Airway complications continue to be an important source of morbidity and mortality following lung transplantation, and bronchial stenosis is the most common manifestation. Such complications have been reported to occur in up to 27% of cases, and 13% of all transplanted patients may require interventional bronchoscopy for treatment.1 These complications have been attributed to an insufficient blood supply to the donor tracheobronchial tree, promoting ischemia and consequently leading to anastomotic dehiscence, malacia, or stenosis. Significant airway stenosis causes respiratory symptoms, decrease in lung function, and other complications, such as mucus retention and infection. Recently a novel thin-walled silicone self-expandable stent (Polyflex®) has been used to treat tracheal stenosis and tracheo-esophageal fistulas. We report a case of treating bronchial stenosis after single lung transplantation using the Polyflex® stent.
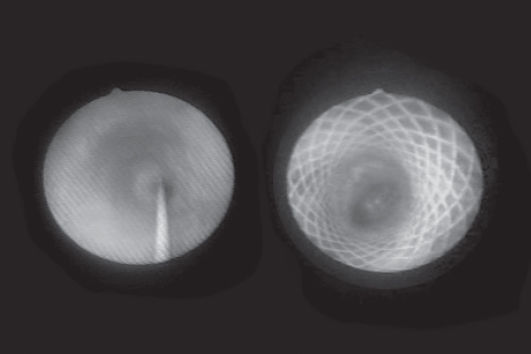
CASE DESCRIPTIONA 37-year-old woman was admitted with a diagnosis of lymphangioleiomyomatosis and underwent left lung transplantation. The bronchial anastomosis was made using polypropylene 4-0, running continuous suture in the posterior membranous wall, simple interrupted suture in the cartilaginous portion, and covered with a donor pericardial flap. The operation was uneventful, and the total ischemic time was 280 minutes. The postoperative period was without complications, and the patient was extubated after 4 hours and discharged from the hospital after 23 days. At this time, bronchoscopy was normal until the third month. Four months after the transplantation, she presented progressive dyspnea, cough, and rude stridor. Flexible bronchoscopy showed stenotic bronchial anastomosis, and the transbronchial biopsy revealed the presence of Cryptococcus neoformans. Computed tomography demonstrated a right loculated pneumothorax, which was treated with an anterior chest tube. Although treatment with amphotericin B oral was undertaken, there was no improvement of symptoms. She underwent balloon dilatation but developed acute respiratory failure a few hours after the procedure, as well as a new episode of right pneumothorax, requiring chest drainage. Under rigid bronchoscopy, we place a Polyflex® (Rüsch GMBH Inc., Kernen, Germany) self-expandable silicone stent 14 x 30 mm (Figure 1), and the patient was extubated few hours later. There was immediate clinical improvent. Three weeks afterwards, she had mucus plugging, and we observed a mild proximal dislodgement with exposition of the distal stenosis portion. Under rigid bronchocospy, we could easily remove the stent and exchange it for a Polyflex® 12 x 40 mm. Although the stenosis resolved, patient died due to sepsis a week later. There was no stent migration at autopsy.
DISCUSSIONSince the first lung transplant in humans performed by James Hardy in 1963, until the first successful lung transplantation by the Toronto Lung Transplant Group in 1983, about 40 transplants were performed around the world without success, most of them related to deficient healing of bronchial anastomosis. Although bronchial artery anastomosis has been supported by some authors, it is technically complicated and ineffective.2 Some other techniques, such as using a short donor bronchial stump, reinforcement of the anastomosis with an omental flap or intercostal muscle pedicle, and telescoping technique, have been shown to be more effective in the bronchial healing. Nowadays, airway complications still frequently occur, and the therapeutic options include balloon dilatation, laser photocoagulation, silicone or metallic stents, and reoperation.
Balloon dilatation has been considered a palliative treatment, with rapid improvement of symptoms but almost certain recurrence.3 Chhajed et al showed that 26% of their patients underwent dilatation alone for treatment of stenosis,4 considering it to be the first choice for treatment. Laser therapy may be used in thermoablation of granulation tissue around the stenosis, but it is ineffective in cases of bronchomalacia, and recurrence frequently occurs. Silicone stents, such as as Hood® and Dumon® stents, were used at first, but although they have great advantage being removable, they are also susceptible to dislodgement. Because of their thick walls and narrow lumens, mucus retention often occurs, and bronchoscopy is frequently necessary to clean up the prosthesis.5
Self-expandable metallic stents are less likely to dislodge, and their walls are thinner, enabling better secretion clearance. There are several reports comparing different types of stents. The Palmaz® stent, an expandable wire balloon stent, was used by Lonchyna and Burns, necessitating more interventions (5.22 vs 1.28) and with a higher complication rate (36.7% vs 10%) in comparison with the Wallstent® and Gianturco® stents. They have no elasticity, are difficult to remove, and fatal complications such as vascular perforation have occurred with this prosthesis. However, Herrera et al observed no complications with this stent and immediate mean improvement of FEV1 values of 87%.
Wallstent® and Ultraflex® are both made of metallic alloy (cobalt-based and nickel-titanium), have low resistance to clearance of secretions, but have adequate resistance to airway compression. They do not require hooks for fixation and conform to the tortuous airway, maintaining a radial force keeping them in position. Complications with these prosthesis are related to the difficult removal, granulation tissue formation, and mucus retention. Chhajed et al, in a comparative study with Gianturco®, Wallstent®, and Ultraflex® stents, obtained the best results with the Ultraflex® stent, such as lower rates of recurrence, mucus plugging, and migration.
The Polyflex® stent, a self-expandable stent, combines the advantages of the metallic ones (elasticity, good adaptation to the irregularities of tracheobronchial tree, and a thin wall allowing better secretion clearance) with those of the silicone stents, primarily the feature of being removable, and thus is the best conceived airway stent. This prosthesis, made of filaments of polyester covered with a silicone layer, is available in several lengths and diameters. Some experience has been achieved using this stent in the treatment of obstructions and tracheo-esophageal fistulas due to malignant disease. Bolliger et al used it in 26 patients, with low migration rate and few complications.6 Wasserman et al reported occasional infolding of the interior layer leading to obstruction.7 In our initial experience, migration was a common complication primarily related to mismatching the correct diameter of the stent. But with correct measuring, we now have patients with laryngotracheal stenosis treated for more than 1 year with Polyflex®.
Spontaneous pneumothorax in the native lung following transplantation and bronchostenosis has been reported before by Chhajed et al with resolution after insertion of a nitinol stent. The airway stenosis contributed to cause high resistance to air flow leading to preferential ventilation to the native lung, causing it to be more susceptible to pneumothorax.8 In our patient, pulmonary fungal infection may have contributed to causing stricture of the anastomosis and then native lung overinflation causing 2 episodes of pneumothorax. We were concern about using a metallic stent because we expected an improvement of stenosis after treatment of the fungal infection, and we decided to use a silicone stent. A removable self-expandable stent was a viable option due the possibility of removing it after treatment for fungal infection.
Although some authors have attempted take advantage of a metallic stent in the treatment of bronchial stenosis after lung transplantation, a removable self-expandable silicone stent seems to be an option in these cases. However, more experience must be achieved with the Polyflex® stent.