Population aging raises concerns regarding the increases in the rates of morbidity and mortality that result from influenza and its complications. Although vaccination is the most important tool for preventing influenza, vaccination program among high-risk groups has not reached its predetermined aims in several settings. This study aimed to evaluate the impacts of clinical and demographic factors on vaccine compliance among the elderly in a setting that includes a well-established annual national influenza vaccination campaign.
METHODS:This cross-sectional study included 134 elderly patients who were regularly followed in an academic medical institution and who were evaluated for their influenza vaccination uptake within the last five years; in addition, the demographic and clinical characteristics and the reasons for compliance or noncompliance with the vaccination program were investigated.
RESULTS:In total, 67.1% of the participants received the seasonal influenza vaccine in 2009. Within this vaccination-compliant group, the most common reason for vaccine uptake was the annual nationwide campaign (52.2%; 95% CI: 41.4–62.9%); compared to the noncompliant group, a higher percentage of compliant patients had been advised by their physician to take the vaccine (58.9% vs. 34.1%; p<0.01).
CONCLUSION:The education of patients and health care professionals along with the implementation of immunization campaigns should be evaluated and considered by health authorities as essential for increasing the success rate of influenza vaccination compliance among the elderly.
Population aging is a worldwide phenomenon, as the proportion of people who are age 60 years and older is increasing faster than any other age group, with an expected increase of 694 million (or 223%) from 1970 to 2025.1 Although the countries with the highest proportions of elderly people are in Europe, approximately 70% of the current global older population lives in developing countries; these countries must deal with the potential increases in economic, health and social demands that are related to aging.
In addition to neoplastic and degenerative diseases, some infectious complications, including those that are caused by influenza, occur more frequently among elderly individuals,2 who suffer the highest rates of serious illness and death that are associated with the disease.3,4,5
Therefore, influenza is a growing issue for public health and geriatric medicine concerns; consequently, seasonal vaccination is recommended for elderly individuals in several countries.6 Among the elderly, vaccination continues to be the most important tool for preventing influenza-related morbidity and mortality7,8 and is associated with reduced hospitalizations due to pneumonia or influenza and for any cause in community-dwelling older persons.3 In Brazil, a national influenza immunization campaign that targets individuals 60 years of age and older has been conducted since 1999;9 since its inception, reduced hospitalizations associated with respiratory diseases have been verified in this age group.10,11
Among high-risk groups, complying with this vaccination is essential to the success of preventive programs that target influenza; however, vaccination coverage among these groups has not reached the established aims in several developed or developing countries.12–16 The World Health Organization (WHO) has established goals for increasing the coverage of influenza vaccination among high-risk populations and has encouraged countries to implement initiatives to raise awareness of influenza and influenza vaccination among the public, although they have not indicated which initiatives should be adopted.17
Several studies that were conducted in Europe and North America identified risk factors for noncompliance with influenza vaccination among the elderly, including low income,18,19 African-American ethnicity,12,20 a good self-perception of health,21,22 younger age,12,14,19,21 cognitive impairments,19 living alone,19 and fear of adverse events following vaccination.18,22 In Brazil, two recent population-based surveys reported that age, smoking, and a lack of an appointment with a physician in the previous year were all independently associated with vaccination noncompliance. In addition, other reasons that were reported were a fear of adverse events following vaccination and a lack of concern regarding the influenza disease itself. The most widely cited source of information regarding the vaccine was the television (66.4%), and the second most frequent source was friends (25.3%), whereas nurses and doctors were cited by only 10.4% and 5.3% of the interviewees, respectively. It was more alarming that in one of the studies, only 10% of the participants mentioned a recommendation by a physician as their motivation for vaccine compliance.23,24
The influence of counseling by physicians and other health care professionals regarding influenza vaccination compliance requires further investigation. It is also conceivable that health care professionals who are involved with primary health care or with the treatment of respiratory diseases, including family physicians, gerontologists, and pulmonologists, might be more prone to recommend the influenza vaccination to their patients, which is a hypothesis that needs to be explored further.
This study was designed to evaluate the impacts of clinical and demographic factors on vaccine compliance among the elderly in a setting that includes a well-established annual national influenza vaccination campaign.
METHODSThis was a cross-sectional study that was conducted in the city of São Paulo, Brazil, between two and five months after the close of the 2009 influenza seasonal vaccination national campaign. The study included patients who were 60 years of age or older and were followed regularly in four different outpatient services (i.e., the Geriatrics, Urology, Pulmonology, and Rheumatology clinics) in a tertiary academic medical institution. The study was approved by the Ethics Committee of the University of São Paulo Medical School. Patients who attended any of the four aforementioned clinics were invited to participate in the study and were interviewed at the hospital after providing informed consent. The interviews were conducted twice weekly on various weekdays during the study period, and all patients who were attending the clinics for their medical appointments were invited to participate. Information was obtained regarding the influenza vaccination status for the previous five years, the demographic and clinical characteristics, and the reasons for compliance or noncompliance with the vaccination program. The reasons for vaccination compliance or noncompliance were obtained via an open question.
The demographic and clinical characteristics of the two groups of patients (i.e., those who had been compliant and those who had been noncompliant with the seasonal influenza vaccination in 2009) were compared using the Pearson's Chi-square test or the two-sided Fisher's exact test for analyzing the categorical variables or using the two-sample Student's t-test, assuming equal variances for analyzing the continuous variables.
The 95% confidence intervals for the percentages of the reasons for vaccination compliance or noncompliance were calculated using the exact binomial method.
The percentages of physicians who had recommended the seasonal influenza vaccination in each clinic were compared using the two-sided Fisher's exact test, and clinics were compared individually using the Pearson's Chi-square test when the clinics were pooled. The following comparisons were performed when the clinics were pooled: the Geriatric clinic versus the other clinics, the Pulmonology clinic versus the other clinics, and the Geriatric and Pulmonology clinics versus the Urology and Rheumatology clinics. The Bonferroni correction was used to adjust for multiple comparisons.
Logistic regression was performed to identify the variables that were associated with compliance with the seasonal influenza vaccination. The following variables were included in the initial model: age, ethnicity, years of education, income, hospital admissions during the previous year, whether they lived alone and/or attended the clinic alone, whether they had a caregiver, if they provided a good self-evaluation of health, the presence of any chronic health condition, the use of medication for a chronic health condition, memory loss, and the recommendation for vaccination by the physician. The backward stepwise regression procedure, with a p-value of 0.05 for backward selection, was used to obtain the final model for the logistic regression analysis.
Each statistical test used a significance level of 0.05 and was performed using STATA version 10.1 software (StataCorp, College Station, TX, USA).
RESULTSA total of 134 patients accepted to participate in the study. These patients had a mean age of 76.2 years (SD ± 8.1) and were primarily included in the Geriatrics clinic (65.7%), followed by the Pulmonology (14.2%), Rheumatology (12%), and Urology (8.1%) clinics. Overall, 67.1% (95% CI: 58.5–75%) of the participants had taken the seasonal influenza vaccine in 2009. The characteristics of the patients were stratified by compliance or noncompliance with their seasonal influenza vaccine in 2009. The data are presented in Table 1.
Characteristics of the interviewed patients according to their seasonal influenza vaccine uptake in 2009.
| Vaccine Uptake | |||
|---|---|---|---|
| Yes (n = 90) | No (n = 44) | ||
| n (%) | p-value∗ | ||
| Age (mean) | 76.3 | 75.9 | 0.8† |
| Male | 25 (27.8) | 16 (36.4) | 0.31 |
| Ethnicity | 0.22 | ||
| Caucasian | 67 (74.4) | 29 (65.9) | |
| Black | 9 (10) | 4 (9.1) | |
| Mulatto | 9 (10) | 10 (22.7) | |
| Asian | 5 (5.6) | 1 (2.3) | |
| Years of education | 0.16 | ||
| <4 | 27 (30) | 14 (31.8) | |
| 4 to 8 | 48 (53.3) | 17 (38.6) | |
| >8 | 13 (29.5) | 15 (16.7) | |
| Income‡ | 0.15 | ||
| <2X minimum wage | 31 (34.4) | 21 (47.7) | |
| 2 to 4X minimum wage | 47 (52.2) | 20 (45.5) | |
| >4X minimum wage | 12 (13.3) | 2 (4.6) | |
| Had a housemate | 67 (74.4) | 38 (86.4) | 0.12 |
| Attended health services alone | 40 (44.4) | 22 (50) | 0.54 |
| Had a caregiver | 22 (24.4) | 12 (27.2) | 0.72 |
| Had regular medical follow-up | 89 (98.9) | 44 (100) | 1∗∗ |
| Personal physician recommended the vaccine | 53 (58.9) | 15 (34.1) | 0.007 |
| Had any chronic disease | 88 (97.7) | 43 (97.7) | 1∗∗ |
| Long-term use of medication | 89 (98.9) | 40 (90.9) | 0.04∗∗ |
| Referred memory loss | 53 (58.9) | 20 (45.5) | 0.14 |
| Good self-evaluation of health status | 52 (57.8) | 25 (56.8) | 0.91 |
| Hospital admission during the previous year | 22 (24.4) | 6 (13.6) | 0.15 |
| Took the seasonal influenza vaccine in 2008 | 84 (93.3) | 8 (18.2) | <0.001 |
| Took the seasonal influenza vaccine at least once in the previous 4 years | 79 (95.2) | 11 (26.8) | <0.001 |
Within the vaccination-compliant group, a higher percentage of patients were receiving medication for a chronic condition than in the noncompliant group (98.9% vs. 90.9%, respectively; p<0.05), and a higher percentage had taken their influenza vaccine in 2008 (93.3% vs. 18.2%, respectively; p<0.05) or at least once in the previous four years (95.2% vs. 26.8%, respectively; p<0.05). In the compliant group, the most frequently cited motivation to take the vaccine was the annual nationwide campaign that was held by the Brazilian Ministry of Health (52.2%; 95% CI: 41.4–62.9%), which was followed by a belief in the protective effect of the vaccine (37.7%; 95% CI: 27.8–48.6%) and recommendation by a physician (35.5%; 95% CI: 25.7–46.3%). Other less frequently mentioned reasons included the lack of side effects, the prevention of pneumonia, vaccination as part of their routine medical care, and frequent episodes of influenza disease (Table 2). A higher percentage of patients in the vaccination-compliant group had been advised by their personal physician to take the vaccine (58.9% vs. 34.1%; p<0.05).
Referenced reasons for influenza vaccination compliance or noncompliance in 2009.
| For compliance | % (95% CI) |
|---|---|
| National influenza vaccination campaign | 52.2 (41.4–62.9) |
| Believed the influenza vaccine is protective | 37.7 (27.8–48.6) |
| Physician recommended it | 35.5 (25.7–46.3) |
| Another health care professional recommended it | 1.1 (0–6) |
| For noncompliance | % (95% CI) |
|---|---|
| Believed the influenza vaccine causes influenza disease | 36.4 (22.4–52.2) |
| Fear of adverse events | 15.9 (6.6–30) |
| Believed they would never contract influenza | 15.9 (6.6–30) |
| Lack of transportation | 9 (0–17.9) |
| Pain | 4.6 (0–15.8) |
Within the vaccination-noncompliant group, the reason that was most frequently cited as their reason to not take the vaccine was the belief that it could induce influenza (36.4%; 95% CI: 22.4–52.2%), which was followed by the belief that the vaccine causes other side effects (16%; 95% CI: 6.6–30%) and the idea that they rarely contracted influenza (16%; 95% CI: 6.6–30%). Other less frequently mentioned reasons included pain due to the vaccine administration and transportation difficulties. Previous vaccine side effects were not reported as reasons to avoid taking the vaccine (Table 2).
The medical recommendation for the influenza vaccine was not statistically different among the four outpatient clinics when evaluated separately (p = 0.25) or when analyzed in the following combinations: Geriatrics versus the other clinics (p = 0.6), Pulmonology versus other clinics (p = 1.0), and Geriatrics and Pulmonology versus the Rheumatology and Urology clinics (p = 0.13).
The logistic regression model revealed that a recommendation from a physician to take the vaccine was the only variable that was significantly associated with vaccine compliance. Patients in the vaccination-compliant group had a likelihood of receiving a recommendation that was 2.7-fold higher than the vaccination-noncompliant group (OR = 2.7; 95% CI = 1.29–5.6; p<0.05).
DISCUSSIONWe believe that preventing influenza among the elderly through vaccination is certainly one of the primary public health goals that governments worldwide should pursue to promote their health and disease prevention policies and achieve an improved quality of life in old age, according to the “active aging” framework established by the WHO.
A prerequisite for the widespread vaccination of high-risk groups is more equitable access to the vaccine, and this has been partially addressed by the Global Action Plan (GAP), outlined by the WHO, in which they projected a sharp increase for 2010 in the annual production capacity of trivalent seasonal influenza vaccine to more than 800 million doses and noted that production capacity is currently available, or is being established, in 25 countries, including developing countries.25 Once the influenza vaccine is available in sufficient quantities, governments then face the challenge of achieving high coverage among high-risk groups.
This study gathered additional evidence to facilitate the planning and improvement of strategies and initiatives that seek to increase the uptake of influenza vaccinations among the elderly. This population is not homogeneous, and this is reflected by the various risk factors that were identified for poor vaccination uptake; the initiatives should reflect this heterogeneity. In this regard, this study provides valuable information regarding a specific subset of older individuals who are followed regularly in a tertiary teaching hospital and who likely have a number of comorbidities.
A recommendation by a physician was found to be a key factor for compliance; this is consistent with other studies. However, doctors are also not a homogeneous population, even in an academic medical institution, and a high proportion of doctors did not advise their patients regarding the influenza vaccination. The association of counseling that is performed by physicians and other health care professionals with influenza vaccination should be explored further in future studies and should be considered in initiatives that seek to improve vaccination uptake, including vaccination campaigns.
Another aspect that should be considered an essential element of any influenza vaccination program is the implementation of campaigns to instruct the population regarding the risks and benefits of the vaccine. The various reasons for vaccine uptake included the belief in vaccine efficacy, whereas the reasons for a lack of compliance included misinformation regarding influenza and the influenza vaccine.
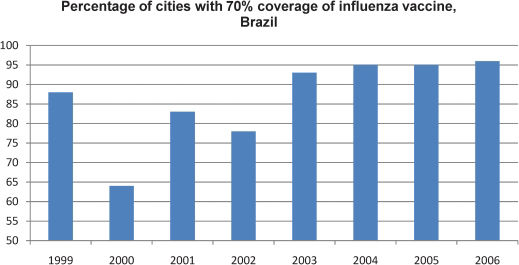
Finally, the most frequent reason that was cited by the patients as their motivation to take the vaccine was the annual nationwide influenza vaccination campaign. National influenza immunization campaigns that target older persons have been conducted in Brazil since 1999, which was considered The International Year of Older Persons. Several strategies have been used by the Brazilian government to promote and maintain influenza vaccine coverage among older persons (Figure 1) including the participation of medical societies, social organizations, radio and TV stations, and the presence of additional health care professionals, thereby minimizing long waiting lines and system malfunctions.9 In the initial years of campaigning, population compliance with the vaccine was moderate; it was generally believed that vaccines should only be administered to children, and the benefits of influenza vaccination in the elderly were not yet fully understood. In addition, myths, such as the occurrence of flu-like symptoms following vaccination, helped propagate distrust towards the vaccine. However, the annual campaigns were continued, and after 2003, more than 90% of Brazilian cities reached the 70% vaccine coverage goal (Figure 2).9 In addition to this experience in Brazil, other authors have analyzed similar strategies for mass influenza vaccination in various settings26,27 and found that these strategies can be cost-effective.
Strategies that were adopted by the Brazilian government to promote and maintain influenza vaccine coverage among older persons. Adapted from the National Influenza Immunization Campaign Targeting Older Persons Technical Report, Brazil, Ministry of Health, 2007.9
Percentage of Brazilian cities with at least 70% influenza vaccine coverage from 1999 through 2006. Adapted from the National Influenza Immunization Campaign Targeting Older Persons Technical Report, Brazil, Ministry of Health, 2007.9
The primary limitations of this study are the sample size and source population, which came from a tertiary academic medical institution. Our sample included a large proportion of patients with more severe and complex diseases, and most of the patients were receiving medication for chronic conditions. For this particular population, the reasons for vaccination compliance may not reflect those of the elderly in the general; therefore, our findings cannot be generalized, and any inferences from our results should be carefully considered.
The success of influenza vaccination program among the elderly will likely depend on multiple demographic and clinical factors that can vary from region to region and should be evaluated by local health authorities, along with actions, such as vaccination campaigns and educating both the target population and health care professionals.
The authors are grateful to the graduate students Maira Leite and Ricardo Costa, who contributed to the acquisition of data.
No potential conflict of interest was reported.
Avelino-Silva VI participated in the design and coordination of the study, acquisition of the data and manuscript writing. Avelino-Silva TJ participated in the design of the study, acquisition of the data and manuscript writing. Miraglia JL participated in the statistical analysis and manuscript writing. Miyaji KT participated in the design of the study and acquisition of the data. Jacob-Filho W participated in the design of the study and manuscript writing. Lopes MH participated in the design of the study and manuscript writing.