To compare the measurements of spirometric peak expiratory flow (PEF) from five different PEF meters and to determine if their values are in agreement. Inaccurate equipment may result in incorrect diagnoses of asthma and inappropriate treatments.
METHODSSixty-eight healthy, sedentary and insufficiently active subjects, aged from 19 to 40 years, performed PEF measurements using Air Zone®, Assess®, Galemed®, Personal Best® and Vitalograph® peak flow meters. The highest value recorded for each subject for each device was compared to the corresponding spirometric values using Friedman’s test with Dunn’s post-hoc (p<0.05), Spearman’s correlation test and Bland-Altman’s agreement test.
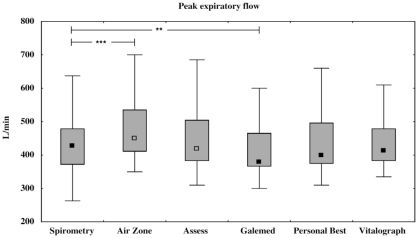
RESULTSThe median and interquartile ranges for the spirometric values and the Air Zone®, Assess®, Galemed®, Personal Best® and Vitalograph® meters were 428 (263–688 L/min), 450 (350–800 L/min), 420 (310–720 L/min), 380 (300–735 L/min), 400 (310–685 L/min) and 415 (335–610 L/min), respectively. Significant differences were found when the spirometric values were compared to those recorded by the Air Zone® (p<0.001) and Galemed ® (p<0.01) meters. There was no agreement between the spirometric values and the five PEF meters.
CONCLUSIONSThe results suggest that the values recorded from Galemed® meters may underestimate the actual value, which could lead to unnecessary interventions, and that Air Zone® meters overestimate spirometric values, which could obfuscate the need for intervention. These findings must be taken into account when interpreting both devices’ results in younger people. These differences should also be considered when directly comparing values from different types of PEF meters.
“Peak flow meters” are portable pieces of equipment that measure the peak expiratory flow (PEF) and are a common, low-cost and simple method that provides consistent readings.1–3 The severity of a patients’ asthma can be inferred from daily variations in PEF values. This parameter is commonly used for monitoring, diagnosing and observing the evolution of asthma.4–6 Several studies have emphasized the importance of PEF measurements in hospital, outpatient and domiciliary care environments.7–9
It is absolutely necessary that PEF meters provide a linear response10 and that they also provide precise and reliable measurements because discordant values from the different types of meters commonly found in outpatient clinics may result in inappropriate asthma monitoring and treatment.2
Many different studies have focused on testing the accuracy of these meters by comparing devices from different manufacturers and equipments from the same brand; these studies have revealed significant inter- and intra-meter variations.1,5,7,8,11–14 In these studies different methods were used to evaluate the accuracy of the peak flow meters, such as a flow generator acknowledged and recommended by the American Thoracic Society (ATS), the collaboration of individuals generating flow in a spirometer connected in series to the meters, or to separate the performance of spirometry measurements with several peak flow meters, with subsequent comparison of the results. It is generally believed that there is a difference in the observed accuracy of the measurements depending on whether the flow is generated by human subjects or by flow generator equipment. It has been suggested by Pretto et al. and cited by Koyama et al. that values obtained using human subjects are more clinically relevant.8 As a result, some studies have assessed peak flow meter accuracy by taking the spirometric PEF as representative of the true value.15 However, no studies comparing Air Zone®, Assess®, Galemed®, Personal Best® and Vitalograph® meters using PEF values obtained during the spirometric forced vital capacity (FVC) maneuver could be found in the literature.
Therefore, the present study aimed to determine whether there are differences among the obtained readings of these five different meters by comparing them with the best FVC maneuver test PEF values performed during the spirometry, considering these latter as true and standard representatives values, verifying if, for each one of the devices, there is an accordance with the spirometric values.
MATERIALS AND METHODSPEF measurements were obtained from sixty-eight healthy, sedentary and insufficiently active volunteers. The volunteer group comprised 50 women and 18 men, all aged between 19 and 40 years, and all residents of the city of São Carlos (SP) or its surrounding area. Smokers, former smokers, individuals presenting respiratory, neurological, temporomandibular or cognitive problems were excluded. Individuals on medication that could influence respiratory performance were also excluded. Fifteen potential subjects were excluded, which represents an 18.1% loss of the sample, considering the total number of volunteers (83 subjects) that participated in the research.
The present study was approved by the institution’s Ethics Committee (nº 058/2007). All subjects were informed regarding the research procedures, and they also freely signed an informed consent statement that granted the researchers the right to record data for research purposes in accordance with Brazilian National Health Council Resolution 196/96. Subsequently, the subjects were submitted to evaluation and measurements.
The evaluation consisted of an anamnesis and a physical exam in which personal data were collected, i.e., name, date of birth, sex, weight, height, smoking habit, presence of previous diseases and pharaceitical drug use. Subjects were also subjected to an interview about physical activity that utilized the short version of the International Physical Activity Questionnaire (IPAQ) to quantify the volunteers’ physical activity level.16
PEF values were measured using five different types of meters, each of which was new and duly calibrated by the manufacturer. The meters used included the Peak Flow Meter Air Zone® (Clement Clarke Inc, Ohio, USA), the Peak Flow Meter Assess® (Health Scan, New Jersey, USA), the Peak Flow Meter Galemed® (Galemed Corporation, Taipei Hsien, Taiwan), the Peak Flow Meter Personal Best® (Health Scan, New Jersey, USA) and the Peak Flow Meter Vitalograph® (Buckingham, UK). The order in which the measurements were taken was determined by a random drawing. The same copy of each device was used for all measurements.
The PEF measurements were obtained in an air-conditioned room where the volunteers remained in an orthostatic position and used a nasal clip to prevent leakage of air through the nose. Volunteers were requested to take a maximum inspiration and thereafter to provide a maximum fast and intense expiratory effort. Volunteers were informed not to bend their neck during the procedure and not to obstruct the mouthpiece with their tongue or spit during the forced expiration to prevent the measurement of higher values that are considered as false.17
During the maneuver the subjects received standardized verbal encouragement and repeated the maneuver three times for each of the five PEF meters. In cases where a difference of more than 40 L/min was observed among the three attempts, more attempts were made until the difference among the values was less than 40 L/min.17
After the measurements with each meter, a 30-second pause was taken to prevent respiratory muscle fatigue.
On non-coincident days, the subjects also performed three other spirometric maneuvers, i.e., slow vital capacity (SVC), forced vital capacity (FVC) and maximal voluntary ventilation (MVV), to demonstrate that they had normal pulmonary function using a portable EasyOne® brand spirometer, which had been duly calibrated. Each maneuver was repeated three times with the subjects seated, using a nasal clip and following the American Thoracic Society/European Respiratory Society (ATS/ERS) recommendations.18 The best value was selected by the instrument, which possesses an internal quality control device. The same examiner performed all of the measurements, and each subject was given standardized instructions and verbal commands. The reference values employed were those proposed by Knudson et al. 19
The highest PEF value obtained from the valid maneuvers performed with each meter was selected and compared to the best PEF value for each subject in the FVC test.
Graph Pad InStat® software, version 3.05 (Graph Pad Software, Inc.) was used to analyze the results of the study. The Kolmogorov-Smirnov test was used to evaluate the normality of the data; the data did not identify a normal distribution. A nonparametric method of analysis was therefore used for the analysis. The highest PEF values from the 68 subjects for each meter were compared with the spirometric PEF values using Friedman’s test with Dunn’s post-hoc test. To assess the relationship between the spirometry value and the value recorded from each meter, Spearman’s non-parametric correlation was calculated because only two of the six analyzed variables were considered as normal using the normality test.
The Bland-Altman plot20 was used to determine the agreement between the five different PEF meters and the PEF spirometric values. MedCalc software, version 9.4.1.0 (MedCAlc, Mariakerke, Belgium) was used for this analysis. Significance was accepted at p<0.05.
RESULTSThe means and standard deviations (SD) of the studied population, with regard to age, height, weight, body mass index (BMI), FEV1/FVC ratio, FVC and FEV1, are presented in Table 1, in addition to the median values and interquartile ranges for the spirometric values and PEF values obtained with Air Zone®, Assess®, Galemed®, Personal Best® and Vitalograph® meters. In Figure 1, a significant increase between PEF spirometric values and those obtained with Air Zone® is observed (p<0.001), and significant decrease when these are compared to Galemed® meter (p<0.01). The percent error for the spirometric values for each meter was 5.1% for Air Zone®, 1.9% for Assess®, 11.2% for Galemed®, 6.5% for Personal Best® and 3.0% for Vitalograph®.
Mean and SD of the subjects’ age, height, weight, BMI, FEV1/FVC ratio, FVC and FEV1, as well as the spirometric and the five meters PEF medians and interquartile ranges values.
| Mean ± SD | |
|---|---|
| Age (years) | 22 ± 3.4 |
| Height (cm) | 166.1 ± 9 |
| Weight (kg) | 64.2 ± 14.9 |
| BMI (kg/m2) | 23 ± 4 |
| FEV1/FVC (%) | 88 ± 6.2 |
| FVC (% predicted) | 91.6 ± 9.3 |
| FEV1 (% predicted) | 92.6 ± 10.1 |
| Spirometry (L/min) | 428 (263–688) |
| Air Zone® (L/min) | 450 (350–800) |
| Assess® (L/min) | 420 (310–720) |
| Galemed® (L/min) | 380 (300–735) |
| Personal Best® (L/min) | 400 (310–685) |
| Vitalograph® (L/min) | 415 (335–610) |
Table 2 shows the results of Spearman’s non-parametric correlation. Highly positive and statistically significant correlations (p<0.0001) were found between the spirometric values and those obtained from the five different PEF meters, indicating that each meter provides similarly valid readings when PEF spirometric values are considered as representative of the true value.
A Bland-Altman20 plot was used to provide a graphical analysis of the agreement between the spirometric values and the values obtained from the five different PEF meters (Figure 2).
Agreement rate between PEF spirometric values and those of the Air Zone® meter (A); the Assess® meter (B); the Galemed® meter (C); the Personal Best® meter (D); and the Vitalograph® meter (E) according to a Bland-Altman analysis. PEF = peak expiratory flow; Bias = mean of the differences among the averages; SD = standard deviation; n = number of subjects; ±1.96SD= 95% of confidence interval (CI). Orange line = regression line of differences versus averages; blue line= 95% CI of limits of agreement; brown dashed line= 95% CI mean of differences.
As shown in Figure 2, it was not possible to identify any agreement between the spirometric PEF values and those recorded by the five different meters, considering that the mean of difference between the means±1,96 standard deviation (95% of confidence interval) of the PEF spirometric values versus those obtained by Air Zone® meter (figure 2A), Assess® meter (figure 2B), Galemed® meter (figure 2C), Personal Best® (figure 2D) and Vitalograph® (figure 2E) were, respectively, −46.5±47.3 (−139.2 to 46.2L/min), −19.2±45.3 (−108.0 to 69.6L/min), 16.8±46.9 (−75.1 to 108.7L/min), 5.9±48.9 (−90.0 to 101.7L/min) and 1.1±45.1 (−87.3 to 89.5L/min). A great variation in the limits of agreement was observed, i.e., around 185.4 L/min for Air Zone®, 177.6 L/min for Assess®, 183.8 L/min for Galemed®, 191.7 L/min for Personal Best® and 176.8 L/min for Vitalograph®.
DISCUSSIONThe results of the present study show that the Air Zone® and Galemed® meters provide significantly different results compared to the spirometric values and suggest that these two meters are less accurate if spirometric values are taken to be representative of the true value. However, such findings are not indicative of an unusually poor performance by these meters. In fact, Spearman’s non-parametric correlation demonstrated that all of the meters have equivalent correlation coefficients. Thus, the individual performance of each meter is adequate; comparisons of daily PEF values will be reliable and will have equivalent validity. The Air Zone® meter had PEF values that were significantly higher than the spirometric values, tending to overestimate them while the Galemed® meter tended to underestimate the spirometric values by presenting values significantly inferior.
It was not possible to find agreement between the spirometric values and any of the values obtained with the five meters, which demonstrates that it is not possible to estimate PEF spirometric readings from the values obtained with the above-mentioned meters. The lack of agreement can be explained by the fact that the means of difference between the averages had been high and therefore distant from the agreement point, due to the great interindividual variation and to the great variation of limits of agreement. Thus, it was not possible to conclude that the spirometric values agreed with those obtained from the five meters because the agreement level was not acceptable for clinical purposes.
There are other studies that partially corroborate these findings. Imbruce21 tested ten adult meters from the MiniWright®, Assess®, Vitalograph® and Ferraris® brands and concluded that the Assess® meter was the only one that fulfilled the National Heart, Lung and Blood Institute (NHLBI) criteria. Eichenhorn et al.12 observed that the Assess® meter is more accurate than the MiniWright® meter and the Vitalograph Pulmonary Monitor® when tested in a series with a pneumotachograph.
A study by Folgering et al.,22 which aimed to compare PEF values recorded with MiniWright®, Personal Best®, Wright Pocket fdE®, Vitalograph®, Assess®, Pocket Peak flow meter® and Truzone® meters to those recorded on a duly calibrated pneumotachograph for 50 subjects, found that the Personal Best® meter provided the best agreement with the pneumotachograph readings.
In contrast, there is some evidence in opposition to the results of this study. When comparing Assess®, MiniWright®, Ferraris® and Astech® meters using a computerized flow generator designed to produce ATS standardized flows, Jackson23 observed that the Astech® brand presented the best performance in terms of accuracy, variability and reproducibility considering the National Asthma Education Program (NAEP) recommendations. Another study that compared MiniWright®, Assess®, Pulmo-graph® and Wright Pocket® meters with PEF values recorded during the forced vital capacity maneuver of patients with asthma, chronic obstructive pulmonary disease (COPD) and bronchiolitis, as well as healthy subjects, also found that the Assess® meter provided a highly significant difference.8
These studies observed results that are equivalent in some aspects to those of the present study. The differences in results may be due to differences in the methodologies applied, or they may be due to the present study’s use of a population that is significantly younger than those assessed in the other mentioned studies.
In the study by Jackson,23 a computerized flow generator designed to produce ATS standardized flows was used to compare several PEF meters. Differences observed relative to this study can be explained by the fact that experiments using human subjects to verify the meters’ accuracy are limited by the lack of an absolute flow pattern.13 Whereas this study did utilize human subjects, the use of a qualified examiner and of standard verbal commands assured that the effort demanded during the PEF measurement was the subject’s maximum and was similar for all of the meters. According to Nazir et al.14 and Pretto et al. (and cited by Koyama et al.8), despite the fact that measurements obtained with human subjects may be less accurate than those made with flow generating equipment, it has been suggested that the measurements obtained with human subjects are more clinically significant.
The Assess®, Personal Best® and Vitalograph® meters did not show significant differences from the spirometric values, but they did not show agreement, suggesting that their readings are clinically valid but are not able to estimate or replace the spirometric PEF.
There are only a few studies in the literature that assess the accuracy of the meters used in the present study. Studies evaluating Air Zone® and Galemed® meters were not found, which suggests that more research is needed to support this study’s conclusions regarding the meter models available on the market.
The results of the present study suggest that the Galemed® and Air Zone® meters provide significantly different values when compared to spirometric values, have great variation in their agreement limits, and may underestimate the measurement and cause an unnecessary intervention (Galemed®), or they may overestimate the value and obfuscate the need for an intervention (Air Zone®). This must be taken into account when interpreting the readings from both meters in younger adults, as well as when making direct comparisons with PEF readings from different meters. Attention should be given to the direct comparison between the different PEF meters reading because the random use of different meters for sale in the national market may produce results that put at risk the monitoring and evaluation of patients with obstructive respiratory problems.
The lack of agreement between the spirometric values and the values obtained from the five meters tested does not indicate that these meters lack validity or perform poorly; it only indicates that the meters cannot replace the PEF spirometric measurements. While spirometry provides measurements of variability, reversibility and airflow limitation severity, and also confirms the diagnosis of asthma, its cost is higher and its availability is lower in both the public and private healthcare systems compared to peak flow meters. Peak flow meters are low-cost, simple methods that provide consistent readings and, therefore, are recommended for clinical and functional control of asthma symptoms, as well as for the patient’s daily monitoring of the symptoms. These attributes make measurements by peak flow meters viable in routine clinical practice.
Conflict of Interest Statement
The authors declare that they participated in designing the study and in the analyses of the results, thereby making effective contributions to the manuscript. We declare that we are responsible for the content of this manuscript and that no link or funding agreement between the authors and any companies that might have an interest in the publication of this article has been omitted. We affirm that we do not have any conflicts of interest regarding either the topic covered by the article or the products cited.
We declare that the article above is an original work and that no other work with substantially similar content has been sent to any other scientific periodical in printed or electronic form.