To evaluate and compare the efficiency of humidification in available heat and moisture exchanger models under conditions of varying tidal volume, respiratory rate, and flow rate.
INTRODUCTION:Inspired gases are routinely preconditioned by heat and moisture exchangers to provide a heat and water content similar to that provided normally by the nose and upper airways. The absolute humidity of air retrieved from and returned to the ventilated patient is an important measurable outcome of the heat and moisture exchangers’ humidifying performance.
METHODS:Eight different heat and moisture exchangers were studied using a respiratory system analog. The system included a heated chamber (acrylic glass, maintained at 37°C), a preserved swine lung, a hygrometer, circuitry and a ventilator. Humidity and temperature levels were measured using eight distinct interposed heat and moisture exchangers given different tidal volumes, respiratory frequencies and flow-rate conditions. Recovery of absolute humidity (%RAH) was calculated for each setting.
RESULTS:Increasing tidal volumes led to a reduction in %RAH for all heat and moisture exchangers while no significant effect was demonstrated in the context of varying respiratory rate or inspiratory flow.
CONCLUSIONS:Our data indicate that heat and moisture exchangers are more efficient when used with low tidal volume ventilation. The roles of flow and respiratory rate were of lesser importance, suggesting that their adjustment has a less significant effect on the performance of heat and moisture exchangers.
The goal of artificially preconditioning inspired gases delivered to ventilated, intubated patients is to provide a heat and water content at the level of the carina that is similar to that usually provided by the nose and upper airways.1 Absolute humidity (AH) is the amount of water vapor per unit volume of gas mixture.2 When a gas contains its respective total capacity for water vapor for a given temperature, the gas is termed “saturated” (accordingly, AH at saturation is highly dependent on the gas temperature).
Relative humidity (RH) is the ratio of a given AH relative to the maximal capacity for water vapor of that gas (again, directly dependent on gas temperature).1 A RH of less than 100% represents a humidity deficit or a burden on the airways of the patient. The task of preconditioning to avoid this deficit can be accomplished by heated humidifiers (HH or active humidifiers) or by heat and moisture exchangers (HME or passive humidifiers).3–6
The AH of the air retrieved from and returned to the patient is an important indicator of the humidifying performance of an HME.7 This is important since endotracheal tube/tracheotomy occlusions may occur when humidity delivery is insufficient.8–11
There are three basic types of HME: hygroscopic, hydrophobic and combined (hygroscopic-hydrophobic).12 This distinction is important for many reasons; for instance, they lead to distinct effects in terms of ventilatory mechanics.13 Hygroscopic HME devices contain materials of low thermal conductivity impregnated with a hygroscopic chemical. Hydrophobic HME units have a larger surface area due to pleating of the material14 and feature a substance covering the filter that prevents the water’s exodus during exhalation and also serves as an efficient microbiological filter.15,16 Combined HME units (hygroscopic-hydrophobic) exhibit humidification performance consistent with the bacterial retention properties of the filter membrane.7,12,17 For the combined HME, the hygroscopically-treated material is located between the patient’s airway and the filter.
Reports have suggested that increasing the tidal volume,18–23 flow rate,18,24 or minute ventilation9,18,23 will decrease the humidification efficiency of an HME. A consistent measure of humidifying efficiency has not been determined to date for HME use. Testing of humidification efficiency for available HME units under a range of ventilatory conditions has not been reported to date. Therefore, we aimed to evaluate and compare the humidifying efficiency of these adjuncts under conditions of varying tidal volume, respiratory rate, and flow rate.
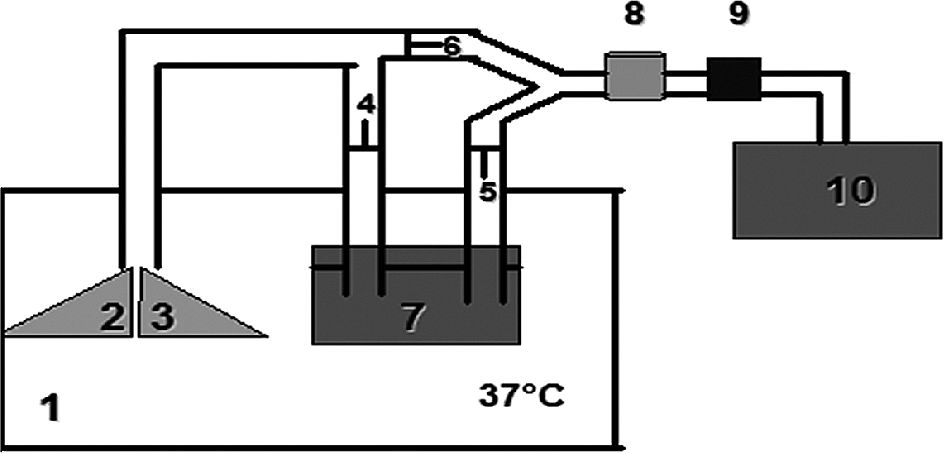
MATERIALS AND METHODSA respiratory system analog (Figure 1) was constructed using preserved swine lungs (BioQuest Inflatable Lungs, NASCO, Ft. Atkinson, WI, USA) in a large plastic box maintained at 37°C. The lungs were arranged to simulate the bifurcation structure of in vivo lungs. To serve as self-humidifying lungs, the tubing circuitry was constructed to route airflow through a cascade-type humidifier after which it ventilated the swine lungs (both within the plastic box maintained at 37°C using a commercial hot-air dryer).
Mechanical model. Components include: a large plastic box maintained at 37°C (1), preserved swine lungs (2, 3) and a cascade-type humidifier (7) inside the box. Three unidirectional valves (4, 5 and 6) were inserted within the tubing section external to the box (representing the airway) to direct flow through the humidifier prior so that it could ventilate the lungs. In this same simulated airway segment, a sensor (Vaisala, HMI 32, Woburn, MA, USA) (8) was positioned to detect AH and temperature. The HME (9) under test was individually installed using a random sequence for each testing period. A mechanical ventilator (10) was used to simulate different ventilatory conditions.
The system analog was connected to a mechanical ventilator (840, Nellcor Puritan Bennett, Carlsbad, CA, USA) used to simulate ventilatory conditions by varying the tidal volume (VT), respiratory rate (f), and flow rate during volume control mode ventilation (Table 1). Positive end-expiratory pressure (PEEP) was not used.
Ventilator settings employed and the corresponding percentage recovery of absolute humidity (%RAH) for each HME
| VT (mL) | Flow-rate (L/min) | f (/min) | FiO2 | %RAH | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| G2S | Portex | HCH | Pall | G light | G compact | Hygrobac S | Hygroster | ||||
| 200 | 30 | 10 | 0.5 | 94.4 | 95.5 | 95.2 | 95.1 | 94.1 | 94.7 | 96.4 | 94.2 |
| 500 | 30 | 10 | 0.5 | 88.3 | 85.5 | 88.9 | 88.3 | 87.9 | 89.7 | 92.3 | 85.8 |
| 1000 | 30 | 10 | 0.5 | 80.5 | 74.9 | 76.4 | 68.8 | 79.9 | 81.7 | 85.4 | 74.5 |
| 500 | 30 | 5 | 0.5 | 87.8 | 85.6 | 86.3 | 83.6 | 86.4 | 89.0 | 91.0 | 83.4 |
| 500 | 30 | 10 | 0.5 | 88.5 | 85.8 | 87.6 | 84.8 | 87.7 | 90.4 | 92.0 | 85.0 |
| 500 | 30 | 20 | 0.5 | 90.2 | 85.9 | 89.6 | 87.3 | 88.2 | 91.5 | 92.8 | 87.1 |
| 500 | 30 | 10 | 0.5 | 88.0 | 85.9 | 87.4 | 85.0 | 87.8 | 90.3 | 92.2 | 87.1 |
| 500 | 60 | 10 | 0.5 | 89.1 | 87.1 | 89.2 | 87.5 | 88.5 | 91.6 | 92.9 | 90.2 |
| 500 | 90 | 10 | 0.5 | 90.5 | 87.4 | 90.1 | 90.8 | 90.0 | 92.5 | 93.7 | 92.0 |
Note: VT = tidal volume; f = respiratory rate; FiO2 = fraction of inspired oxygen; %RAH = percentage recovery of absolute humidity
The testing region featured a section of tubing and connectors external to the box that represented the airways. In this airway segment, eight different HME units were sequentially tested, one of each of the following:
- •
Hygroscopic
HUMID-VENT 2S (G2S) - Gibeck, Upplands-Väsby, Sweden
THERMOVENT 1200 (Portex) - SIMS Portex Ltd, Kent, United Kingdom
Hygroscopic Condenser Humidifier (HCH) - Newmed, Bromma, Sweden
- •
Hydrophobic
BB100MFS (Pall) - Pall, Cornwall, United Kingdom
- •
Hygroscopic-hydrophobic
HUMID-VENT FILTER LIGHT (G light) - Gibeck, Upplands-Väsby, Sweden
HUMID-VENT FILTER COMPACT (G compact) - Gibeck, Upplands-Väsby, Sweden
HYGROBAC S DAR (Hygrobac S) - Mallinckrodt Medical, Mironda, Italy
HYGROSTER DAR (Hygroster) - Mallinckrodt Medical, Mironda, Italy
The dead-space volumes of each of the tested HMEs were recorded as listed in the manufacturers’ specifications.
A thermister/hygrometer (Vaisala, HMI 32, Woburn, MA, USA) was positioned between the HME and the respiratory system analog to continuously measure inspired/expired relative humidity and temperature (Figure 1).
Data were transmitted to a chart recorder (Astro-Med, Inc. Astro-Med Industrial Park, West Warwick, RI, USA) for analysis. Box temperature was continuously monitored using a thermostat (Digitec, model 5810, United Systems Corporation, Dayton, OH, USA) and the hot-air dryer was adjusted to maintain the box temperature at 37°C. A stabilization period of one hour was allowed for each HME to reach an “efficient” steady state, prior to the actual measurements being recorded. After this time period, we waited for 10 respiratory cycles before measuring RH and temperature (steady-state values had consistently stabilized by the fourth respiratory cycle).
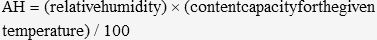
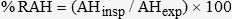
AH and percentage recovery of absolute humidity (%RAH) for each HME were determined using the following formulas:
Where AHinsp refers to the absolute humidity of the inspired air and AHexp is the equivalent measurement during expiration.
RESULTSWe initially recorded repeated measurements under different respiratory parameters with different HMEs, and our model showed excellent reproducibility, with a standard deviation for AH of 0.66 mg H2O/L. Our measurements were considered statistically different (p < 0.05) if they differed from one another by more than twice this standard deviation (1.32 mg H2O/L) – the so-called 95% confidence interval.25 In this manner, many comparisons were found to be statistically different - their clinical importance is addressed in the Discussion section.
HME models differed slightly in their ability to maintain humidity levels except during high-tidal-volume ventilation, when differences among the HME units were more pronounced. Hygrobac S exhibited a greater %RAH than the others.
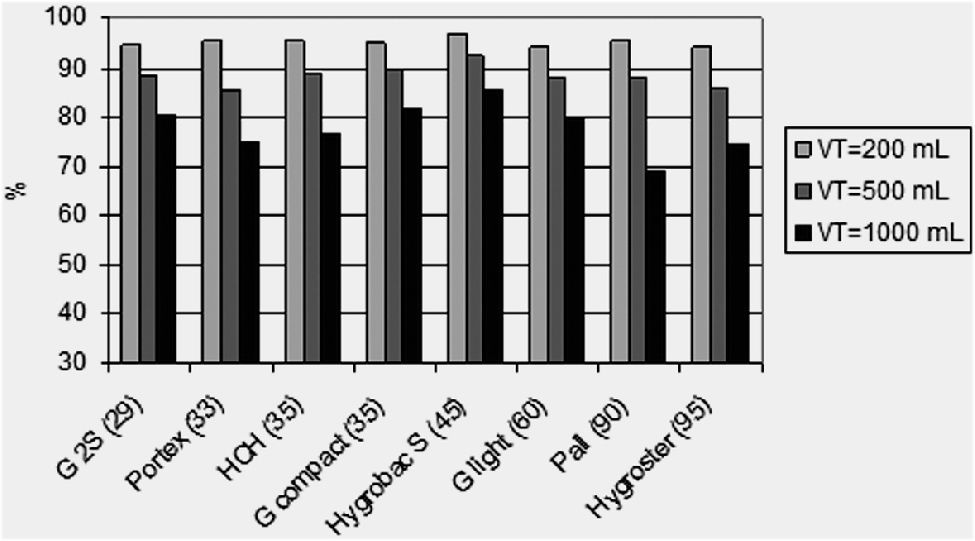
The %RAH for HME use with the following fixed parameters is shown in Figure 2 and in Table 1: flow rate = 30 L/min, f = 10/min, FiO2 = 0.5; when VT was delivered at 200, 500 and 1000 mL.
Effect of tidal volume (200, 500 and 1000 mL) in the context of %RAH. The dead-space volume for each HME is shown in parentheses and the HME units are listed in order of increasing dead-space volume. Overall, the HME models differed slightly in terms of their ability to maintain absolute humidity levels, except when a high tidal volume was delivered. There was an inverse relationship between the efficiency of humidification and tidal volume. Hygrobac S was the HME model with the greatest %RAH.
We observed that VT affected the ability of a given HME to maintain humidity; when VT increased there was a consistent reduction in %RAH, which was independent of the HME type (Figure 2, Table 1). At a VT of 200 mL, the %RAH for each HME was greater than 90%. With the VT set to 500 mL, each HME recovered more than 80% of AH. However, when the VT was set to 1000 mL, only 3 of the HME units recovered greater than 80% of AH; and in this scenario the Pall HME model exhibited the lowest %RAH (under 70%).
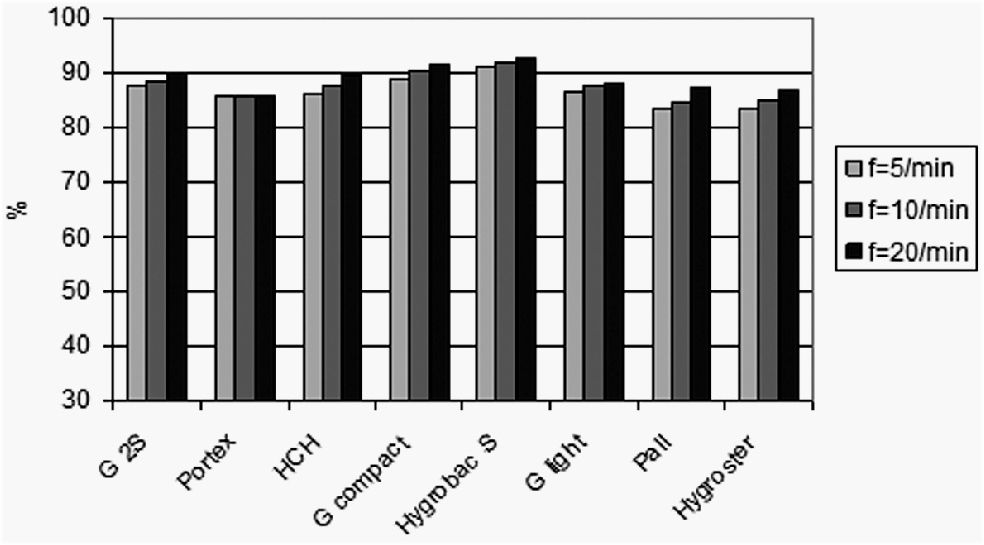
The %RAH for different respiratory frequencies is displayed in Figure 3 and Table 1. HME models differed slightly in their ability to maintain AH levels but, in general, %RAH did not change markedly with increasing frequencies given a VT of 500 mL.
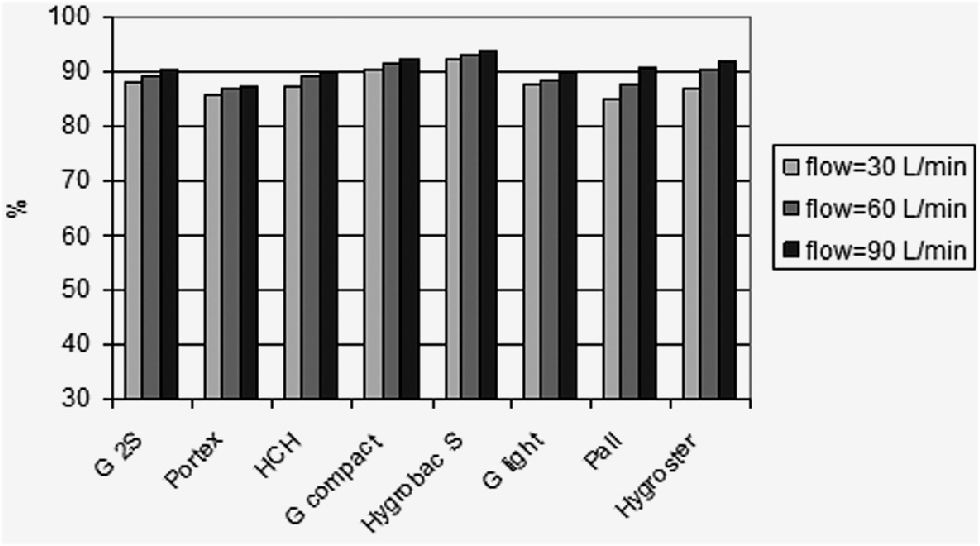
The effect of flow rate on %RAH is displayed in Figure 4 and Table 1. There were minor differences between HME models and the recovery of AH was not influenced by different flow rates. In our setting of a VT of 500 mL, greater flow rates did not negatively impact the ability of HME to maintain adequate levels of humidity.
DISCUSSIONOur study assessed the ability of currently available HME units to return heat and humidity to a simulated airway under a variety of ventilatory scenarios. The choice of HME models was based on previous research that focused on models the most commonly found in the largest hospitals of our city.
Previous data show that HME units recover heat and moisture during exhalation and return a significant portion of the heat and humidity during the subsequent inspiration. 14,17,26–29 Our data, however, suggest that the efficiency of this process was not very significantly related to flow and respiratory rates, although it was profoundly affected by increasing VT.
We also failed to identify any significant relationships between the type of HME and %RAH. HME performance was poorly correlated with the material in each HME, except in cases of high VT. In this particular situation the Pall HME, the only hydrophobic model, had a decreased %RAH of less than 70%.
These findings are somewhat consistent with the literature. Eckerbom and Lindholm20 reported a poor correlation between performance and internal HME volumes (deadspace), although Grolman et al.30 found that filter material and size influenced the HME moisture output efficiency.
The efficiency of HME in maintaining heat and humidity has been reported to be affected by the ventilator settings. Our data revealed an inverse relationship between the efficiency of humidification and the tidal volume.18–23 For a lower tidal volume of 200 mL, the HME appears to provide adequate humidification. However, the AH was consistently lower for a VT of 1000 mL as compared to 500 mL or 200 mL. Branson and Davis,23 Eckerbom and Lindholm20 and Wilkes22 also observed that HMEs delivered higher humidity when the VT was 500 mL as compared with 1000 mL in their lung model studies. We found that the most efficient HME was the Hygrobac S at all VT settings.
In our study, %RAH was nearly constant when we changed the respiratory rate and flow rate for each HME. Other studies have suggested that increasing minute ventilation decreases the efficiency of humidification by an HME.9,18,23 When we compared different frequencies, the efficiency of humidification remained nearly constant. The efficiency of humidification decreased when high minute ventilation was achieved by increasing the tidal volume. Our data suggest that the previously described minute ventilation effect on HME efficiency is due almost exclusively to the role played by VT.
When we changed the flow rate, we failed to observe changes in the humidification efficiency. Other studies18,24 found that flow rate was a performance-changing factor with higher gas flow-rates decreasing the efficiency of humidification recovery as provided by the HME. It is likely that singularities in the respiratory models between these studies and ours may account for the observed differences.
One limitation of our study is the fact that we collected our data in a respiratory system analog. Although we tried to control all possible pertinent variables, to directly translate our findings into the clinical scenario would be an oversimplification. Further studies at the ICU will probably help corroborate these data and evaluate their relevance in a clinical scenario.
ICU patients are a heterogeneous group and many patients receive positive pressure ventilation through oral or nasal endotracheal intubation or via tracheotomy. In spite of the trend towards a protective strategy that involves low tidal volumes, 31 some patients require high-tidal-volume ventilation. Our data suggest that the use of HH instead of HME should be considered for this subset of patients, in order to avoid the possibility of insufficient humidification and all potential associated complications.8–11
Our data also indicate that the role of flow and respiratory rate is of lesser importance; accordingly, adjustments to these parameters seem to exert only a small impact on the final HME performance.
CONCLUSIONSHME are more efficient when used with low-VT ventilation. The roles of flow and respiratory rate were of lesser importance, suggesting that their adjustment has a less significant effect on HME performance.