Esophageal cancer staging has been performed through bronchoscopy, computerized tomography (CT), positron emission tomography (PET), and endoscopic ultrasound (EUS). Whereas CT and PET scan provide assessments of distant metastasis, bronchoscopy importantly diagnoses tracheobronchial involvement, complementing chest CT findings. EUS is the most accurate examination for T and N staging but is technically limited when tumoral stenoses cannot be traversed. Endobronchial ultrasound (EBUS) appears to present greater accuracy than EUS, CT, and bronchoscopy for assessing tracheobronchial wall involvement. EBUS has been recently associated with EUS for esophageal cancer staging in our unit.
OBJECTIVE:To compare EBUS findings in esophageal cancer patients without evident signs of tracheobronchial invasion on conventional bronchoscopy with EUS and CT.
METHODS:Fourteen patients with esophageal cancer underwent CT, conventional bronchoscopy, EUS, and EBUS for preoperative staging. All patients underwent EBUS and EUS with an Olympus® MH-908 echoendoscope at 7.5 MHz. Seven patients were eligible for the study according to the inclusion criteria.
RESULTS:The echoendoscope could not traverse tumoral esophageal stenosis to perform EUS in two patients, and invasion was effectively diagnosed by EBUS. In 4 (57%) of 7 patients EBUS revealed additional information to staging. In the remaining 3 cases the invasion findings were the same under both EUS and EBUS.
CONCLUSION:EBUS showed signs of tracheobronchial invasion not observed by conventional bronchoscopy, adding information to staging in most of the cases when compared with CT and EUS.
Esophageal cancer is a disease whose clinical manifestations generally occur in the advanced stages. Due to the distensibility of the esophagus, dysphagia occurs when approximately 2/3 of the esophageal lumen is involved. Conversely, absence of a serous layer facilitates tumoral invasion into adjacent structures. Consequently, only 20% of patients are able to undergo curative surgery.1,2 The most frequent incurable causes are tracheobronchial involvement and metastases into cervical and abdominal lymph nodes, liver, and lung.3,4 Lesion staging assumes a fundamental importance in therapeutic planning because of the great number of incurable occurrences of esophageal cancer.
Esophageal carcinoma staging is performed by bronchoscopy, computerized tomography (CT) scan and endoscopic ultrasound (EUS). Positron emission tomography (PET) scan is used in some centers with a diagnostic accuracy rate of approximately 74%, similar to that of CT.5 Whereas real-time EUS-guided puncture is the most accurate examination for tumor (T) and nodal (N) staging, with a sensitivity of approximately 85% and 75%, respectively,6,7 CT provides an assessment of distant metastases. Due to the intimate contact of the esophagus with the tracheobronchial tree, assessment of the possible involvement of this organ represents one of the steps for staging. Therefore, EUS is an accurate method for evaluating esophageal tumor invasion into adjacent organs.8
Despite the high EUS sensitivity and specificity in T staging of esophageal neoplasias, the presence of tumoral obstruction in the esophageal lumen can prevent the progression of the echoendoscope in up to 30% of the cases, making the performance of the procedure impossible.9,10 Endobronchial ultrasound (EBUS) can be used in these situations with the objective of staging the area adjacent to the tumor, including the tracheobronchial wall and mediastinal lymph nodes. Recent studies have demonstrated that EBUS has a great accuracy in the study of tracheobronchial invasion by esophageal neoplasia when compared to conventional bronchoscopy, CT and EUS,11,12 justifying the use of the method in this group of patients.
The aim of this study was to describe and compare EBUS and EUS findings in a group of patients with esophageal cancer and no evident signs of tracheobronchial invasion on conventional bronchoscopy.
PATIENTS AND METHODSThe study was approved by the Ethics and Research Committee of the Gastroenterology Discipline of Hospital das Clínicas of São Paulo University Medical School (HC-FMUSP). All patients diagnosed with esophageal neoplasia who fulfilled the inclusion criteria according to the study protocol were followed in the outpatient clinic or ward of the Esophagus Surgery Unit of the Clinical Surgery II Division. A group of 14 patients with esophageal cancer underwent CT, conventional bronchoscopy, EUS, and EBUS in HC-FMUSP. EUS and EBUS examinations were performed in the Gastrointestinal Endoscopy and Respiratory Endoscopy Units of HC-FMUSP.
Inclusion and Exclusion CriteriaSeven patients were eligible for the study according to the following inclusion criteria: over 18 years old and histopathological diagnosis of thoracic and cervical esophageal neoplasia with no evident signs of invasion into the tracheal or bronchial wall on conventional bronchoscopy. These patients underwent CT, EUS, and EBUS for preoperative staging.
Patients with cardiorespiratory instability diagnosed with tracheobronchial tree invasion on conventional bronchoscopy and those who had undergone prior treatment with chemotherapy, radiotherapy, or curative surgery were excluded.
Bronchoscopy, Endoscopic Ultrasound, and Endobronchial UltrasoundBronchoscopy for respiratory tree staging was performed under intravenous sedation. EUS and EBUS procedures were performed under deep sedation assisted by anesthesiologists. During the procedures, patients were monitored for cardiac and respiratory function. Laryngeal masks were used to perform EBUS, which made the passage of the device into the lower airways easier and allowed simultaneous ventilation during the procedures. EUS and EBUS examinations were performed by experienced endoscopists and bronchoscopists.
An Olympus® videobronchoscope was used to perform conventional bronchoscopy along with an Olympus® MH-908 (Olympus Medical System Corporation, Tokyo, Japan) echoendoscope without an optical system but with a channel for guide-wire passage. A 7.5-MHz ultrasound transducer enabled evaluation with an echographic depth of approximately 15 mm.
The conventional videobronchoscope was introduced through a laryngeal mask for guide-wire positioning to guide the introduction of the echoendoscope. The echoendoscope was positioned at the esophageal neoplasia level, and a silicone balloon, which covers the transducer, was intermittently filled with sterile water to produce an acoustic window. Echographic images through the trachea were assessed by the echoendoscopy and bronchoscopy team and documented in digital photos and films.
Transesophageal endoscopic ultrasound was subsequently performed in the same way. The conventional videoendoscope was introduced into the esophagus, and a guide-wire was positioned allowing the echoendoscope passage to the neoplasia level. Echographic images through the esophagus were assessed by the echoendoscopist and documented in digital photos and films.
In conventional laringealtracheobronchoscopy, the following changes were documented: mobility of the vocal folds, bulges in the posterior tracheal and bronchial wall, synchronous tumors, mucosal infiltration, or presence of fistula. Vocal fold paralysis, suggesting involvement of the laryngeal recurrent nerve, infiltration of the respiratory mucosa and fistula were considered as marks of invasion into the tracheobronchial tree by an adjacent tumor.13 The ultrasound criterion used to determine invasion in the respiratory tree by an esophageal neoplasia was the interruption of the tracheobronchial adventitia characterizing infiltration by an adjacent tumor.11,12
RESULTSThe mean age of the group studied was 59 ± 3.3 years old. Upper gastrointestinal endoscopy was performed in all patients, and in two cases, tumoral obstructions of the esophagus did not allow echoendoscope passage.
On conventional bronchoscopy, no mucosal infiltration or fistulas were observed in the seven cases included. A bulge of the posterior tracheal wall and/or left main-stem bronchus, although covered by normal mucosa, was observed in five cases (71.4%) but, none of those cases were considered to constitute invasion. Vocal fold paralysis was observed in one case. Bronchoscopy was normal in two cases (28.57%).
CT scan revealed peri-esophageal thickness with no evident signs of tracheobronchial tree invasion in six cases (85.7%) and an infiltrative lesion in the middle third of the esophagus with invasion of the left main-stem bronchus, which was not visible during the conventional bronchoscopy examination.
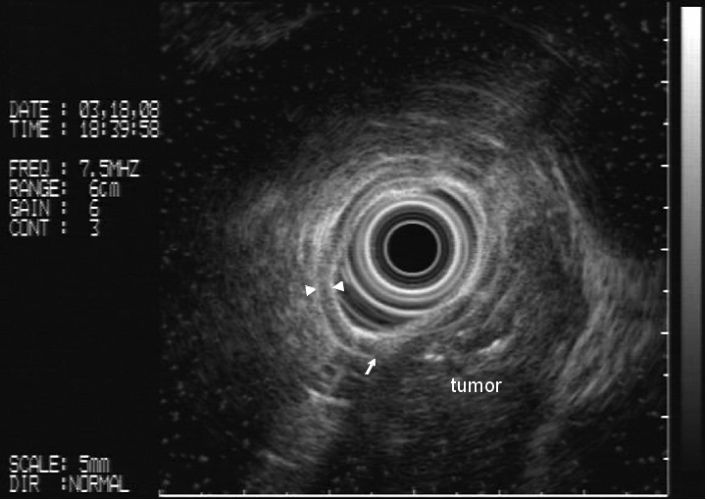
EUS could not be performed in two cases (28.6%) due to esophageal tumoral stenosis. In five cases, esophageal EUS was performed, revealing tracheobronchial invasion in two patients (28.6%) and an absence of invasion in two other cases (Figure 1). The limitations of this method were revealed when the acquisition of echographic images of the invasion in one case could not be clearly defined.
EBUS was performed in all seven patients, revealing invasion in six of them (85.71%). EUS and EBUS findings concurred in three patients (60%), confirming tracheobronchial invasion in two cases (Figure 2) and excluding invasion in one. EBUS was successfully performed revealing tracheobronchial invasion in the two cases in which EUS could not be performed due to tumoral stenosis. EUS could not define invasion in one case in which EBUS revealed invasion. Of the seven cases studied, EBUS revealed tracheobronchial invasion in six, concurring with CT in one case. In two cases, conventional bronchoscopy showed normal and EBUS revealed invasion. A description of all cases and a summary of the results obtained from this study are presented in Table 1.
Characteristics of patients studied and results of the tests performed.
| Patient | Age | CT scan | UGI endoscopy | Bronchoscopy | EUS | EBUS |
|---|---|---|---|---|---|---|
| 1 | 58 | Parietal thickness of esophagusNo signs of invasionRight superior paraesophageal lymphadenomegaly | SCC 18 cm SDAImportant stenosis | LVF ParalysisBulge of proximal trachea with normal mucosa | Not performed (obstructive esophageal tumor) | Tracheal invasion by esophageal lesionLymph node adhered to the mass |
| 2 | 56 | Parietal thickness of esophagusNo signs of invasion | SCC 28 cm SDAStenosis | Bulge of distal trachea and LMB, with normal mucosa | Tracheal invasion by esophageal lesion Lymph nodes | Tracheal invasion by esophageal lesion |
| 3 | 58 | Infiltrative stenotic lesion of middle 1/3 of esophagus with signs of invasion | SCC 24 cm SDAImportant stenosis | Bulge of distal trachea and LMB, with normal mucosa | Not performed (obstructive esophageal tumor) | Tracheal invasion by esophageal lesion |
| 4 | 56 | Parietal thickness of proximal esophagusNo signs of invasion | Proximal cricopharyngeal SCC | Normal | Tracheal invasion by esophageal lesion 3 lymph nodes | Tracheal invasion by esophageal lesion |
| 5 | 62 | Parietal thickness of esophagusNo signs of invasion | SCC at 26 cm of SDA | Bulge of left mainstem bronchus with normal mucosa | Trachea not invaded by neoplastic lesion | Tracheal invasion by esophageal lesion |
| 6 | 65 | Parietal thickness of esophagus in middle 1/3 No signs of invasion Subcarinal, paratracheal, supraclavicular lymph nodes | SCC at 25 cm of SDA | Normal | No definition of invasion or tracheal wall (EUS image limitation) | Tracheal invasion by esophageal lesion |
| 7 | 59 | Infiltrative parietal thickness of the esophagus in contact with LMB | SCC at 26 cm of SDA Stenosis | Bulge of posterior wall in distal trachea | No tracheal invasion by esophageal lesion | Invasion-free tracheobronchial tree |
Abbreviations Used: CT (computed tomography), UGI endoscopy (upper gastrointestinal endoscopy), EUS (endoscopic ultrasound), EBUS (endobronchial ultrasound), SCC (squamous cell carcinoma), SDA (superior dental arch), LVF (left vocal fold), LMB (left main bronchus).
Assessment of tracheobronchial tree invasion by esophageal cancer provides one of the most important pieces of information for therapeutic planning. Diagnostic methods such as CT scan, conventional bronchoscopy, and EUS are currently used for this purpose; however, none of them have a satisfactory accuracy.11,12 Nishimura et al.12 reported accuracy rates of 78% and 58% for conventional bronchoscopy and CT, respectively, for invasion diagnosis criteria. During conventional laringealtracheobronchoscopy, the finding of vocal fold paralysis almost excludes the possibility of curative surgery. However the objective of our study was to analyze just the tracheobronchial wall invasion. Nonetheless, a bulge of the posterior tracheobronchial wall or minimal mucosal changes (enanthema, edema) does not confirm neoplasic invasion of the wall.13 Bronchoscopy seems to be a good specific test only when there is a visible lesion in the airway lumen.13 In our study, just one patient had suggestive findings of infiltrative tracheobronchial disease upon CT and EBUS findings. Infiltration was not diagnosed by EUS, due obstructive esophageal disease. The remaining patients had only partial thickening of the esophagus upon CT, and one of them did not have invasion according to EBUS or EUS. It is important to reinforce the importance of different methods in establishing pre-operative staging of this pathology.
With the advent of miniprobe associated with endoscopy, new methods such as EUS and EBUS have elevated diagnostic accuracy rates for tracheobronchial invasion to 85% and 91%, respectively.12 In the present study, six patients did not show classical signs of tracheal or bronchial invasion upon CT scan, but invasion was observed in two cases by EUS and in five by EBUS. CT results concurred with EBUS in two cases (28.57%).
Studies have demonstrated that EBUS is feasible in all cases of esophageal cancer staging, whereas EUS presents limitations in cases of esophageal obstruction by tumors.11 In the present series, EUS could not be performed in 28.57% of the cases due to tumoral stenosis, and only when EBUS was performed was respiratory tree invasion revealed.
Echographic images of the anterior tracheobronchial wall by EBUS (with 20-MHz probe) have been divided into seven layers: mucosal (high density), submucosal (low density), endochondral (high density), cartilage (low density), perichondral (low density), connective tissue (low density), and adventitial (low density) layers. Likewise, the posterior wall is divided into three layers: mucosal (high density), submucosal (low density) and adventitial (high density) layers.11 Involvement of tracheal or bronchial adventitia is considered diagnostic of respiratory tree invasion.11,14 Although the use of 20-MHz miniprobes for this purpose has been described in the literature, a 7.5-MHz probe was used in our study, which limited but did not prevent visualization of the different layers of the posterior tracheobronchial wall. Consequently, EBUS alone was responsible for the diagnosis of tumoral invasion in three of the seven cases studied. A prior study conducted by Bowrey et al.15 also used a 7.5-MHz esophagoprobe to assess invasion into the tracheal wall in esophageal cancer staging through EUS, with 90% accuracy.
As for the safety of the EBUS procedure, although occlusion produced by the balloon in the tracheal or bronchial lumen was observed, the test was performed in all cases without respiratory or hemodynamic dysfunction. The use of the laryngeal mask was important to ensure ventilation and oxygenation during the procedure.
Tracheal invasion diagnosis in the cases reported was not confirmed by operative or histopathological findings because the patients with such findings were referred to radiotherapy and chemotherapy. Nevertheless, the information obtained had an impact on their therapeutic planning. Consequently, EBUS can play an important role in the restaging of these patients after radiotherapy and chemotherapy in the search for candidates for rescue esophagectomy.
CONCLUSIONEBUS showed signs of tracheobronchial invasion not observed by conventional bronchoscopy. It added information to staging in most cases when compared with EUS and CT results. The present case series represents the outset of EBUS experience in Brazil, and despite the restricted number of patients, this series proved to be feasible and safe.