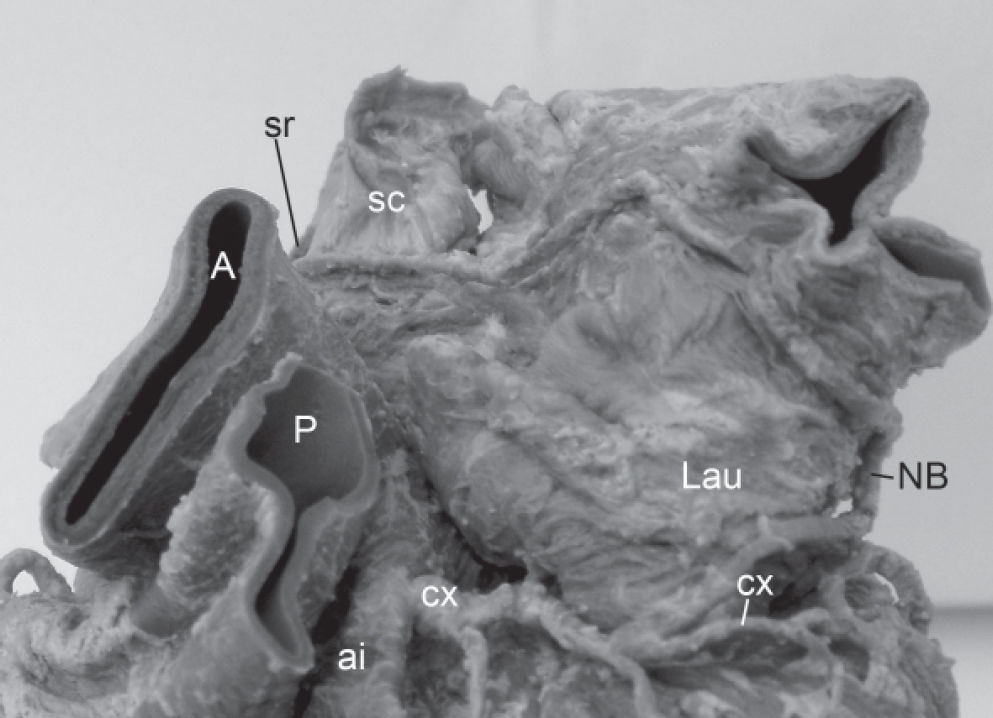
Accordingly, each SANB, except for the branch of probable bronchial artery origin, was classified into one of the following types (Figure 1):
R1 originating in the right coronary artery with a route medial to the right auricle, and subdivided into R1a (Figure 2) and R1b, according to its clockwise or counterclockwise route, respectively, in the sinuatrial node region at the base of the superior vena cava.
R2 originating in the right coronary artery with a route that traversed the posterior surface of the right atrium, crossing the sinuatrial node region to the right of the superior vena cava in a counterclockwise direction (type R2b).
L1 originating in the circumflex branch of the left coronary artery with a route medial to the right auricle and subdivided into L1a and L1b (Figure 3), according to its clockwise or counterclockwise route, respectively, at the base of the superior vena cava.
L2 originating in the circumflex branch of the left coronary artery with a route on the left pulmonary surface of the heart posterior to the left auricle and subdivided into L2a and L2b, according to its clockwise or counterclockwise route, respectively, at the base of the superior vena cava.
L3 originating in the circumflex branch of the left coronary artery with a route that traversed parallel to it, up to the posterior surface of the left atrium, where it described a convex curve to the right, passing inferiorly the left inferior pulmonary vein end and traversing the atrial ceiling to reach the sinuatrial region. This type assumed the form of an “S” in its route, from its origin to the sinuatrial region and could be subdivided into L3a (Figure 4) and L3b, according to its clockwise or counterclockwise route, respectively, at the base of the superior vena cava. For type R, the distance between the right aortic sinus and the origin of the SANB in the right coronary artery was measured. For type L, 2 distances were measured: left 1 (Dist L 1), between the left aortic sinus and the bifurcation of the left coronary artery and left 2 (Dist L 2), between this bifurcation and origin of the SANB in the circumflex branch of the left coronary artery.
Schematic representation of the route types of the sinuatrial node branch (NB) and its frequency. A. Types of the right side. B. Types of the left side. C, D. With 2 NB, 2 types, respectively: R1a, L1b and R1a, L2a. E. With 3 NB: 1 type R1a, other type R2 and the third branch probably originated from the bronchial branch of the thoracic aorta
A Mitutoyo digital pachymeter was used for the measurements in millimetric units with 1-decimal point approximations. The values were reported as minimum, maximum, and mean ± SD. A schematic representation of each heart was made, and some were photographed.
RESULTSTable 1 shows the frequency, number of branches, origin, diameter, length, distances from the origin to the aortic sinus, and the presence or absence of ring formation at the base of the superior vena cava.
Distribution of the frequency, number of branches, origin, diameter, length, distance from origin to aortic sinus, and ring formation at the base of the superior vena cava of the sinuatrial nodal artery branches (SANB)
| No.N° branches / origin origem | n | % | Do: | Dsr | Leng | Dist R | Dist L 1 | Dist L 2 | Complete Ring |
|---|---|---|---|---|---|---|---|---|---|
| 1 SANB | n | ||||||||
| 1 SNAB | |||||||||
| o: rc | 25 | 50 | 1.3-2.5 | 0.8-1.6 | 41.6-105.0 | 1.0-48.6 | - | - | 2 |
| 1.7± 0.3 | 1.2±0.2 | 71.4±14.3 | 17.9±13.6 | ||||||
| o: lc | 22 | 44 | 1.3-2.5 | 0.6-1.4 | 52.5-134.0 | 2.0-11.0 | 2.6-33.6 | 4 | |
| 1.8±0.3 | 1.1±0.2 | 95.2±28.1 | 7.2±2.6 | 13.3±10.8 | |||||
| 16 | |||||||||
| Total | 47 | 94 | 1.3-2.5 | 0.6-1.6 | 41.6-134.0 | 1.0-48.6 | 2.0-11.0 | 2.6-33.6 | 6 |
| 2 | 1.7±0.3 | 1.1±0.2 | 82.2±24.4 | 17.9±13.6 | 7.2±2.6 | 13.3±10.8 | |||
| SANBSNAB | |||||||||
| o: rc and lc | 2 | 4 | 1.4-2.0 | 0.6-1.3 | 40.1-98.5 | 19.6-21.2 | 6.0-7.2 | 7.6-12.3 | – |
| 3 | 1.9±0.3 | 1.0±0.3 | 64.7±29.0 | 20.4±1.1 | 6.6±0.8 | 10.0±3.3 | |||
| SANBSNAB | |||||||||
| o: rc and BB* | 1 | 2 | 1.2 | 85.,3 | 19.,9 | – | – | – | |
| Total | 50 | 100 | 1.1-2.5 | 0.6-1.6 | 40.1-134.0 | 1.0-48.6 | 2.0-11.0 | 2.6-33.6 | 6 |
| 1.7±0.3 | 1.1±0.28 | 1.3±24.8 | 20.3±14.7 | 7.1±2.5 | 13.0±10.4 |
SNAB = sinuatrial node branch; o: = origin; Do: = diameter at origin; Dsr = diameter in sinuatrial nodal region; Leng = length; Dist R = distance from ANBSNAB origin in right coronary artery to right aortic sinus; Dist L 1 = distance from bifurcation of the left coronary artery to the left aortic sinus; Dist L 2 = distance from SNAB origin in circumflex branch to the point of bifurcation of the left coronary artery. rc = right coronary artery; lc = left coronary artery; BB* = sinuatrial node branch, which was sectioned, probably originating from the bronchial branch of the thoracic aorta and measured only Dsr.
In 47/50 (94%) cases, a single SANB was found that originated from the right coronary artery in 25/47 of cases and was oriented as follows: 21/25 cases in the anterior segment and in 4/25 cases lateral to this artery. In 22/47 cases, a single SANB was found that originated from the circumflex branch of the left coronary artery, oriented as follows: 17/22 cases in the anterior segment and 5/22 cases in the lateral segment of this branch.
In 2/50 cases (4%), 2 branches were found originating from the anterior segment, one from the right coronary artery and the other from the circumflex branch of the left coronary artery. In 1/50 cases (2%), 3 branches were found; 1 branch originated in the anterior segment of the right coronary artery, 1 originated in the lateral segment of the right coronary artery, and 1 was sectioned during the heart removal procedure at the ceiling level of the left atrium and probably originated from the bronchial artery.
In 3/50 (6%) cases, all with a single SANB, with 2/3 cases being type L1b and 1/3 type L1a, the SANB presented a submerged segment in the interatrial septum along its route; after traversing the left atrial ceiling, it submerged in the septum, it became visible on the surface when reaching the sinuatrial node region.
A ring formation around the base of the superior vena cava was observed in 14/47 cases with 1 SANB, of which 8/14 cases were incomplete and 6/14 cases were complete, and in 1 case with several SANB (Table 1).
In 31/47 cases with a single SANB, the branch reached the node region to the right of the vena cava (type a, 21/31 and type b, 10/31), prior to descending (25/31) or not descending (6/31) on the terminal sulcus. In 16/47 type b cases, the SANB ascended along on the terminal sulcus to the node region. In 1/50 cases with 2 type a branches, both reached the node region to the right of the vena cava, where one branch descended along on the terminal sulcus and the other did not. In 1/50 cases with 2 branches, the type a branch did not descend along on the terminal sulcus and the type b branch ascended along on the terminal sulcus. In 1/50 cases with 3 branches, 2 originated in the right coronary artery ascending along on the terminal sulcus, while the third probably originated in the bronchial branch of the thoracic aorta, descending from the node to the terminal sulcus.
The SANB provided up to 10 collateral branches, where those originating from the right coronary artery emitted collateral vessels to the right atrium, right auricle, right ventricle aorta, left atrium, and/or superior vena cava, while the SANB originating from the left coronary artery emitted collateral vessels to the left atrium, left auricle, right atrium, and/or right auricle (Table 2). The mean ± SD of the diameters of the collateral branches were as follows: in hearts with 1 SANB, 0.9 ± 0.2 mm (range, 0.5-1.6 mm); with 2 SANB, 0.8 ± 0.10 (range, 0.5-1.0 mm); with 3 SANB, 0.6 ± 0.1 mm (range, 0.5-0.7 mm); and for the 50 hearts, 0.9 ± 0.2 mm (range, 0.5-1.6 mm).
Distribution of number, diameter, and territory of irrigation of the collateral branches of the sinuatrial nodal artery (SANB)
| 1 SANB (47 cases) | o: right coronary artery (25 cases) | o: left coronary artery (22 cases) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. bs | n | % | n | RA | Rau | LA | RV | A | SC | n | RA | Lau | LA | RAu |
| 1 | 7 | 14 | 5 | - | - | 5 | - | - | - | 2 | - | 1 | 1 | - |
| 2 | 7 | 14 | 3 | 3 | 1 | 2 | - | - | - | 4 | - | - | 8 | - |
| 3 | 7 | 14 | 2 | 4 | - | 2 | - | - | - | 5 | 2 | 1 | 12 | - |
| 4 | 11 | 22 | 6 | 10 | 6 | 7 | 1 | - | - | 5 | 3 | - | 17 | - |
| 5 | 4 | 8 | 2 | 6 | 1 | 2 | 1 | - | - | 2 | 3 | - | 7 | - |
| 6 | 2 | 4 | 1 | 5 | 1 | - | - | - | 1 | 3 | 1 | 2 | - | |
| 7 | 6 | 12 | 4 | 13 | 3 | 9 | 1 | 1 | 1 | 2 | 2 | - | 12 | - |
| 8 | 3 | 6 | 2 | 7 | 3 | 4 | - | - | 2 | 1 | 1 | - | 6 | 1 |
| 2 SANB (2 cases) | o: right coronary artery | o: left coronary artery | ||||||||||||
| No. bs | n | % | RA | Rau | LA | - | - | - | SC | - | Lau | LA | - | |
| 2 | 1 | 2 | - | - | - | - | - | - | 1 | - | 1 | - | - | |
| 10 | 1 | 2 | 1 | 2 | 1 | - | - | - | - | - | 1 | 5 | ||
| 3 SANB (1 case) | o: right coronary artery | |||||||||||||
| No. bs | n | % | - | Rau | LA | - | - | - | - | - | - | - | - | |
| 3 | 1 | 2 | - | 2 | 1 | - | - | - | - | - | ||||
No. bs = number of collateral branches of the SANB; o = origin; R+L = right and left side; RA = right atrium; Rau = right auricle; LA = left atrium; RV = right ventricle; A = aorta; SC = superior vena cava; Lau = left auricle.
The sinuatrial nodal branch of the coronary artery (SANB) corresponds to the eponym “branch of the Keith-Flack node,” attributed by Crainicianu.16 The SANB was the atrial branch with the largest diameter found in the study, except in 4% of the cases, in which the SANB was collateral to the intermediate atrial branch, which had a slightly larger diameter. The branches for the sinuatrial and atrioventricular nodes, together with the intermediate atrial branch, were the only atrial branches highlighted by the Federative Committee on Anatomical Terminology,21 probably due to their functional importance and constancy.
We agree with the authors referred to in Table 3, in that the SANB predominately originates from the right coronary artery, followed in frequency by the circumflex branch of the left coronary artery.
Comparison of frequencies of origin and branch numbers of sinuatrial nodal artery branches (SANB) reported by various authors
| Author(s) | 1 branch | 2 branches | 3 branches | |||||
|---|---|---|---|---|---|---|---|---|
| rc | cx / | lc | bb | rc + cx | cx/bb/rc | 2rc + | rc + | |
| (%) | (%) | 1 bb (%) | bb(%) | |||||
| Crainicianu (1922)10 | 68.0 | 25.0 | - | - | 7.0 | - | - | - |
| Géraudel (1925)15 | + | + | - | + | - | - | - | - |
| Campbell (1929)1 | 52.6 | 13.7 | 33.7 | - | - | - | - | - |
| James (1961)2 | 55.0 | 45.0 | - | - | - | - | - | - |
| Romhilt et al (1968)3 | 60.8 | 37.6 | - | - | 1.6 | - | - | - |
| Kennel and Titus (1972)12 | 65.0 | 35.0 | - | - | - | - | - | - |
| Hadziselimovic (1978)17 | 60.0 | 40.0 | - | - | - | 15/12/7* | - | - |
| Hutchinson (1978)13 | 65.0 | 35.0 | - | - | - | - | - | - |
| Nerantzis and Avgoustakis (1980)4 | 62.0 | 37.0 | - | - | 1.0 | - | - | - |
| Bokeriya et al (1984)5 | 61.4 | 28.6 | 10.0 | - | - | - | - | - |
| Busquet et al (1984)18 | 66.0 | 30.0 | - | - | 4.0 | - | - | - |
| Henriquez et al (1984)7 | 67.5 | 32.5 | - | - | - | - | - | - |
| Caetano et al (1995)14 | 58.0 | 30.0 | 12.0 | - | - | - | - | - |
| Sow et al (1996)8 | 64.5 | 24.4 | - | 11.1 | - | - | - | |
| Jatene et al (1999)9 | 63.3 | 36.7 | - | - | - | - | - | - |
| Futami et al (2003)10 | 73.4 | 3.3 | 23.3 | - | - | - | ||
| Kawashima and Sazaki (2003)11 | 32.0 | 14.2 | - | - | 50.0 | - | - | 3.8 |
| Present study (2006) | 50.0 | 44.0 | - | - | 4.0 | - | 2.0 | - |
rc = right coronary artery; lc = trunk of left coronary artery; cx, circumflex branch of left coronary artery; bb = bronchial branch of the thoracic aorta * The second branch originated from the circumflex branch of the left coronary artery, the bronchial artery, or the right coronary artery in 15%, 12%, and 7% of cases, respectively
In reference to the number of branches in the sinuatrial node, the results presented are intermediate to those obtained by several authors,3,4,8,16,18 who found 2 branches in percentages equal to or less than 11%, one originating from the right coronary artery and the other from the circumflex branch of the left coronary artery Table 3). In comparison with the present results, it is probable that the higher frequencies shown for the presence of 2 branches of the sinuatrial node reported by Futami et al10 (23%) and Kawashima and Sasaki11 (50%) are anatomical variations associated with a particular ethnic group—Brazilians, of European and African descendent, on the one hand and Japanese on the other. Regarding the frequency of 3 branches, our findings (2%) are similar to those of Kawashima and Sasaki11 (3.8%); these authors stated that the greater the number of branches and routes, the greater the possibility of collateral circulation in case of SANB section or obstruction. We agree with these authors11 that the sinuatrial branch is situated within the nodal mass. In one case in which 3 branches were found, 2 branches originated from the right coronary artery and the third probably originated from the bronchial artery. This latter branch, due to its extracardiac origin, had been sectioned in the heart removal procedure. This extracardiac origin was first described by Géraudel15 and was found as a second branch in 7% of cases by Hadziselimovic.17
With regard to the point of origin of the SANB, it was predominantly in the anterior segment and, in case percentages equal to or less than 10%, in the lateral segment, whether from the right coronary artery or circumflex branch of the left coronary artery; our results are in agreement with those of Romhilt and Hackel3 and Hutchinson.13 No branch origin was found in the posterior segment of the circumflex branch, as has been reported in 7.5% of cases,6 nor directly in the right aortic sinus, reported in 1.7% of cases.12 The mean diameter of the SANB, measured at the point of origin, was 1.7 mm, and measured within the node was 1.1 mm, both slightly larger than those reported by Kennel and Titus12 (1.1 mm and 0.7 mm). The branch length varied from 40.1 to 134 mm, values that were practically equal to those reported by Nerantzis and Avgoustakis (50-135 mm).4 The distance between the ostium of the right coronary sinus and the SANB origin was practically the same as that reported by Henríquez et al,7 while the distance between the origin of the circumflex branch and the SANB origin was slightly less than that described by those authors.7 Considering both sides, the degree of variation in the distance between the SANB origin and the ostia of the coronary sinus was greater than that reported by Nerantzis and Avgoustakis.4
In agreement with the results of several authors,3,6,9,13 the most frequently observed types on the right side were the medial route to the base of the right auricle, followed by the posterior route to the right atrium, the latter found in no more than 10% of cases.9 On the left side, in decreasing order, the routes were medial to the auricle, posterior to the base of the left auricle, and posterior to the left atrium. These last two were considered to be the same by Jatene et al.9
In 8% of cases, a percentage equal to or greater than that reported by a number of authors,4,12,22 we observed that the SANB formed an “S”, originating in the anterior or lateral segment and running parallel to the circumflex branch of the left coronary artery, describing a curve on the lateral surface (type E2) or on the posterior surface (type E3) of the left atrium, curving again under the left pulmonary vein to arrive at the atrial ceiling and the sinuatrial node.
In agreement with the results of Crainicianu,16 the SANB, whether originating in the right coronary artery or the circumflex branch of the left coronary artery, generally had a submerged route in the myocardium or sometimes in the interatrial septum. However, in some cases, the SANB was more than 2.0 mm in diameter, following a surface route to the node region, possibly presenting collateral branches.
Regarding the ring formation around the base of the superior vena cava by the SANB, several authors13,15,16 have reported that in a small number of cases, the SANB divides into branches that circle the base of the superior vena cava, thus forming a ring. This ring was complete, with the branch of greatest diameter following a counterclockwise route, in 12% of the cases observed in this study, a smaller percentage than the 16% reported by Anderson et al.22 The ring was incomplete in 18% of the cases observed in the current work, all with an counterclockwise route, except in 1 case, in agreement with Kennel and Titus.12 The ring was absent in 70% of the cases observed in this study, and the route traversed the node in a clockwise (44%) or counterclockwise (26%) direction. Thus, considering the total number of cases, the SANB showed a counterclockwise route in the majority of cases (54%), in agreement with Kennel and Titus12 and Anderson et al.22
In 6% of cases, a collateral branch of the SANB to the right ventricle was observed, such that in 1 of these cases, the branch provided was atrioventricular.23
The following conclusions were drawn: a) in 94% of cases only a single SANB was observed, originating from the right coronary artery (50%) and the left coronary artery (44%); in 4% of cases, 2 SANB were found, one on each side; in 2% of cases, 3 SANB were observed with 2 branches originating from the right coronary artery and a third probably from the bronchial artery. b) The length of the SANB originating from the left side was longer than that from the right. c) A predominance for the medial to auricle route occurred, whether the SANB originated from the left or right side. d) In 8% of cases, the SANB originating from the left presented the form of an “S”. e) At the base of the superior vena cava, the SANB presented a counterclockwise route in 54% of cases and a clockwise route in 46%, and in 30% of cases it formed a ring around the vein. f) In all cases, the SANB provided collateral branches to the atrium and/or the auricle of the same side as its origin and/or the opposite side. g) The frequency of the presence of 2 SANB was less in the Brazilians of European and African descent (4%) in this study than in those of Japanese decent (50%) reported in a previous study,11 which is probably an example of anatomical variations associated with ethnic origin.