This study aimed to evaluate the accuracy and quality of healing of main corneal incisions in femtosecond laser procedures in cataract surgery.
MethodsIt was a prospective, non-randomized, investigator-masked study. A total of 37 eyes of 37 patients with indication for cataract surgery were separated into two groups in this prospective, nonrandomized study: Femto group, with incisions automated by femtosecond laser (18 eyes), and Phaco group, with incisions made using a keratome (19 eyes). The planned incisions were 2.2 mm wide and 1.65 mm long. The length of the incision and prevalence of endothelial gap, endothelial misalignment, and localized Descemet Membrane Detachment (DMD) were compared.
ResultsThe mean incision length was statistically higher in the Femto group in two examinations: 1.64 mm ± 0.16 vs. 1.43 mm ± 0.30 (p = 0.001) in Exam 1 (between 2 and 4 days) and 1.58 mm ± 0.22 vs. 1.27 mm ± 0.34 (p < 0.0001) in Exam 2 (between 1 and 3 months). No eye presented an endothelial gap in Exam 2. The endothelial gap was higher in the Femto group in Exam 1. In the two examinations, endothelial misalignment was lower in the Femto group, whereas the incidence of DMD was lower in the Femto group in the two examinations.
ConclusionsAutomated incisions with femtolaser presented a higher mean length and lower DMD prevalence compared to manual incisions with a keratome.
The femtosecond laser procedure in ophthalmology began with the performance of lamellar sections in laser in situ keratomileusis in refractive corneal surgeries.1 Subsequently, its use expanded to perform full-thickness sections of the cornea, enabling different corneal transplant formats.2
The first cataract surgery using a femtolaser was performed in Hungary in 2008.3 Currently, femtolaser is used in facectomy to perform corneal incisions, capsulotomy, and fragmentation of the lens nucleus.4-6
Femtolaser-assisted cataract surgery has advantages over the conventional technique, including reduced use of ultrasonic energy,5,7 decreased endothelial damage,4,5,7 reduced corneal edema in the postoperative period,5 and performance of capsulotomy8 and more precise corneal incisions.9,10
However, the femtolaser procedure has some disadvantages in relation to the conventional technique, including increased prostaglandin levels in the anterior chamber;5 high cost;6 and positioning of the incisions farther from the limbus, toward the clear cornea, which may increase the risk of astigmatism.11
The corneal incision influences the intraocular manipulation during cataract surgery and the patient's visual result.12 However, a definitive consensus on the ideal parameters for constructing a high-quality incision has yet to be established.
Anterior Segment Optical Coherence Tomography (AS-OCT) obtains images of the cornea, measures the incision length, and is used to identify complications, such as incomplete sealing, Descemet Membrane Detachment (DMD), and retraction of the corneal endothelial face near the limbus.10,13
This study aimed to evaluate the accuracy and quality of healing of main corneal incisions in femtosecond laser procedure in cataract surgery compared with keratome incisions in the conventional phacoemulsification technique.
Patients and methodsThis prospective, non-randomized, investigator-masked study was approved by the ethics committee of the Universidade de São Paulo, and all patients provided informed consent to participate in the study, following the guidelines established in the Declaration of Helsinki.
All participants were submitted to preoperative ophthalmologic evaluation. A total of 37 eyes of 37 patients with indication for cataract surgery were allocated into two groups: 19 eyes were assigned to the group submitted to incision using a keratome blade and conventional phacoemulsification (Phaco group) and 18 eyes were assigned to the group with incisions, capsulotomy, and fracture of the lens core with femtosecond laser (Femto group).
The study compared the incision length, as well as the prevalence of endothelial gaps, endothelial misalignment, and localized Descemet Membrane Detachment (DMD).
Surgical techniqueAn experienced surgeon (R.C.H.) performed all surgeries with topical anesthesia. In the Femto group, the femtosecond laser platform (LensX®, Alcon Laboratories, Inc.) was used. Approximately 5 min prior to laser use, a drop of 0.025 %–0.3 % naphazoline hydrochloride and pheniramine maleate (Claril, Alcon Laboratories, Inc.) was instilled to decrease subconjunctival bleeding due to eye suction. After sucking the eye, the main and accessory incisions were adjusted toward the clear cornea, anterior to the limbus. The standard configuration of the main incision was as follows: temporal axis, trapezoid tri-planar architecture, 2.2 mm wide on the epithelial surface and 2.3 mm on the endothelial face, 1.65 mm long, and tunnel with entry angle of 70° and exit angle of 90° After completion of the laser, the residual adhesions of the corneal stromal fibers were dissected with a spatula.
In the Phaco group, the 2.2-mm-wide main incision was made with a disposable keratome (Bisturi Medical 2.2 M, GeeEdge Medical Instrument Co., Ltd., China), temporally, in a clear cornea. The planned architecture of the incision was biplanar arched, in the clear cornea, with an objective length of 1.65 mm. The definition of the programmed length was based on studies that demonstrated safety in rectangular-shaped incisions, with the tunnel long enough to generate a valvular effect and make it self-sealing, preventing the influx, and reflux of fluid from the anterior chamber.
The surgery proceeded with the traditional phacoemulsification and the stop-and-chop technique. In the end, the main and accessory incisions were hydrated with balanced saline, and a sponge (PVA Eye Spear, Cenefom Corp., Taiwan) was used to press the anterior flap and check for leakage. In case of a positive Seidel sign, the hydration of the stroma was repeated until the leak was stopped.
AS-OCTThe images of corneal incisions were obtained by a single masked examiner who used the AS-OCT software (Cirrus, Carl Zeiss Meditec AG). The endothelial gap and DMD appear in the early postoperative period and persist for up to 3 months.14 Retraction of the posterior corneal flap at the incision site appears in 33.3 % of the eyes between 2 and 3 wk.14 Based on these results, the examination process occurred in two periods: between 2 and 4 days after surgery and between 1 and 3 months after surgery. The objective was to record images with the following characteristics: incision entry and exit site, main incision site with the largest corneal thickness, changes in the endothelial surface of the cut, and DMD.
Qualitative and quantitative evaluation of AS‑OCT imagesThe AS-OCT images present a scale of dimensions defined by the equipment itself. The same investigator analyzed the images of each incision after exporting the images to the ImageJ software.
The evaluation of the architecture of the incisions included the incision length, endothelial gap, endothelial misalignment, and localized DMD. The characteristics described are considered indicators of sealing and healing quality.12-19
Length was measured by tracing a line from the point of entry of the incision into the epithelium to the point of penetration into the anterior chamber. The comparison of the final measurement with the initially planned architecture is another quality indicator, since the length of the incision influences intraocular manipulation20 and the risk of astigmatism.21
The endothelial gap is the apposition of the incisional edges of the posterior cornea13 and characterizes an incomplete sealing. The longer the length of the incision and the more inclined the angle of entry into the anterior chamber, the larger the size, and area of the endothelial gap.12 Another risk factor is low intraocular pressure.17,22
Endothelial misalignment is defined as a misalignment of the edges of the incision in the posterior cornea and may occur by a combination of limbal margin contraction and central tissue thickening,14 indicating incomplete remodeling.14 High intraocular pressure is significantly related to its presence, as well as stromal hydration.17
The main risk factors for localized DMD are as follows: advanced age, preexisting endothelial diseases, prolonged surgical time, hard cataracts, irregular corneal incisions and inadvertent trauma with blunt instruments or phacoemulsification probe, and incisional trauma.18 The longer the effective phacoemulsification time, the greater the risk of DMD.13
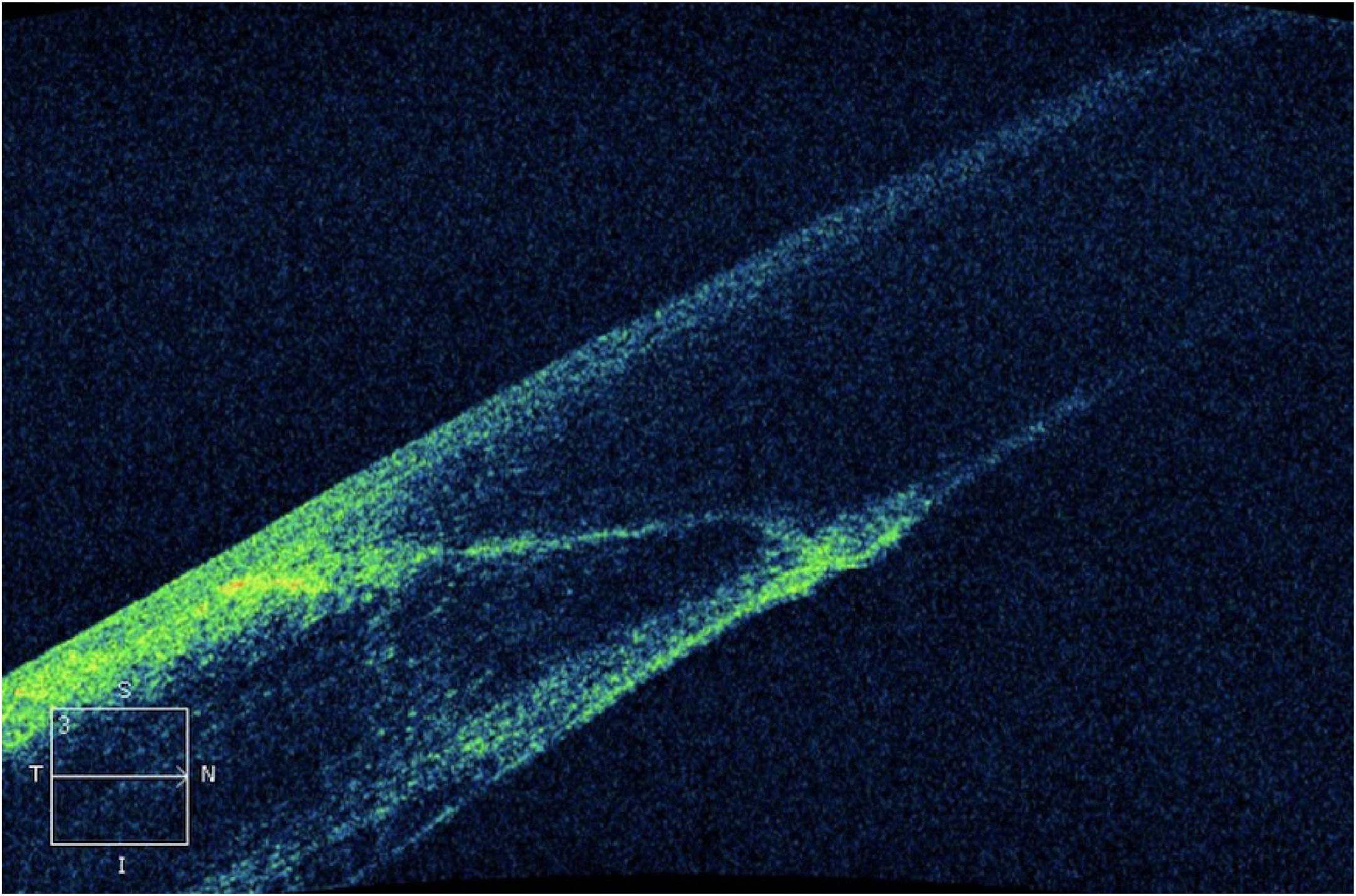
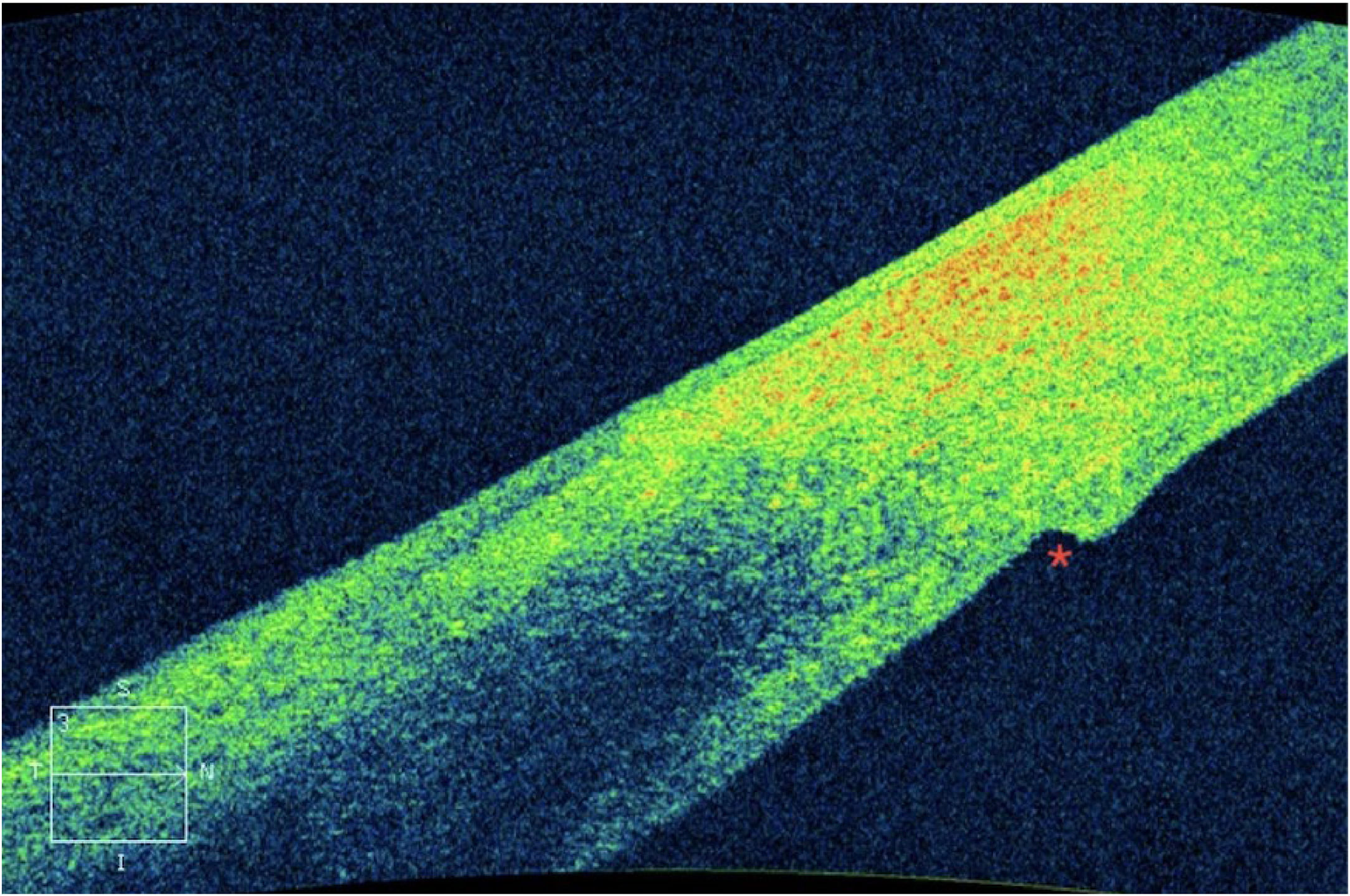
Fig. 1 shows an incision made with the femtolaser, and Fig. 2 an incision with a keratome blade. Figs. 3 and 4, and Supplemental Figure 1 illustrate the concepts of endothelial gap, endothelial misalignment, and DMD, respectively.
Statistical analysisDescriptive and exploratory data analyses were performed, and means, standard deviations, medians, and minimum, and maximum values were used for quantitative variables and absolute and relative frequencies for categorical variables. Next, the nonparametric Mann–Whitney test was used to compare the groups in relation to the time between surgery and examinations and the length of the incision. The chi-square and Fisher's exact tests were used to analyze the associations of the groups with the presence of endothelial gap, endothelial misalignment, and DMD. All analyses were performed with the aid of the R program, considering a significance level of 5 %.
R Core Team (2023). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
ResultsThe study included 37 eyes from 37 patients. Table 1 presents the results of the two groups, conventional phacoemulsification (Phaco group) and femtosecond laser-assisted phacoemulsification (Femto group), in relation to the characteristics of the participants and examinations. There was no significant difference between the groups regarding laterality, sex, and age of the patients (p > 0.05).
Results of the analysis of the sample characterization variables according to the group.
| Variable | Category | Groupa | p-value | |
|---|---|---|---|---|
| Phaco | Femto | |||
| n (%) | ||||
| Sample | ‒ | 19 (100.0 %) | 18 (100.0 %) | ‒ |
| Eye | Right | 12 (63.2 %) | 9 (50.0 %) | 0.4194b |
| Left | 7 (36.8 %) | 9 (50.0 %) | ||
| Sex | Female | 14 (73.7 %) | 11 (61.1 %) | 0.4142b |
| Male | 5 (26.3 %) | 7 (38.9 %) | ||
| Mean (standard deviation; minimum; maximum) | ||||
| Age (years) | ‒ | 70.6 (7.0; 58.0; 84.0) | 67.8 (7.6; 55.0; 81.0) | 0.2875c |
The mean length of the incisions was significantly higher in the Femto group than in the Phaco group (p < 0.05) (Table 2 and Supplemental Fig. 2). In the first examination, which was performed in the immediate postoperative period, the mean length of the incisions was 1.64 mm (range 1.35–1.96) in the Femto group and 1.43 mm (range 1.09–2.19) in the Phaco group. In the second examination, at 1 month postoperatively, the mean was 1.58 mm (range 1.27–2.14) in the Femto group and 1.27 mm (range 0.90–2.42) in the Phaco group. In all cases, the length of the incisions, manual, or automated, did not result in intraoperative technical difficulties or complications such as iris prolapse and incisional burn.
Mean (standard deviation) and median (minimum and maximum value) incision lengths (mm) as a function of the group.
Table 3 shows that there was no significant association of the type of surgery to which the participants of both groups were submitted, in relation to the presence of endothelial gap and the occurrence of endothelial misalignment (p > 0.05). The prevalence of endothelial gaps was 42.1 % and 61.1 % for the Phaco and Femto groups, respectively, in Exam 1, and 0.0 % in both groups in Exam 2. The occurrence rates of endothelial misalignment were 42.1 % and 27.8 % for the Phaco and Femto groups, respectively, in Exam 1, and 31.6 % and 5.6 % for the Phaco and Femto groups, respectively, in Exam 2. In Exam 1, the prevalence rate of DMD was significantly higher in the Phaco group (63.2 %) compared to that in the Femto group (22.2 %) (p < 0.05) (Fig. 1). In Exam 2, there was no significant association between the group regarding the presence of DMD (p > 0.05), and the prevalence rates were 10.5 % and 0.0 % in the Phaco and Femto groups, respectively.
Presence of complications: endothelial gap, endothelial misalignment, and Descemet Membrane Detachment (DMD) depending on the group.
| Examc | Variable | Groupa | p-value | |
|---|---|---|---|---|
| Phaco | Femto | |||
| n (%) | ||||
| Exam 1 | Endothelial gap | 8 (42.1 %) | 11 (61.1 %) | 0.2476b |
| Exam 2 | Endothelial gap | 0 (0.0 %) | 0 (0.0 %) | ‒ |
| Exam 1 | Endothelial misalignment | 8 (42.1 %) | 5 (27.8 %) | 0.3615b |
| Exam 2 | Endothelial misalignment | 6 (31.6 %) | 1 (5.6 %) | 0.0897c |
| Exam 1 | Descemet's membrane detachment | 12 (63.2 %) | 4 (22.2 %) | 0.0120b |
| Exam 2 | Descemet's membrane detachment | 2 (10.5 %) | 0 (0.0 %) | 0.4865c |
Clinical data were also measured in the postoperative period. Significant corneal edema was identified in three eyes in the Phaco group (15.7 %) and three eyes in the Femto group (16.6 %) in Exam 1 (between 2 and 4 days postoperatively). At 1 and 3 months after surgery, the mean best corrected visual acuity was 0.2 logMAR in both groups. The mean keratometry before (Kpre) and after surgery (Kpost) remained stable: Phaco group, Kpre = 42.22 and Kpost = 42.12, and Femto group, Kpre = 42.34 and Kpost = 42.22.
DiscussionThe corneal incision in cataract surgery has been widely studied in the literature and studies that evaluated postoperative results contributed to the understanding of the quality of the incisions. However, there is still no consensus that defines the ideal parameters for its construction.
Visibility23 and freedom of intraocular movements,12,20 complete self-sealing that prevents the flow of fluid through the incision24 and hypotonia,25 and refractive neutrality21,26,27 can be considered the main qualities of an adequate incision.
Incision length and architectureThere is no metric definition of a long or short incision in the literature. The presence of the following intraoperative challenges contributes to defining an excessively long incision: difficulty in the mobility of intraocular instruments, decreased visibility due to corneal striae and corneal hydration, and difficulty in the angle of access to cataracts.20 About the architecture, the incision is safer when it presents a tunnel with a valve mechanism to prevent the influx and reflux of fluid from the anterior chamber.24,28
Monica and Long demonstrated the safety and efficiency of 3-mm-wide and 2–3-mm-long self-sealing corneal incisions.29 Sonmez and Karaca evaluated 2.8-mm-wide rectangular incisions and concluded that there was a statistically greater risk of astigmatism in cases with a length of 1.5 mm than in cases with a length of 1.1 mm.21 Conversely, in 2023, Wilczynski et al. 26 found no significant difference in the risk of astigmatism between incisions with lengths of 1.4 mm, 1.8 mm, and 2.4 mm.
Ernest et al. evaluated that incisions with a quadrangular shape, that is, equal width and length, are more stable in preventing leaks after external pressure than rectangular incisions.30 Masket and Belani presented the safety of quadrangular self-sealing incisions of 2.2 mm and 3.0 mm in preventing leakage and hypotonia in the postoperative period.25
In the comparison between the incision models, Grewal et al. reported that the tri-planar architecture was found in only 19 % of the eyes with manual incisions and 100 % of the incisions with femtolaser procedure.9
Incision parameters and evaluationFrom the analysis of the data on the efficiency of both rectangular and quadrangular incisions, it is concluded that the planned incisions of 2.2 mm wide and 1.65 mm long, rectangular shape, triplanar with femtolaser, and biplanar with the keratome, used in the present study, present adequate quality parameters.
Stromal hydration at the end of surgery decreases the inflow of fluid into the anterior chamber after surgery.15 This technique generates greater local corneal edema13 in relation to cases in which hydration was not performed,16 and the change in thickness remains for up to 2 wk postoperatively. However, there is no significant difference in the cicatricial aspects of incisions with and without hydration.16 Between 5 and 9 wk after an unsutured corneal incision, a cellular reactivation occurs in the stroma, characterizing a final phase of healing.31
Therefore, the choice of technique with stromal hydration, along with scheduling the first AS-OCT examination for 2 to 4 days after surgery and the second examination for 1–3 months post-surgery, is appropriate for the analysis of the incisions.
The AS-OCT provides sensitive and detailed measurements of the incision in the clear cornea13 and has been widely used for these purposes in the literature. Supplemental Table 1 presents the results of other studies that evaluated the characteristics of tunnel length, endothelial gap, endothelial misalignment, and DMD of major incisions in cataract surgery by means of AS-OCT examinations. Most studies did not analyze the incisions after 1 month, and the authors found in the literature only 3 studies9,10,32 that evaluated automated incisions with femtolaser. Thus, the evaluation, in the medium term, of incisions 2.2 mm wide and 1.65 mm in length, with the femtolaser platform (LensX®, Alcon Laboratories, Inc.) is a novelty of the present study.
The analysis of the causes and consequences of complications of endothelial gap, endothelial misalignment, and DMD has been extensively addressed in other studies.
Endothelial gapCalladine and Packard suggested that a longer incision would be less affected by the loss of coaptation because the removal of the margins of the posterior cornea would represent a smaller percentage of the entire incision.17 Jin et al. reported a direct and significant relationship between incision length and angle of entry into the anterior chamber with increased endothelial gap area.12 The changes in keratometry and spherical equivalent were statistically greater in the cases with endothelial gap.12
Bacteria present in the tear can reach the aqueous humor if there is a gap of the inner side of the incision, without needing a complete gap of the incisional tunnel.14 In incisions with a 2.75-mm keratome blade, there was a significant increase in anterior corneal astigmatism in the group that presented endothelial gap, at the postoperative period of 1-wk and 1-month, but not after 3-months.12 Corneal thickening was statistically greater in patients with endothelial gaps than in patients without it.13 The functioning of the corneal endothelial pump could explain the improvement of this alteration over time, as demonstrated by the studies.12,14,16,33,34,35,36 Thus, an endothelial gap delays a patient's visual and refractive rehabilitation time.
Endothelial misalignmentEndothelial misalignment may be caused by the combination of hydration and edema of the incision roof16 with retraction of the posterior limbal margin. Wang et al. evaluated endothelial misalignment at 2–3 wk (33.3 %), 1–3-years (75 %), and 3 years (90.5 %) after surgery. The data showed that the prevalence of misalignment increased over the years.14 Its clinical effect is unknown, but it is supposed to induce changes in the anterior and posterior curvatures and, consequently, alter the power of the cornea and astigmatism.14
DMDIn cataract surgery, DMD can occur, supposedly, during the construction of the main incision or in the insertion of surgical instruments.17 Hypotonia is also correlated with its presence.17 DMD impedes the mechanism of the local endothelial pump, which hinders the complete sealing of the incisional wound and, consequently, increases the endothelial gap, and thickening of the cornea at the incision site, leading to slower visual recovery.18,19
Femtolaser corneal incisionsA study by Chaves et al. found no significant difference between the intended length and that achieved by femtolaser in 1.8-mm tunnel incisions. The authors evaluated the incisions immediately after femtolaser (18 % gap and 0 % DMD) and immediately after completing surgery (91 % gap and 45 % DMD). The results suggest that endothelial gap and DMD are more related to intraoperative manipulation than to laser energy.10
Grewal et al. found that endothelial misalignment and DMD were significantly less prevalent in femtolaser-generated incisions than in manual incisions.9 The mean length of femtolaser incisions was 1.99 mm (1.86–2.13), which represents 94.9 % of the intended 2.1 mm9 and is in line with the result of the current study (95.7 %).
In the present study, two characteristics related to the quality and precision of the incisions were statistically favorable to the femtolaser technique: mean incision length in both exams and lower prevalence of DMD in Exam 1. Conversely, one hypothesis for the higher prevalence rate, although not significant, of an endothelial gap in the Femto group in Exam 1, is the longer mean incision length. There was a higher, albeit not significant, prevalence of endothelial misalignment in the Phaco group, which might be related to the need for more vigorous stromal hydration in this group.
The observation of the cases during the postoperative period suggests that the eyes with DMD presented slower visual recovery, which would constitute a clinical advantage to the use of femtolaser. However, there were no intraoperative complications related to the alterations, and the final visual acuity was similar between the groups. Both surgical techniques showed safe results. Thus, the authors conclude that, although, when submitted to microscopic evaluation, the quality of the incisions may vary according to the technique used, further clinical analysis is still required.
Studies on corneal incisions include different equipment, parameters, and surgical techniques used in both femtolaser and conventional phacoemulsification, as well as diversity in tunnel architecture planning. The advancement of studies on the subject is necessary so that new data help define the currently vague concept of ideal incision.
Ethical approvalThe study was approved by the ethics committee of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, and all patients provided informed consent to participate in the study, following the guidelines established in the Declaration of Helsinki.
FundingNone.