Nasal continuous positive airway pressure is used as a standard of care after extubation in very-low-birth-weight infants. A pressure of 5 cmH2O is usually applied regardless of individual differences in lung compliance. Current methods for evaluation of lung compliance and air distribution in the lungs are thus imprecise for preterm infants. This study used electrical impedance tomography to determine the feasibility of evaluating the positive end-expiratory pressure level associated with a more homogeneous air distribution within the lungs before extubation.
METHODSVentilation homogeneity was defined by electrical impedance tomography as the ratio of ventilation between dependent and non-dependent lung areas. The best ventilation homogeneity was achieved when this ratio was equal to 1. Just before extubation, decremental expiratory pressure levels were applied (8, 7, 6 and 5 cmH20; 3 minutes each step), and the pressure that determined the best ventilation homogeneity was defined as the best positive end-expiratory pressure.
RESULTSThe best positive end-expiratory pressure value was 6.3±1.1 cmH20, and the mean continuous positive airway pressure applied after extubation was 5.2±0.4 cmH20 (p = 0.002). The extubation failure rate was 21.4%. X-Ray and blood gases after extubation were also checked.
CONCLUSIONThis study demonstrates that electrical impedance tomography can be safely and successfully used in patients ready for extubation to suggest the best ventilation homogeneity, which is influenced by the level of expiratory pressure applied. In this feasibility study, the best lung compliance was found with pressure levels higher than the continuous positive airway pressure levels that are usually applied for routine extubation.
Mechanical ventilation is crucial for the stabilization and care of extreme preterm infants. It can be applied invasively, through an endotracheal tube, or non invasive ventilation (NIV), with the use of non-invasive interfaces, which is associated with a lower morbidity rate in preterm infants (1,2). Nasal continuous positive airway pressure (CPAP) applied using nasal prongs is the most common type of NIV performed on extreme preterm infants (3-5).
For very-low-birth-weight (VLBW) infants who undergo invasive ventilation, extubation failure is unpredictable and occurs in approximately 20 to 30% of patients (6). The use of CPAP in these patients is the standard of practice that aims to reduce this complication, but different approaches and interfaces are used among hospitals (7-10).
Electrical impedance tomography (EIT) provides real-time bedside information that can be used to estimate regional lung ventilation (11-14). This technique has been used to study ventilation patterns in adults and neonates, but it has not yet been used to evaluate preterm infants before extubation (15-20). Recently, differences in tidal ventilation were assessed for volume-targeted ventilation in preterm infants (14). Variations in positive end-expiratory pressure (PEEP) levels and the resulting effect on air distribution in preterm infants during spontaneous assisted conventional ventilation were not previously studied.
In this study, we used EIT in VLBW during assisted mechanical ventilation immediately before extubation. This study was designed to determine the feasibility of evaluating the PEEP level associated with a more homogeneous air distribution within the lungs before extubation by using electrical impedance tomography. We used EIT to determine the PEEP level associated with the best air distribution in the lungs of these patients, which corresponds to the best ventilation homogeneity (VH) and follows the global inhomogeneity index concept previously described by Zhao et al., i.e., a ratio of 1 ventilation between the dependent and non-dependent lung (21,22).
MATERIAL AND METHODSStudy populationThis study was performed in the Hospital Israelita Albert Einstein NICU in São Paulo after approval by the institutional review board and the institution's ethics committee. Every VLBW infant (birth weight <1,500 g), regardless of the prior respiratory disease that determined invasive ventilation, was submitted to the following ventilatory parameters before extubation: synchronous intermittent mandatory ventilation plus a pressure support mode (SIMV+PS; Servo-i - Maquet Getinge Group, Sweden), FiO2≤0.35, PEEP≤6 cmH20, and respiratory rate ≤15 breaths/min. Exclusion criteria included congenital malformations, intracranial hemorrhage of grades III and IV (23) and previous pneumothorax.
The patients were assigned to the routine CPAP of 5 to 6 cmH20 applied after tube removal at the discretion of the attending staff, as is the routine procedure at our institution. As this was a feasibility study, a convenience sample of fourteen patients was chosen.
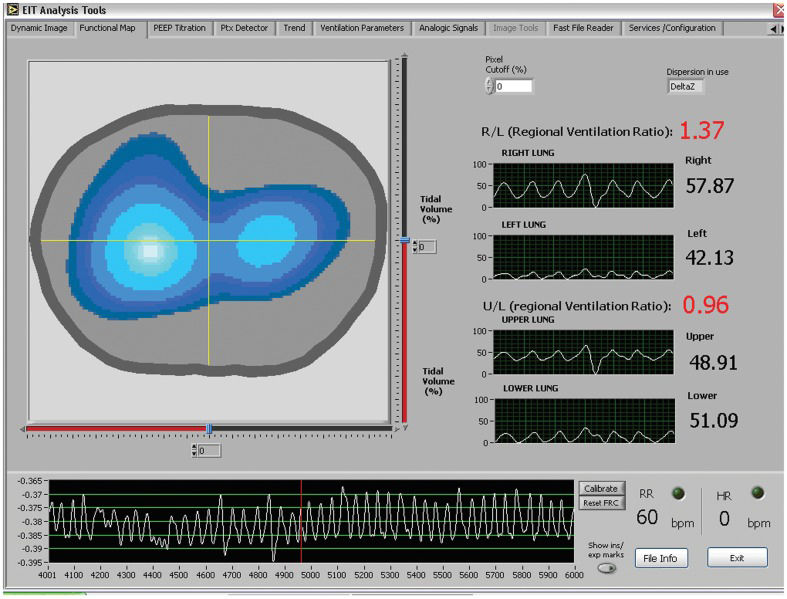
EIT measurements and data analysisA 16-electrode EIT belt was specially designed to fit VLBW infants who had thorax diameters as small as 17 cm. The EIT used an Enlight® technology model DX-1800 apparatus that sampled at 50 Hz (Dixtal, Sao Paulo, Brazil). EIT images were continuously recorded and reconstructed based on a 3-D finite element mesh under decremental PEEP levels (8, 7, 6 and 5 cmH20; 3 minutes for each step). The ventilation ratio between the dependent and the non-dependent lung areas (upper/lower ratio, U/L) was continuously calculated. Because of the variability of the impedance change caused by the typical respiratory pattern of VLBW infants during spontaneous assisted breathing, as well as variability arising from the patients' movements, only stable respiratory cycles defined by at least two of the researchers were used to calculate the PEEP that promoted the best ventilation homogeneity (VH), which was considered an upper/lower ratio of 1, as previously described (Figure 1.
The “functional map” (FM) screen used to evaluate upper/lower ventilation ratio (U/L) during image acquisition and off-line analysis and to determine ventilation homogeneity (VH). U/L (regional ventilation ratio) displays the calculated ratio at a certain window of data collection. Of note is the variability of the impedance presented in the lower black box, which was detected during the first half of data acquisition.
Extubation failure was defined as the need for reintubation within 72 hours after tube removal. Patients were reintubated if they needed FiO2≥0.6 to maintain arterial oxygen saturation between 88-94%, PaCO2≥70 mmHg or if they presented apnea that required bag mask ventilation for stabilization.
A thorax x-ray and ABG analysis were performed six to twelve hours after extubation. Evidence for atelectasis was specifically checked in the x-ray images. Oxygen index (OI), alveolar-arterial oxygen difference (A-a), arterial/alveolar ratio (a/A) and pH and paCO2 levels were calculated and compared.
The mean and standard deviation were used to describe data. Continuous data were analyzed using Student-t test or the Mann-Whitney test as appropriate. R statistical software (version 2.10.1) was used for all analyses. p≤0.05 was considered statistically significant.
RESULTSAfter the non-invasive, radiation-free and harmless EIT method was explained, one family declined to consent. Five other eligible infants were also not enrolled because they were extubated without the presence of a member of the study team at the NICU.
The demographic characteristics of the fourteen patients included in this study are shown in Table 1. The mean value and standard deviation of the body weight were 940±205 g, gestational age was 28.1±2.6 weeks and age at EIT evaluation was 7.5±10.8 days. Extubation failure was observed in three infants (21.4%). One patient was reintubated for central apnea without evident deterioration of lung compliance. Reintubation because of respiratory distress after tube removal occurred in two patients. Both patients were ventilated for more than four weeks prior to EIT evaluation and were diagnosed as having bronchopulmonary dysplasia. The mean PEEP level determined by the EIT that resulted in the best VH was 6.3±1.1 cmH2O, which was significantly different from 5.2±0.4 cmH2O, which was the CPAP empirically applied after extubation (p = 0.002). The two patients in which extubation failed had a best PEEP = 6 cmH2O and were extubated to a CPAP of 5 and 6 cmH20, respectively. Of all EIT signals collected, 70.2% of the data were considered appropriate to be analyzed. ABG analysis, oxygenation indices, the x-ray pattern and the other preliminary outcomes are presented in Table 2. No side effects, either related to the use of the EIT device in these infants, including skin lesions secondary to electrodes, or related to the infant manipulation, were found. Figure 2 corresponds to EIT images representing the loss of ventilation in the dependent zone after a PEEP reduction in one of the studied patients.
Demographic characteristics of the 14 newborns included in the study.
| Infant | Sex | Apgar 5 | Prenatal steroids | BW (g) | GA (wk) | EITd (days) | Surfactant |
|---|---|---|---|---|---|---|---|
| 1 | F | 10 | Yes | 860 | 26.0 | 1 | No |
| 2 | F | 8 | Yes | 1055 | 33.0 | 1 | No |
| 3 | M | 10 | Yes | 1060 | 29.9 | 5 | Yes |
| 4 | M | 10 | Yes | 1290 | 30.4 | 5 | Yes |
| 5 | F | 9 | Yes | 1175 | 28.6 | 1 | Yes |
| 6 | M | 9 | Yes | 1185 | 31.6 | 6 | Yes |
| 7 | M | 6 | Yes | 675 | 24.4 | 29 | Yes |
| 8 | M | 6 | No | 990 | 28.0 | 8 | Yes |
| 9 | F | 5 | No | 930 | 26.4 | 2 | Yes |
| 10 | M | 8 | Yes | 920 | 25.6 | 1 | Yes |
| 11 | M | 9 | Yes | 560 | 25.0 | 35 | Yes |
| 12 | F | 6 | Yes | 880 | 26.7 | 8 | Yes |
| 13 | F | 8 | Yes | 855 | 30.7 | 1 | Yes |
| 14 | F | 8 | No | 730 | 27.1 | 2 | Yes |
BW birth weight, GA gestational age at birth, EITd day of life when EIT was performed.
Secondary outcomes among the 14 newborns included in the study.
| Mean±SD | Maximum | Minimum | |
|---|---|---|---|
| Atelectasis after extubation (%) | 0.0(0.0%) | - | - |
| Oxygen index | 4.4±2.2 | 8.0 | 1.6 |
| Alveolar-arterial oxygen difference (mmHg) | 129±64 | 237.9 | 43.5 |
| Arterial/alveolar ratio | 0.315±0.121 | 0.580 | 0.130 |
| pH (-logH+) | 7.354±0.070 | 7.470 | 7.240 |
| PaCO2 (mmHg) | 39.2±9.6 | 62.9 | 28.0 |
Panels A and B show an example of ventilatory modification that was detected by electrical impedance tomography after PEEP reduction. The best ventilation homogeneity is in panel A, with an upper/lower ratio (U/L) of 1.05. After PEEP reduction, panel B presents a U/L ratio of 2.22 with collapse of the dependent area of the left lung. In both situations, the right lung was more aerated than the left lung.
This feasibility study showed that it is possible to evaluate air distribution during spontaneous assisted ventilation in VLBW infants with the use of EIT and also determined the PEEP that results in the best VH. To our knowledge, the use of dynamic images to evaluate different PEEP levels and their effects on preterm lungs in infants receiving assisted conventional mechanical ventilation has never been reported before.
Similarly to other studies using controlled ventilation, both in adult anesthetized patients with healthy lungs and in animal models of lung injury (21,22,24), we applied an index to define a more homogeneous air distribution between lung areas. However, there is a concern that heterogeneity is a physiological phenomenon in patients who are to be extubated and who also present minimal or no lung collapse (25).
The use of EIT to describe air distribution during mechanical ventilation in preterm infants has only recently been reported, in which the age of the infant during volume-targeted ventilation (14) and the application of surfactant (26) impact the distribution of tidal ventilation.
In the small and heterogeneous population studied, the mean value of the best PEEP determined by EIT during assisted ventilation was higher than the usual pressures applied with CPAP after tube removal at our NICU. Assuming that extubation failure may be reduced if the pressures that determine the best VH are efficiently applied using non-invasive ventilation, the maintenance of a desired CPAP level is highly desired. If this is true, however, in contrast to invasive ventilation, part of the pressure may leak through the mouth, esophagus or nasal prong. The EIT can be used to evaluate breathing patterns of non-ventilated neonates (16,27), and it could also possibly be used to titrate CPAP levels in extubated patients. However, this was not explored in our protocol. Despite these limitations, our results may be used as a reference for future studies that will evaluate EIT application in preterm infants who are considered ready for extubation. Although different CPAP apparatuses were used, previous data suggest that this factor does not influence the extubation success rate (9,28,29). The extubation failure found in this small sample of patients was in agreement with previous studies (6,7,10,25,29).
Variability of the VH index during spontaneous breathing was a hallmark observed in all patients studied (Figure 1. EIT evaluation performed with the use of muscle relaxation and sedation during controlled ventilation in animals and patients does not address this variability because all of the respiratory cycles behave similarly (13,15,21,22,24,30). Previous studies evaluating neonates have also described marked impedance variations during both assisted and unassisted respirations. These studies used very short and stable EIT data to evaluate and characterize air distribution among different lung areas (14,17,31). In contrast to this concept, we collected and analyzed the largest number of cycles that were unaffected by movements or artifacts. In doing so, almost 30% of the raw data was not used for interpretation. Our strategy is more time-consuming and can be biased by individual interpretation, but may better reflect the usual respiratory pattern of the neonates. A tool capable of automatically discarding impedance variations unrelated to air movement could facilitate EIT interpretation in spontaneous breathing neonates and is highly desired.
One interesting finding was the absence of a trend favoring non-dependent ventilation at lower levels of PEEP. This was in contrast to results in previous EIT studies that utilized controlled ventilation. There are at least two explanations for this observation. First, as the neonates were considered ready for extubation, their respiratory compliance was likely close to normal, which may have minimized the effects of lung recruitment observed in sicker lungs (30,32). Second, we studied only a narrow PEEP window because we were aware of the possible deleterious effects of using very high or low PEEP for the VLBW infants. A recent study showed that spontaneous non-ventilated preterm infants tended to ventilate non-dependent areas more than dependent areas (33) whereas ventilated infants had higher ventilation in the middle third of the chest (14).
The other analyzed outcomes of atelectasis after extubation and blood gas analysis did not show differences among the patients but only represent preliminary data because the sample studied was too small for clinical inferences.
EIT is still being adapted to generate high-quality images and information in small patients. Specific algorithms for image reconstruction must be developed to allow the correct interpretation of impedance variation in these extreme patients (34,35). The electrodes also need to be gentle on the skin of VLBW infants who are particularly prone to lesions and must also have a size capable of fitting around the infants' very small thoraxes. The spatial resolution of EIT images is affected by and directly related to the number of electrodes that are used (11,36).
Mechanical ventilation, which is used worldwide to increase the survival of many neonates in need, still relies on empirical protocols. The possibility to study ventilation in real time at the bedside without radiation and without high costs using EIT in these tiny and unstable patients deserves future trials.
AUTHOR CONTRIBUTIONSRossi FS and Rebello CM participated in original concept and writing of the manuscript and contributed to data acquisition. Yagui AC and Haddad LC contributed to data acquisition. Deutsch AA participated in the original concept and writing of the manuscript.
The authors thank Prof. Dr. Marcelo Britto Passos Amato and the Experimental Pneumology Laboratory – LIM 09, University of São Paulo, for support during this study.
No potential conflict of interest was reported.