To study the imaging exams more commonly used for abdominal aortic aneurysms evaluation – ultrasonography, conventional computerized tomography, helical computerized tomography and nuclear magnetic angioresonance – comparing the preoperative measurements reached by those radiological methods with the measurements made during the surgical procedures.
METHODSPatients who had indication of elective transperitoneal surgical treatment for their abdominal aortic aneurysms were included in the study. The initial diagnosis of the aortic dilatation was made by ultrasonography and, after the surgical treatment was indicated, the patient was submitted to another imaging method.
Sixty patients were divided into 3 groups according to the complementary imaging method (conventional computerised tomography, helical computerized tomography, nuclear magnetic angioresonance). The ultrasonography of the first 20 patients were joined in a fourth group. There were considered in the study the measurements of the transversal diameter of the proximal neck, maximum transversal diameter of the aneurysm, straight-line length and transversal diameter of the common iliac arteries given by the imaging methods. The same measurements were made by using a caliper during the surgical procedure, and then compared to the values obtained from the radiological exams.
RESULTSThe maximum transverse diameter had a range measurement variation of 4.5 to 13.6 cm in the intraoperative, with no statistically significant differences when compared with all the imaging tests. The ultrasonography, however, overestimated the measurements of the proximal neck and the common iliac arteries, in comparison with intraoperative measures. The length of the aorta aneurysm obtained by the conventional computerized tomography was significantly lower if compared to the measures done with the calliper during the operation. The helical computerized tomography and the nuclear magnetic angioresonance provided measurements with no significant differences in the statistic view when compared to the intraoperative measures.
CONCLUSIONSUltrasonography is a reliable method for the diagnosis and follow-up of the aorta abdominal aneurysms, but insufficient for endovascular surgery planning. The conventional computed tomography can provoke distortion in the length measurements of the aorta dilatation. Helical computed tomography and nuclear magnetic angioresonance provided precise measurements of all the studied parameters, being of great utility for surgical planning.
Estudar os métodos mais freqüentemente empregados na avaliação dos aneurismas de aorta abdominal – ultrassonografia, tomografia computadorizada convencional, tomografia computadorizada helicoidal e angio-ressonância nuclear magnética – comparando as medidas fornecidas por estes exames radiológicos no pré-operatório com medidas realizadas durante a operação.
MÉTODOForam incluídos no estudo pacientes portadores de aneurisma da aorta abdominal com indicação de tratamento cirúrgico eletivo por via transperitoneal. O diagnóstico inicial da dilatação aórtica foi feito com ultra-sonografia e, uma vez indicado o tratamento cirúrgico, era então solicitado um outro exame radiológico complementar, já que não é nossa rotina operar esses pacientes com base apenas na ultra-sonografia. Sessenta pacientes foram divididos em 3 grupos de acordo com o exame complementar realizado (tomografia computadorizada convencional, tomografia computadorizada helicoidal ou angio-ressonância nuclear magnética). As ultra-sonografias dos 20 primeiros pacientes foram incluídas em um 4° grupo.
Analisamos neste estudo as medidas do colo proximal da aorta, o diâmetro transverso máximo e o comprimento do aneurisma, além do diâmetro transverso das artérias ilíacas comuns conseguidos a partir dos exames radiológicos. As mesmas medidas eram realizadas por ocasião da operação com o auxílio de um paquímetro e, então, comparadas aos valores indicados pelos exames de imagem.
RESULTADOSAs medidas do diâmetro transverso máximo do aneurisma variaram de 4.5 a 13.6 cm no intra-operatório, não apresentando diferença estatisticamente significativa em relação a nenhum dos exames radiológicos estudados. A ultra-sonografia, entretanto, superestimou as medidas do colo proximal da aorta e dos diâmetros transversos das artérias ilíacas, em comparação com os valores auferidos durante o tratamento cirúrgico. O comprimento dos aneurismas medidos pela tomografia computadorizada convencional era menor em relação às medições feitas com o paquímetro de maneira estatisticamente significativa. Tanto a tomografia computadorizada helicoidal quanto a angio-ressonância nuclear magnética proporcionaram medidas sem diferença significante do ponto de vista estatístico para todos os parâmetros estudados, quando confrontados com os valores obtidos no intra-operatório.
CONCLUSÕESA ultra-sonografia consiste em método valioso para o diagnóstico e seguimento clínico de pacientes com aneurisma de aorta abdominal, sendo, porém, insuficiente para o planejamento de tratamento por técnica endovascular. A tomografia computadorizada convencional pode induzir a erro na estimativa da extensão crânio-caudal do aneurisma. A tomografia computadorizada helicoidal e a angio-ressonância nuclear magnética geraram medidas precisas de todos os parâmetros estudados, sendo ambos de grande importância para a programação operatória.
The endovascular treatment of aortic aneurysms, requires the determination of the exact dimensions of the affected artery for the correct selection of the prosthesis as well as to ensure the success of the procedure.
The most used imaging methods in the diagnosis and follow-up of patients with abdominal aortic aneurisms are ultrasonography (USG), conventional computerized tomography (CCT), helical computerized tomography (HCT), and nuclear magnetic angioresonance (NMR).
In the literature there are reports comparing these methods regarding patients with abdominal aortic aneurisms;1,2,3 however, few of them are prospective, include a large sample population, or make comparisons with surgical findings, which are certainly the most reliable test of measurement efficacy for these different methods.
The objective of this study was to compare the preoperative measurements of aortic aneurysms revealed by USG, CCT, HCT, and NMR with actual measurements made during the surgical procedure, thus to evaluate the accuracy of the imaging methods.
PATIENTS AND METHODSBetween June 1998 and December 2001, after approval by the Ethical Committee of the São Paulo University Medical School, 60 consecutive patients with infrarenal abdominal aortic aneurysms, with or without compromised iliac arteries, were analyzed.
Only patients who had an indication for surgical treatment by transperitoneal access were included.
The initial diagnosis of abdominal aortic aneurysm was made by USG, and the maximum transverse diameter was measured by this method. If surgical treatment was indicated, the patient underwent one other imaging method.
Because an aortic aneurysm is a life-threatening condition that requires prompt treatment, it would not have been ethical to submit each patient to all the other 3 methods, due to the delay in surgical treatment. Consequently, patients were divided into groups according to the complementary imaging method performed after the USG (CCT, HCT, or NMR). The first 20 patients, irrespective of the complementary imaging method performed, composed the group in which USG results were used in the comparison (Group 1). For the 40 subsequent patients the complementary imaging method, rather that the USG results were considered in the study. Thus, the patient groups were as follows: Group 1, USG; Group 2, CCT; Group 3, HCT; and Group 4, NMR.
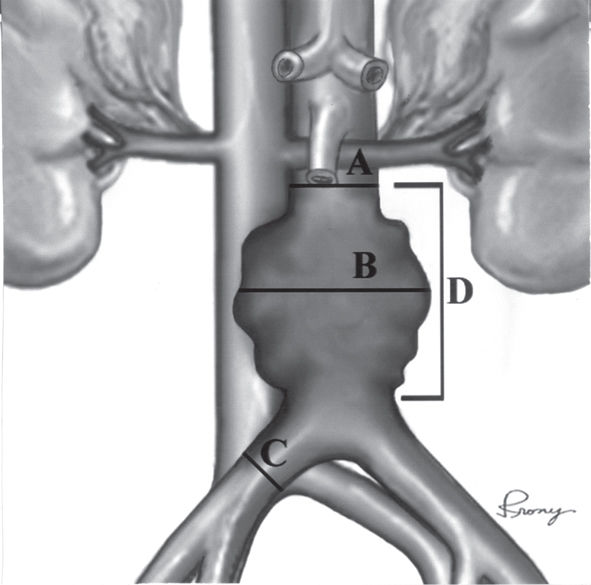
All measurements during the preoperative period were made from images by the same radiologist, as follows (Figure 1):
- •
Transverse diameter of the proximal neck of the aorta (A).
- •
Maximum transverse aortic diameter (B).
- •
Straight-line length of the aneurysm (D).
- •
Transverse diameter of the iliac arteries at their greatest diameter when an iliac aneurysm was present, or the diameter measured approximately 2 cm above the bifurcation when they exhibited a normal caliber (C).
An investigator blinded to the preoperative measurements made the intraoperative measurements in all groups. These measurements were performed using a caliper after full dissection of the aneurysm and before aortic clamping (Figure 2). A slightly modified caliper with elongated blades to facilitate the surgical measurements was utilized.
In this study, the surgical measurement was considered the gold standard to which all the imaging methods measurements were compared.
Of the 60 patients, 48 (80%) were male and 12 (20%) female; their ages ranged from 53 to 81, with a mean age of 67.3 years.
An exclusion criterion for Group 4 was the presence of a pacemaker or any metallic material that prohibited the nuclear magnetic resonance procedure.
A GE 500 instrument with a 3.5 MHz convex transducer was utilized in the USG imaging, and transversal and longitudinal scans were made.
For the NMR images, we used a GE Signa 1.5 Tesla instrument. The 3D reconstruction was performed using the Advantage Workstation for Windows, version 4.0. Patient preparation required a 4-hour fast and an intravenous injection (30-mL) of gadolinium-DTPA medium (0.2 mmol/kg).
The HCT images were made by a GE Hi-Speed instrument, with 5 to 10 mm scans before and after contrast injection (2 mL/kg).
Statistical AnalysisThe Wilcoxon nonparametric test was used for the analysis of results, with a significance level of α = 0.05
RESULTSNeither complications nor intercurrent events occurred during the imaging procedures or due to the intraoperative caliper measurements, which were concluded in a 2- to 4-minute interval. All the imaging methods employed in this study confirmed the clinical diagnosis of the aneurysm.
The maximum intraoperative transverse diameter of the aorta ranged from 4.5 to 13.6 cm, which was not significantly different from any of the preoperative imaging results.
Table 1 compares USG measurements with the respective intraoperative aneurysm findings.
Comparison between ultrasonography measurements (USG) and surgical observation (SO) (n = 20).
| Region | USG Average ± SDMedian | SO Average ± SDMedian | Statistical comparison |
|---|---|---|---|
| PN | 2.8 ± 0.5 | 2.5 ± 0.4 | P = 0.008* |
| 2.8 | 2.6 | ||
| MDA | 6.5 ± 1.3 | 6.3 ± 1.2 | P = 0.344 |
| 6.3 | 6.2 | ||
| LA | 10.5 ± 3.2 | 10.5 ± 2.5 | P = 0.979 |
| 10.5 | 10.2 | ||
| DRI | 2.4 ± 1.0 | 2.1 ± 0.8 | P = 0.005* |
| 2.0 | 2.0 | ||
| DLI | 2.2 ± 0.8 | 2.0 ± 0.8 | P = 0.016* |
| 2.1 | 1.7 |
PN = proximal neck; MDA = maximum transverse diameter of the aorta; LA = straight-line length of the aneurysm; DRI = diameter of the right common iliac artery; DLI = diameter of the left common iliac artery
There were statistically significant differences for the measurements of the proximal neck and of the common iliac arteries. Ultrasonography overestimated those found during the surgery at the same sites.
Table 2 compares CCT measurements with the respective intraoperative surgical observations.
Comparison between conventional computerized tomography (CCT) measurements and surgical observation (SO) (n = 20).
| Region | CCT Average ± SDMedian | SO Average ± SDMedian | Statistical comparison |
|---|---|---|---|
| PN | 2.4 ± 0.4 | 2.3 ± 0.4 | P = 0.092 |
| 2.4 | 2.3 | ||
| MDA | 5.3 ± 1.0 | 5.3 ± 1.0 | P = 0.693 |
| 5.5 | 5.2 | ||
| LA | 8.6 ± 2.8 | 9.6 ± 2.7 | P <0.001* |
| 8.0 | 9.3 | ||
| DRI | 2.0 ± 0.9 | 1.9 ± 0.9 | P = 0.244 |
| 1.9 | 2.0 | ||
| DLI | 1.7 ± 0.7 | 1.7 ± 0.7 | P = 0.336 |
| 1.5 | 1.5 |
PN = proximal neck; MDA = maximum transverse diameter of the aorta; LA = straight-line length of the aneurysm; DRI = diameter of the right common iliac artery; DLI = diameter of the left common iliac artery
The length of the aortic aneurysm obtained by CCT was significantly less compared with the intraoperative measurements.
Table 3 compares HCT measurements with the respective intraoperative surgical observations.
Comparison between helical computerized tomography (HCT) measurements and surgical observation (SO) (n = 20).
| Region | HCT Average ± SDMedian | SO Average ± SDMedian | Statistical comparison |
|---|---|---|---|
| PN | 2.6 ± 0.5 | 2.6 ± 0.6 | P = 0.772 |
| 2.6 | 2.6 | ||
| MDA | 6.1 ± 1.0 | 6.2 ± 1.0 | P = 0.275 |
| 6.0 | 6.0 | ||
| LA | 10.3 ± 2.7 | 10.4 ± 2.7 | P = 0.818 |
| 9.6 | 9.8 | ||
| DRI | 1.6 ± 0.5 | 1.6 ± 0.5 | P = 0.385 |
| 1.8 | 1.8 | ||
| DLI | 1.5 ± 0.5 | 1.5 ± 0.5 | P = 0.425 |
| 1.4 | 1.3 |
PN = proximal neck; MDA = maximum transverse diameter of the aorta; LA = straight-line length of the aneurysm; DRI = diameter of the right common iliac artery; DLI = diameter of the left common iliac artery; * = statistically significant; SD = standard deviation.
None of the HCT results were significantly different from the intraoperative results.
Table 4 compares NMR measurements with the respective intraoperative surgical observations.
Comparison between nuclear magnetic resonance (NMR) measurements and surgical observation (SO) (n = 20).
| Region | NMR Average ± SDMedian | SO Average ± SDMedian | Statistical comparison |
|---|---|---|---|
| PN | 2.6 ± 0.5 | 2.5 ± 0.5 | P = 0.209 |
| 2.6 | 2.6 | ||
| MDA | 5.9 ± 1.0 | 5.9 ± 1.0 | P = 0.502 |
| 5.8 | 5.8 | ||
| LA | 9.6 ± 2.6 | 10.0 ± 2.6 | P = 0.165 |
| 9.5 | 9.4 | ||
| DRI | 1.9 ± 0.7 | 1.8 ± 0.7 | P = 0.624 |
| 1.8 | 1.8 | ||
| DLI | 1.6 ± 0.5 | 1.5 ± 0.5 | P = 0.131 |
| 1.5 | 1.3 |
PN = proximal neck; MDA = maximum transverse diameter of the aorta; LA = straight-line length of the aneurysm; DRI = diameter of the right common iliac artery; DLI = diameter of the left common iliac artery; * = statistically significant; SD = standard deviation.
None of the NMR measurements were significantly different from the surgical observations.
DISCUSSIONAortic abdominal aneurysms are usually initially suspected during a physical examination by means of the careful palpation of the abdomen.4 Such suspicion can be confirmed by imaging methodology. The USG is the most utilized imaging method for this purpose since it is noninvasive, practical, and specific.5 However, from the moment a surgical treatment is considered, information regarding other parameters beyond the maximum transverse diameter of the aneurysm is required for planning the surgical operation. Precise information regarding the proximal and distal extent of the aortic dilatation and the possible compromising of the visceral arteries is vitally important for procedural success when endovascular treatment is the chosen option.6,7
Imprecise measurements can introduce a risk of not totally excluding the aneurysm (thereby allowing leakage) and even some visceral branch occlusion, especially of the renal artery. Anatomic variations and concomitant abdominal diseases can also affect the decisions regarding the most appropriate techniques and operative tactics. For these reasons, accurate imaging technologies are necessary.
Comparisons between the diagnostic accuracy of different radiological methods for measuring aneurysms have been made in several studies, with very controversial results.8,9,10 Few authors have compared imaging methods (USG, CCT, HCT, and NMR) with the surgical findings, which is the most reliable standard for such comparative studies.
Fox et al.11 compared surgical measurements with those obtained by USG and NMR in 13 patients. They found similarity in the proximal neck measurements by both methods; on the other hand, NMR better assessed the length and diameter of the iliac arteries.
Baud et al.12 observed that the USG underestimated the anterior-posterior aortic diameter and the proximal neck when compared with CT results. When they compared these imaging results to the surgical findings, they found that the anterior-posterior and transverse diameters were similar, whereas USG and CT had a sensitivity of 75% and 50%, respectively, regarding the extent of the aneurysms when the lower limit was above the bifurcation of the aorta.
Castrucci et al.13 evaluated the performance of NMR imaging in 80 patients and found high sensitivity compared with the surgical findings; the same pattern was found by Ecklund et al. regarding USG and CT in 40 patients.
Prior to our study, no specific, prospective study had been designed to compare the surgical findings with all radiological measurement methods (USG, CCT, HCT, and NMR).
Our data analysis showed that USG (Figure 3) had good precision both for the evaluation of the aneurysm length (longitudinal extent) and for the transverse diameter of the aorta (the main risk factor for rupture), demonstrating that USG is an important tool for surgical planning. However, the measurements of the proximal neck and iliac arterial diameters from USG images were significantly smaller than the corresponding intraoperative measurements. Consequently, we conclude that USG may be considered a valuable imaging method for the diagnosis and follow-up of clinically treated patients with abdominal aortic aneurysms, but that it is insufficient for suitable surgical planning, especially in cases requiring endoluminal corrections.
Conventional CT (Figure 4) was first used in 1980 in the diagnosis and preoperative and postoperative evaluations of abdominal aortic aneurysms.14,15 It provided clear images with information regarding the size and extent of the aneurysm, presence of intraluminal thrombi, calcifications and anatomic anomalies, ruptures, as well as the presence of an inflammatory component. Conventional CT has the advantage over the angiography of revealing not only the vessel lumen but also the walls and adjacent structures. The CCT exam takes only a few minutes, and intravenous iodide contrast medium injections can be used but may cause problems with nephrotoxicity and eventual allergic complications. In our study, we did not have complications resulting from the use of iodide contrasts.
Our data analysis revealed that, on one hand, CCT has good accuracy regarding the proximal neck, transverse diameter of the aorta, and common iliac artery measurements, which did not differ statistically from those achieved in the intraoperative setting. On the other hand, this method showed some inconsistency with intraoperative measurements in the evaluation of the aneurysm length, probably due to artefacts caused by breathing movements. Thus, CCT can be considered a valuable method not only for diagnosis but also for conventional surgery planning. At present, with the improvement of endoluminal correction techniques for aortic aneurysms, CCT has become the most utilized method in a number of medical centers. However, errors in the length measurements of the aneurysms may compromise the success of the procedure.
Other advantages of CCT compared with USG are the good visualization of the suprarenal aorta, iliac arteries, and thoracoabdominal transition, as well as the fact that image interpretation does not depend on the examiner. Available in most hospitals, CCT is a rapid and convenient method for the patient since only a peripheral venous puncture is necessary. However, CCT is more expensive than the USG and may be subject to interference from breathing movements.
Helical computerized tomography (Figure 5) is an evolution of CCT. The images are constructed faster and require lower radiation exposures and volume of contrast for the patient. In addition, HCT allows 3D reconstruction and eliminates interference from breathing movements, which is a frequent cause of distortions in other imaging technologies.16,17
In our study population, we did not observe any difference between measurements from HCT images and the intraoperative measurements of the proximal neck of the aorta, the transverse diameter of the aorta and iliac arteries, and the longitudinal extent of the aneurysms. Consequently, with exact measurements of the arteries, we were able to plan for any type of abdominal aortic aneurysm treatment (conventional or endovascular).
Nuclear magnetic angioresonance (NMR) (Figure 6) is a recently developed technique that utilizes a powerful magnetic field and the different tissue characteristics to generate images in multiple planes.3,18,19 Developed at the end of the 1980s, it is relatively noninvasive and provides information about the arterial wall morphology, the adjacent structures, and the physiology of arterial flow. It does not result in adverse effects from radiation, radio-opaque contrasts, or arterial catheterization punctures that can be caused by other imaging techniques. It reveals the vessel structures, with not only the aneurysm lumen but also the walls and perivascular structures being well delineated. Patients with pacemakers or metallic devices cannot be submitted to NMR because the magnetic field may be harmful in such conditions.
Like the HCT technique, the NMR technique used in this study allowed precise measurements to be made that did not differ significantly from the measurements made during surgery
CONCLUSIONS- 1.
USG is a reliable technology for the diagnosis and follow-up of abdominal aortic aneurysm patients; however, it insufficient for endovascular surgery planning.
- 2.
CCT is potentially faulty in measuring the length (extent) of the aortic dilatation and is therefore not suitable for the endovascular surgery planning.
- 3.
HCT and NMR are precise methods for evaluating all the studied parameters, including the proximal neck of the aorta and the maximum transverse diameters of the aorta and iliac arteries. Therefore, they are technologies of fundamental value, and either of these methods can be used by themselves for endovascular surgery planning.